On this page
What Is a Nebuliser and How It Works
A nebuliser (also spelled nebulizer) is a small machine that turns liquid asthma medicine into a fine mist you breathe into your lungs.
It has a medicine cup, a mouthpiece or face mask, tubing, and a power source (a compressor or a quiet mesh unit). You sit upright and breathe normally while the mist flows.
A breathing treatment usually takes about 5–10 minutes to finish.
A nebulizer is not a humidifier or steamer. It delivers medicine, not plain water vapor.
Bottom line: A nebulizer is a machine that turns liquid medicine into a mist you breathe in.
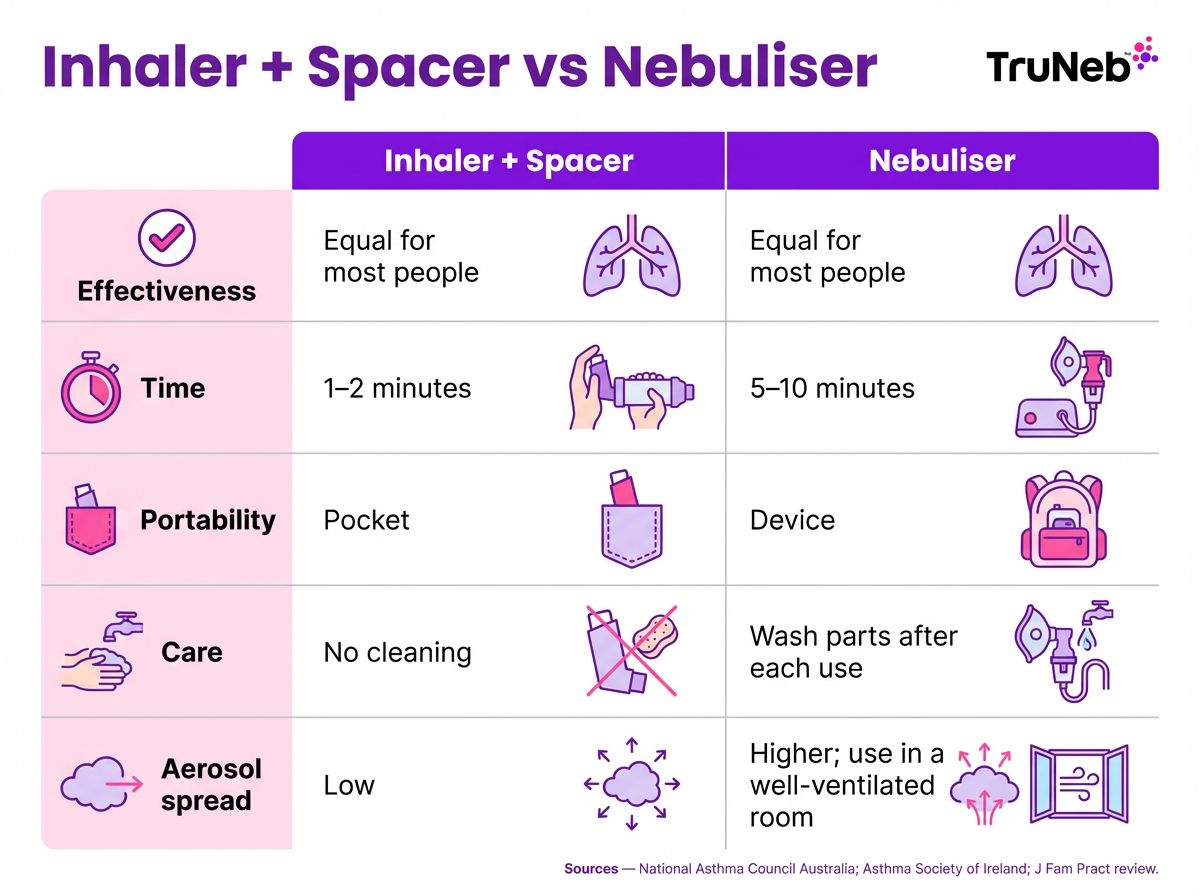
Nebulizer vs Inhaler: Which Is Better for Asthma Relief
For most people with asthma, a puffer (metered-dose inhaler) with a spacer is the first choice for treating symptoms and flare-ups. Research and asthma guidelines back this up, and people usually have fewer side effects with the inhaler-and-spacer option.
Why inhaler + spacer usually wins:
- Fast: medicine in seconds instead of minutes.
- Portable: pocket size.
- Simple care: no cup or mask to wash after each use.
- Usually lower cost.
Limits of a nebulizer when you don’t need one:
- Takes longer (about 5–10 minutes per dose).
- Needs power and regular cleaning.
- Can spread aerosol in the room.
Because the mist can hang in the air, it’s best to use a nebulizer in a well-ventilated space, especially around other people.
- Parts need replacing over time.
Exception: In a severe attack or if you cannot use an inhaler well, a nebulizer may be used under medical advice.
Key point: A nebulizer isn’t stronger medicine; it’s just another way to deliver the same medicine.
| Feature | Inhaler + spacer | Nebuliser |
|---|---|---|
| Effectiveness | Equal for most people | Equal for most people |
| Treatment time | 1–2 minutes | 5–10 minutes |
| Portability | Pocket-sized | Device with power source |
| Cleaning | No washing after use | Wash cup and mask/mouthpiece |
| Aerosol spread | Low | Higher; use in a well-ventilated room |
| Cost | Usually lower | Device + parts over time |
Note: Your doctor will advise which option fits your situation.
Bottom line: Inhalers with a spacer work as effectively as nebulizers for most asthma care.
When Is a Nebulizer Needed for Asthma
You usually need a nebulizer only in specific situations.
Severe asthma attack (emergency use)
In ambulances or the ER, clinicians sometimes use a nebulizer to deliver continuous rescue medicine when breathing is very hard. Follow your Asthma Action Plan. If you are not improving, call 911 or 999.
Babies and young children
If a child can’t use an inhaler and spacer correctly yet, a nebulizer with a face mask lets them breathe normally while getting medicine.
People who struggle with inhalers
If arthritis, a stroke, or coordination issues make inhalers hard to use (even with a spacer), a nebulizer can help you get the full dose.
Severe or uncontrolled asthma at home
Some people have a home nebulizer as part of a specialist’s plan. Home nebulizer use for children should be started and managed only by specialists. Don’t buy or start a home nebulizer on your own—your asthma specialist should decide if you need one and show you how to use it safely.
Other lung conditions
People with bronchiectasis, cystic fibrosis, or sometimes COPD and pulmonary fibrosis inhale sterile hypertonic saline (3% or 7%) or other medicines by nebulizer to loosen mucus. TruNeb™ 3% and 7% Hypertonic Saline are examples of sterile saline solutions used for mucus-clearance needs when prescribed by a doctor. This is not routine asthma care.
If you’re not sure whether you need a nebulizer, check in with your doctor or asthma nurse.
Bottom line: Nebulizers are for special cases - severe attacks, little kids, or when you can’t use an inhaler well.
What Medications Are Used in a Nebulizer
Nebulizers use liquid forms of the same drugs you get by inhaler. These come in pre-measured vials (nebules).
- Relievers (short-acting beta-agonists): Albuterol (salbutamol) opens the airways fast during symptoms.
- Anticholinergics: Doctors sometimes add ipratropium in bad flare-ups.
- Steroids: Budesonide (respules) is used daily in some children or in people who can’t use inhaler steroids well.
- Saline: Sterile hypertonic saline (3% or 7%) helps loosen thick mucus in conditions like bronchiectasis or cystic fibrosis. It’s not routine asthma treatment.
Some people with chronic lung infections also use nebulised antibiotics, but this is specialist care and not part of routine asthma treatment.
Only use medicines prescribed for nebulizing. Do not put oils, homemade mixtures, or crushed pills into a nebulizer—putting other substances in the cup can damage your lungs or the device.
Your doctor will decide which medicines belong in your nebulizer and how often to use them—don’t change the dose or schedule on your own.
Bottom line: Only use liquid asthma medicines that were prescribed for nebulizer use—never put other substances in the cup.
How to Use a Nebulizer at Home Step-by-Step
Always follow your nebulizer's instruction manual too - different brands can have small differences in setup and cleaning.
- Wash your hands well.
- Set up the device: attach tubing; have the clean cup and mask or mouthpiece ready; charge a portable unit if you use one.
- Add the prescribed medicine to the cup. Check the vial and do not mix or dilute unless instructed.
- Assemble and sit upright. Put on the mask snugly or seal your lips around the mouthpiece.
- Turn it on and breathe slowly through your mouth. Pause if you cough; resume when ready.
- Continue until the mist slows and the cup sputters. Keep the cup upright. Most treatments take about 5–10 minutes.
- Turn off and remove the mask or mouthpiece.
- If you used a steroid, rinse your mouth and gargle; spit out. If you wore a mask, wash your face.
- Clean the parts (cup, mask/mouthpiece) after each use so they’re dry and ready next time.
Tips: Use the device on a flat, hard surface with the vents clear. Try to sit in a well-ventilated room, especially if other people are nearby.
How Often to Use a Nebulizer for Asthma
Use your nebulizer only as your doctor prescribes and as written in your Asthma Action Plan. This section gives general guidance only; your doctor will set the exact dose and timing for your treatments. Most people use it only when symptoms flare. If you feel you need treatments very frequently or close together, that’s a red flag—call your doctor. If a severe attack is not improving after one treatment at home, seek emergency care instead of repeating treatments over and over at home.
Bottom line: At home, you set up your nebulizer, add the prescribed medicine, breathe normally for about 10 minutes, then clean the parts.

Cleaning and Maintaining Your Nebuliser
Proper cleaning keeps you safe and helps the device work right.
Dirty nebulizers can grow bacteria and raise your risk of chest infections, so regular cleaning is essential.
Source: Asthma + Lung UK
After every use:
- Turn off and unplug.
- Take apart the cup and mask/mouthpiece (do not wash tubing or the motor).
- Wash cup and mask/mouthpiece in warm soapy water. Rinse well.
- Shake off water and air-dry completely on a clean towel. Do not towel-dry by hand.
Weekly (or as the manual says): disinfect parts as directed. Some models have parts that are dishwasher-safe; follow your device instructions.
Filters and parts: Check the filter (if present) and replace on schedule. Replace cups, masks, and tubing regularly based on use—often every 3–6 months, or as your manual suggests.
Storage: Keep parts clean, dry, and covered. Have a spare set so one can dry while the other is ready.
Bottom line: Clean after every use and replace parts on schedule to keep doses safe and effective.
Nebulizer Safety Tips and Side Effects
Safety note: Talk to your doctor before trying a new medication.
Do:
- Use only the medicines and doses your doctor (or asthma nurse) prescribed.
- Supervise children during every treatment.
- Keep the machine on a flat, hard surface with vents clear. Use in a well-ventilated area.
- Have your technique and device checked at clinic visits.
Do not:
- Delay emergency care. If a severe attack isn’t improving, call 911 or 999.
- Share masks or mouthpieces.
- Cover air vents or use the device near smoke or heavy dust.
- ⚠️ Don’t rely on repeated home nebulizer treatments if your breathing is getting worse. If you’re struggling to breathe, can’t speak in full sentences, feel faint, or notice blue lips or face, call 911 or 999 right away.
Common side effects (usually temporary):
- Shaky hands or a racing heart (common with albuterol/salbutamol).
- Dry mouth or throat irritation.
- Headache or lightheadedness.
- Facial rash or oral thrush after steroid nebulizer treatments (rinse mouth and wash face).
- Eye irritation with ipratropium if mist gets into the eyes (keep mask snug and protect eyes).
This isn’t a full list of side effects—always read the leaflet that comes with your medicine and talk to your doctor if anything worries you.
If you notice new or severe side effects during or after a nebulizer treatment, stop the treatment and speak with a doctor right away.
Travel tip: Pack your nebulizer, meds, charger or batteries, and cleaning supplies. Carry it in hand luggage and bring the right power adapter. A small, battery-powered nebulizer is easiest to pack for trips. Ask your airline about in-flight use.
Bottom line: If a nebulizer treatment isn’t helping fast, seek emergency care - don’t wait.
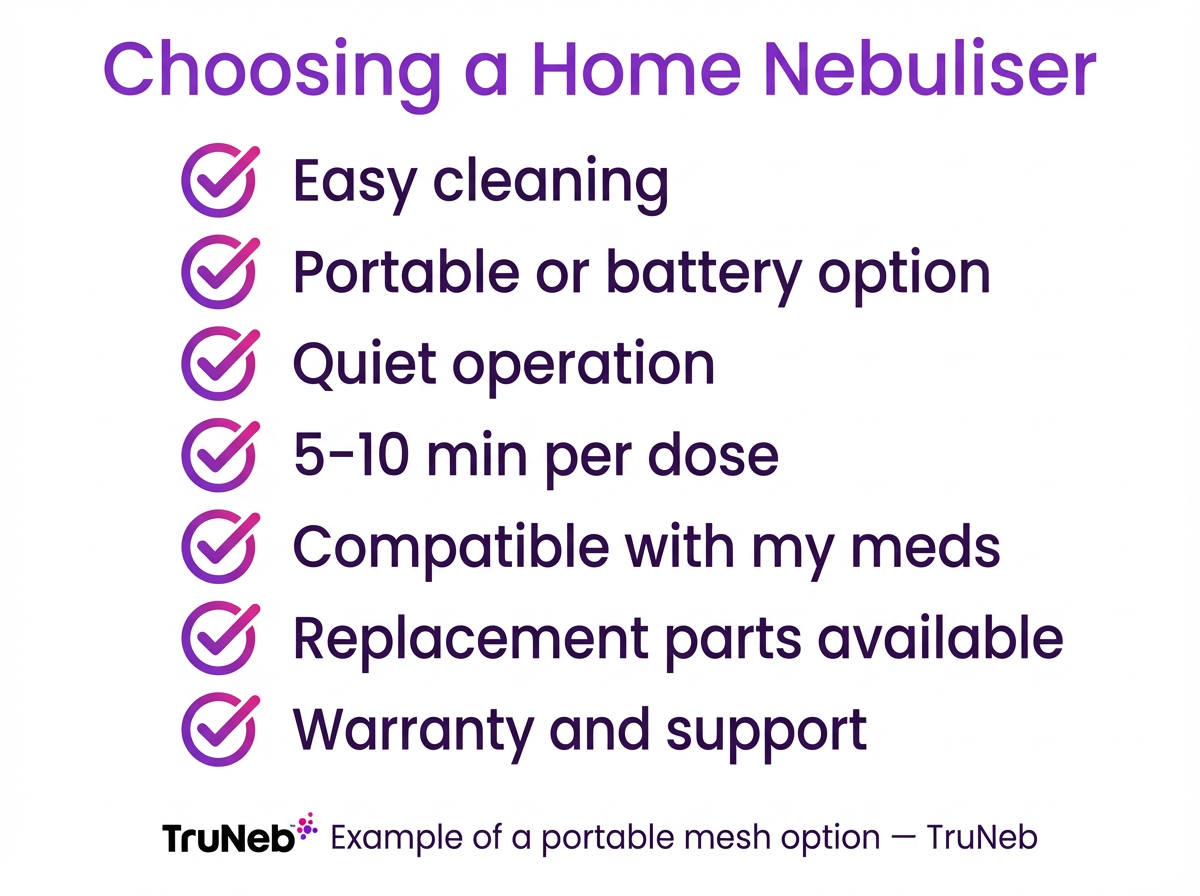
Choosing the Right Nebulizer for Home Use
If your doctor advises a home nebulizer, compare these points:
- Ease of use and cleaning: Fewer parts and simple cleaning save time.
- Portability: Will you travel or use it at school or work? Pocket-size mesh models are easy to carry.
- Power: Wall plug, rechargeable battery, USB, or car adapter.
- Noise: Compressors can be loud; mesh and ultrasonic models are quieter.
- Treatment time and specs: Aim for a device that delivers a dose in about 5–10 minutes and is compatible with your medicines.
- Parts and support: Make sure masks, cups, and filters are easy to buy. A clear warranty and helpful support matter.
- Safety and approvals: Check that the nebulizer is from a reputable company and meets local safety standards (such as FDA-registered or CE-marked).
Example: TruNeb™ Portable Mesh Nebulizer is handheld, quiet, and battery-powered, which can make daily and travel use simpler. Use any device only as your doctor recommends.
Bottom line: Pick a nebulizer that’s easy to clean, quiet, portable, and compatible with your meds.
Frequently Asked Questions
These quick answers cover common questions about when nebulisers are needed, how they compare with inhalers, and how to use them safely. Tap or click a question below to see the answer:
Most likely not. If your inhaler with a spacer works well, you usually don’t need a nebuliser. Asthma guidelines say inhalers are equally effective for most people. Ask your doctor if you’re not sure.
For most people, an inhaler with a spacer is just as good as a nebuliser—and faster and easier to carry. A nebuliser isn’t stronger; it’s simply a different way to deliver the same medicines.
It can, especially in a severe attack under medical care. If a home nebuliser is part of your action plan, use it as directed. If symptoms don’t improve quickly, call 911 or 999.
Yes. Nebulisers are commonly used for babies and young children who can’t use an inhaler and spacer yet. As kids learn good technique, they usually switch to inhaler + spacer because it’s faster.
Use it only as prescribed. Frequent need is a sign your asthma isn’t controlled. Call your doctor if you need repeated treatments close together or if you’re not improving.
You can usually buy a nebuliser device without a prescription, but the medicines are usually prescription-only. Don’t start nebuliser treatments without your doctor’s guidance.
Bottom line: Most people with asthma do well with an inhaler and spacer, and nebulizers are reserved for special situations that your doctor will explain.
In short, an inhaler with a spacer is enough for most day-to-day asthma care. Nebulizers are useful in specific situations and should fit into your Asthma Action Plan. Keep your device clean, follow your doctor’s instructions, and seek urgent care if symptoms are not improving.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, medications, and any questions you have about using a nebulizer.







