On this page
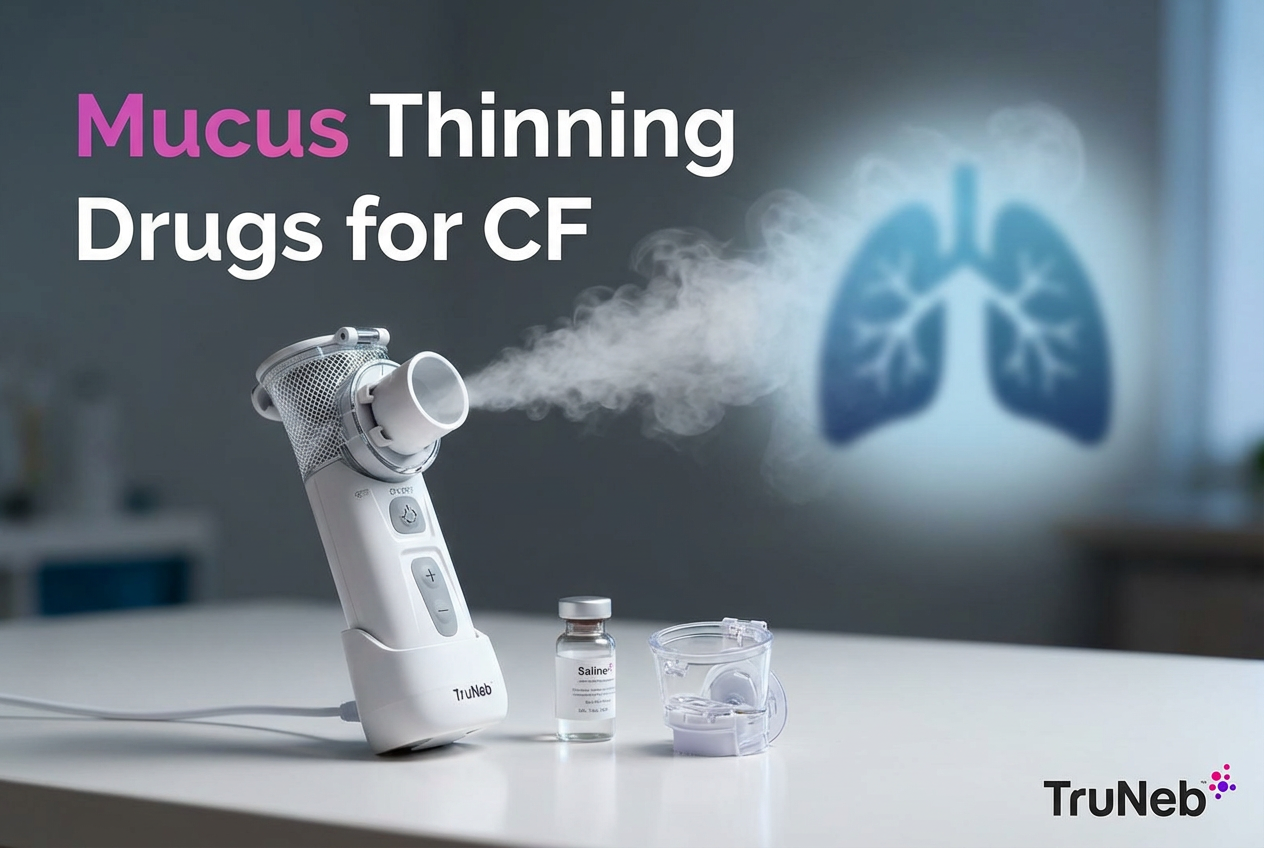
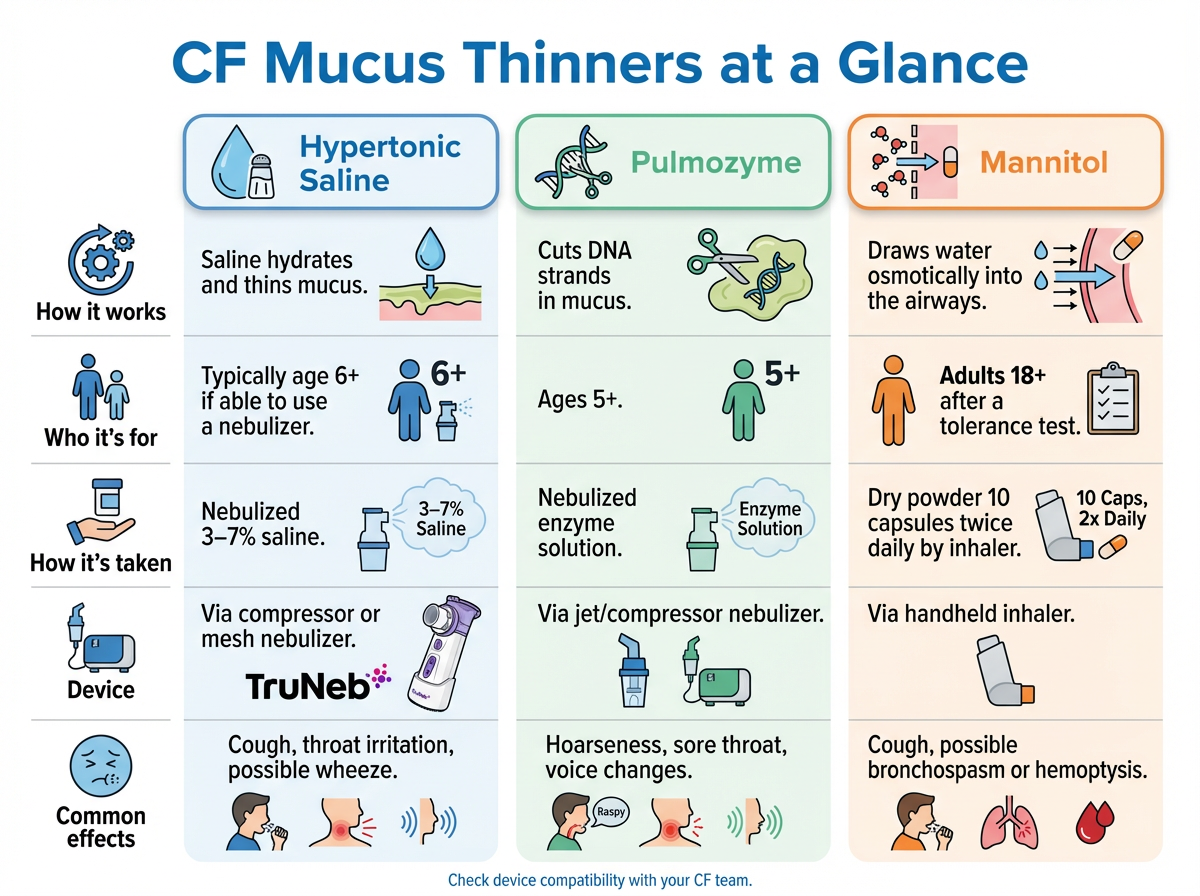
Inhaled Mannitol Powder – An Additional Option for Adults
Inhaled mannitol, sold as Bronchitol, is a dry powder you breathe in to thin and clear thick CF mucus. It acts as an osmotic agent, drawing water into the airways so mucus loosens and is easier to cough out. The exact action isn’t fully known, but the aim is the same as saline: easier clearance.
Who Uses It
For adults 18 and older. Before starting, you'll do a supervised Bronchitol tolerance (challenge) test in clinic to be sure your airways don’t tighten.
How It’s Taken
- Capsules of powder with the provided inhaler.
- Prescribing information typically calls for a total of 10 capsules twice a day, but your CF team will decide the exact dose and schedule for you.
- People usually inhale each capsule one after another. Airway clearance is often scheduled soon afterward because the mucus-thinning effect is short-lived; your clinic will tell you how to time it.
What to Expect
Some adults see better mucus clearance and lung function. Some studies haven’t found clear added benefit when it’s layered on top of Pulmozyme, so teams usually consider mannitol when saline or Pulmozyme aren’t tolerated.
Side Effects
- Very common: coughing.
- Others: throat irritation, headache, nausea.
- Possible reactions: bronchospasm or coughing up blood (hemoptysis). Clinics sometimes recommend using a bronchodilator before mannitol to reduce airway tightness; your CF team will let you know if that’s right for you.
⚠️ If you develop sudden trouble breathing, severe chest tightness, or cough up more than small streaks of blood, contact your CF team immediately or seek emergency care.
Bronchitol has FDA approval for adults with CF in the U.S. (2020) and is also used in regions such as Europe and Australia. Coverage and access can vary by insurance plan and CF center.
Note: Talk to your doctor before trying a new medication.
Quick take: Bronchitol is an adult-only inhaled powder that draws water into the airways to thin CF mucus. It is started only after a clinic tolerance test, and it is one more option in the toolbox for adult CF care when your team thinks it fits your overall plan.
Using Mucus Thinners in Your CF Care Routine
Mucus thinners work best as part of a bigger plan. They’re teamed with bronchodilators, airway clearance techniques, antibiotics when needed, and CFTR modulators. Your CF team will tailor the mix to you.
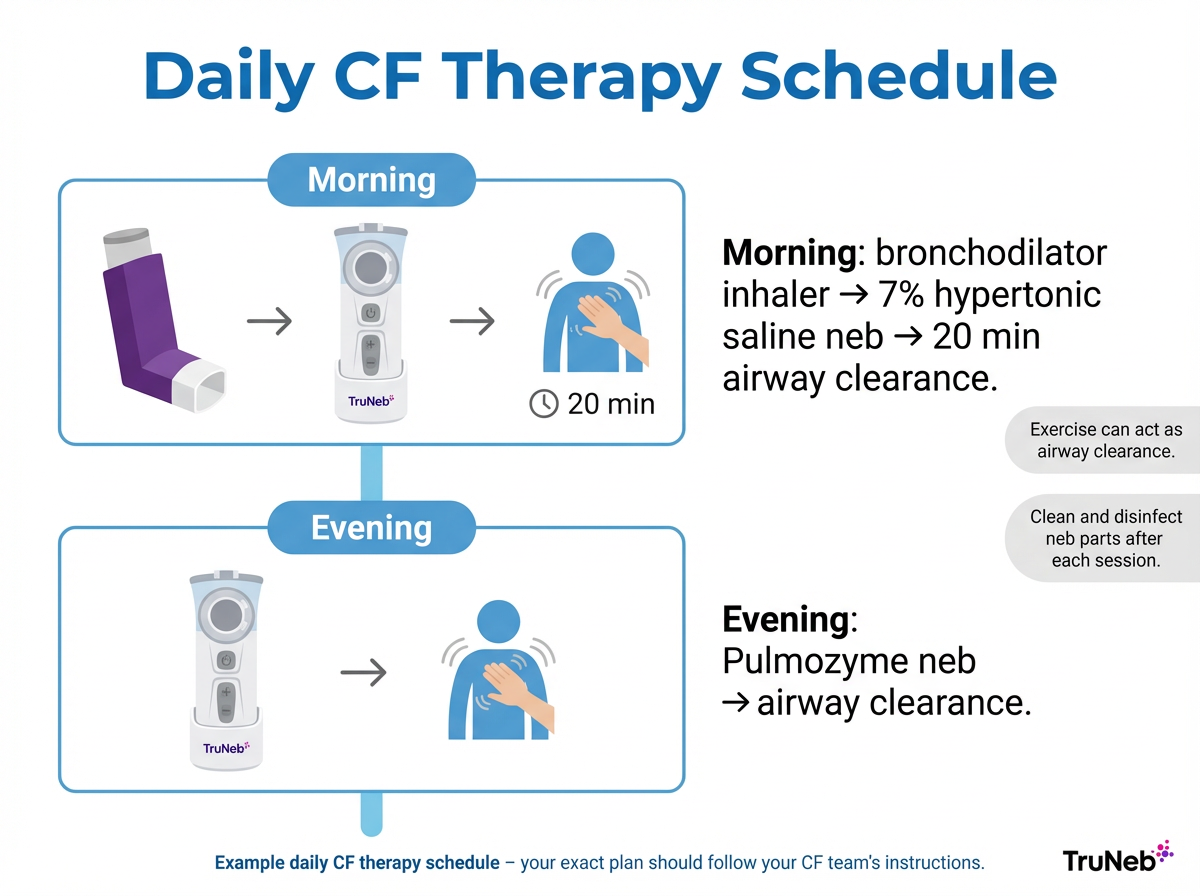
A simple daily rhythm
Here’s an example of how a CF team might organize a day (your schedule may look different):
- Morning: a bronchodilator inhaler → 7% hypertonic saline by nebulizer → about 20 minutes of chest physiotherapy (vest or percussion) to move out loosened mucus, as your team recommends.
- Evening: dornase alfa (Pulmozyme) with its recommended jet/compressor nebulizer → airway clearance again. Some care teams time saline before exercise so coughing helps clear mucus. Ask your CF team if that makes sense for your plan.
Sticking with it
- It helps to set steady times, use phone reminders or a simple checklist, and keep your neb parts clean and ready so it’s easy to get started.
At clinic visits, your CF team checks lung function tests like FEV1, reviews how your treatments are working, and may adjust saline concentration, add bronchodilators, or change timing. If mucus is getting thicker or infections flare, they may order sputum cultures. Staying consistent with mucus thinners and airway clearance can help reduce flare-ups and make day-to-day breathing easier.
Nebulizer devices matter
- Good equipment helps medicine reach your lungs. Portable mesh nebulizers are quiet and battery powered. That can make it easier to keep up with saline or bronchodilator doses on busy days. A portable nebulizer like TruNeb™ is one example that can make treatments simpler on the go.
- Device fit is medication-specific. Use a compressor jet system for Pulmozyme as recommended by its instructions. Ask your CF team which device to use for each medication.
Safety and cleaning
- Guidelines recommend cleaning and disinfecting all nebulizer parts after each use to prevent germs. This step protects your lungs as much as the medicine does.
⚠️ If you ever feel sudden severe shortness of breath, chest pain, or notice blue lips or fingertips during treatments, call emergency services right away.
Tip: If your CF team approves, consider a compact mesh nebulizer for travel or school. You can also get sterile hypertonic saline vials delivered to your home. If you’re using insurance, your plan usually requires a prescription from your doctor. Off-the-shelf saline from suppliers (including TruNeb) can sometimes be bought without using insurance, but always follow your doctor’s guidance on which solution to use.
Important: Always talk to your doctor before changing dose timing, adding over-the-counter remedies, or switching devices.
Quick take: Build a repeatable morning-and-evening routine and match each medication to the right nebulizer for best results.
FAQs – Cystic Fibrosis Mucus Thinners
This FAQ answers common questions about CF mucus thinners, including how they work, when they’re started, and how they fit with other treatments. Tap or click a question below to see the answer:
The main mucus thinners are hypertonic saline and dornase alfa (Pulmozyme). Some adults also use inhaled mannitol powder (Bronchitol) after a clinic tolerance test. These treatments help make sticky mucus thinner and easier to cough out.
Hypertonic saline hydrates and thins mucus by drawing water into the airways. Pulmozyme is an enzyme that cuts apart DNA in the mucus to break it up. A lot of people use both for a combined effect.
CFTR modulators improve how the CFTR protein works, but they don’t replace airway clearance or mucus thinners for most people. Most patients stay on saline and/or Pulmozyme unless their CF specialist changes the plan. Never stop or cut back on mucus thinners without your CF specialist’s guidance.
Doctors typically start hypertonic saline around age 6 (sometimes earlier if a child can manage a neb). Pulmozyme is approved for ages 5 and up. Your CF team will guide timing based on readiness.
For infants and toddlers, airway clearance techniques like percussion and positioning do most of the work. Mucus thinners are usually added when a child can cooperate with nebulizers. Follow your pediatric CF specialist’s plan.
Your doctor might prescribe a bronchodilator before saline to reduce wheeze. Some people start with 3% saline and later move up to 7% under their clinic’s guidance so their airways can adjust. If you have severe coughing, wheezing, or tightness that doesn’t improve, contact your CF clinic right away.
Use the device your team recommends for each drug. Hypertonic saline works with most compressors or mesh nebs—including portable options like TruNeb for on-the-go use. Pulmozyme should be used with a specified jet/compressor system. Always confirm with your clinic.
No. Steam inhalers you see in stores aren’t the same as nebulizers and shouldn’t be used for prescription CF medications. Use the device your clinic recommends for each medication.
Studies so far suggest these treatments are generally safe to use long-term when prescribed by your CF team. Letting thick mucus build up can damage the lungs, which is why your team usually recommends regular mucus thinners. They’ll monitor you and adjust the plan if any side effects or concerns come up.
OTC expectorants haven’t been shown to help much with CF’s thick mucus. CF-specific inhaled therapies generally work better for most people. Always check with your CF doctor before adding any over-the-counter product.
Disclaimer: This information is for educational purposes only and is not a substitute for professional medical advice. Always talk to your CF doctor or care team about your treatments.