On this page
What is a mucus plug in the lungs?
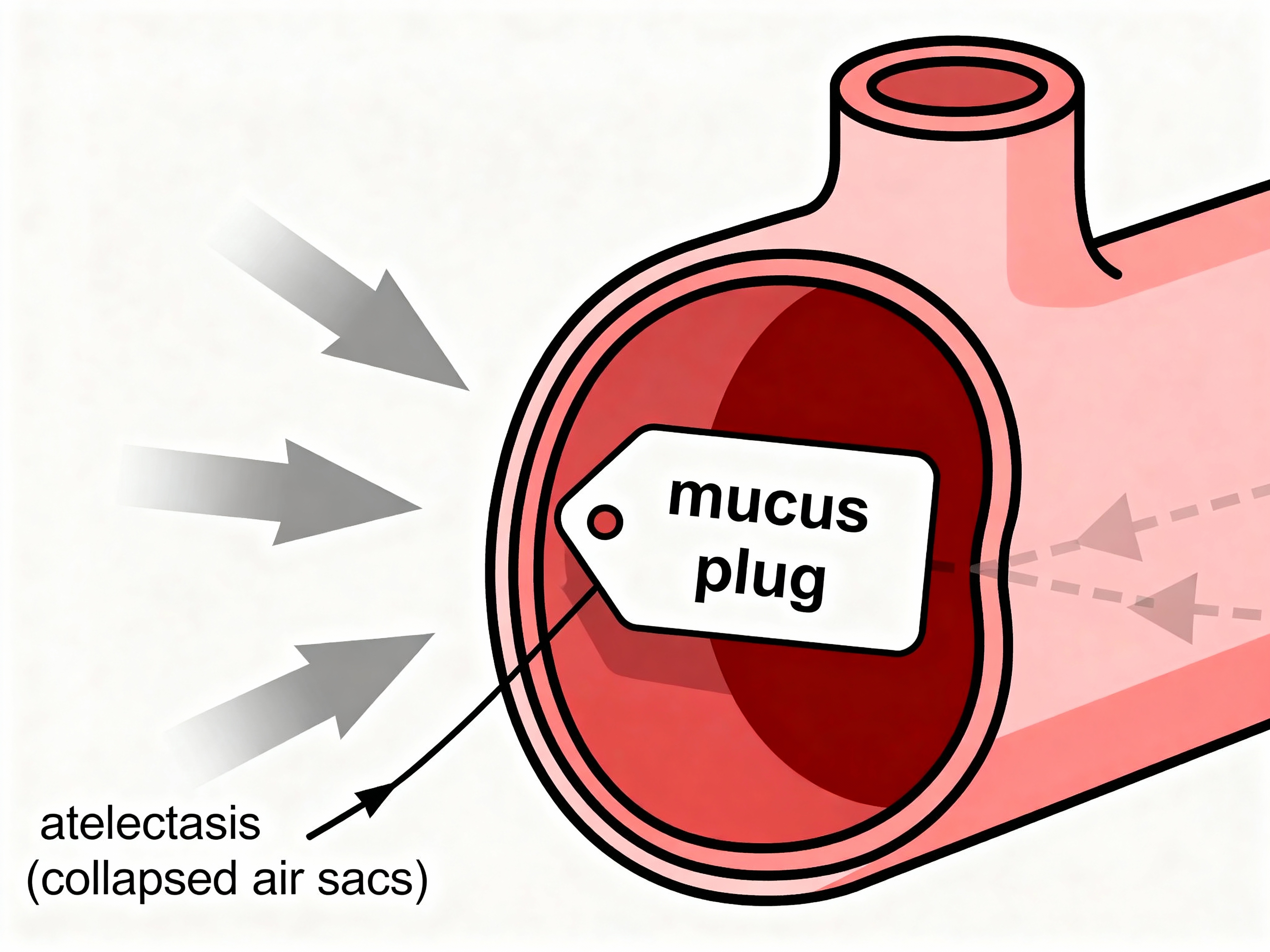
A mucus plug is a thick clump of sputum (phlegm) that blocks an airway so air can’t get through. Think of it like a clog in a pipe. Air can’t reach the tiny air sacs (alveoli), and the area behind the plug can partly collapse (atelectasis). In medical terms, this is an airway obstruction. Normal mucus protects your lungs; a plug is thick and stuck.
Key point: A mucus plug is a thick mucus blockage that obstructs an airway and can cause part of the lung to collapse (atelectasis).
What causes mucus plugs in the lungs?
Mucus plugs form when your lungs make more mucus than usual, the mucus gets too thick, or your cough can’t move it. This mucus plugging happens when secretions thicken or your cough is too weak to move them. Common causes include:
- Chronic lung diseases: Asthma, COPD (chronic bronchitis and emphysema), bronchiectasis, and cystic fibrosis can lead to extra, thicker mucus that’s hard to clear.
- Infections: Pneumonia or bad viral bronchitis can pack small airways with phlegm, especially during flare-ups.
- After surgery or hospital stays: General anesthesia, pain, and bed rest can lead to shallow breaths and weak coughs. Mucus builds up and can plug airways.
- Weak cough or neuromuscular conditions: ALS or spinal cord injury can weaken cough strength, so mucus sits and dries into a plug.
- Dehydration and dry air: Not enough fluids or dry airways make mucus thicker and stickier.
- Smoking and irritants: Smoke harms the cilia (tiny hairs) that move mucus, and it triggers more mucus production.
- Less common causes: Allergic bronchopulmonary aspergillosis (ABPA), plastic bronchitis, and pulmonary alveolar proteinosis can produce unusually thick mucus that plugs airways.
Rule of thumb: Anything that thickens mucus or weakens your cough can set the stage for a plug.
Signs and symptoms of a mucus plug
Symptoms can be sudden or subtle, depending on the plug’s size and location.
- Cough that won’t clear
- Shortness of breath or chest tightness
- Wheezing or whistling sounds
- Choking sensation or trouble taking a deep breath
- Chest congestion or a heavy feeling in the chest
- Rapid, shallow breathing and anxiety
- Sometimes there are few clear signs if a small airway is blocked, but you can feel more winded than usual
Sputum color can change with infections, but color alone doesn’t diagnose infection—see your doctor if you’re concerned.
Quick check: A sudden “blocked” feeling you can’t clear—plus breathlessness or wheeze—points to a mucus plug.
Why mucus plugs can be dangerous
Most mucus plugs can be cleared. But if a plug sits too long or fully blocks a large airway, it can cause problems.
- Airway blockage and atelectasis: The lung segment beyond the plug can collapse, cutting down oxygen exchange.
- Low oxygen levels (hypoxemia): You can feel dizzy, confused, or very short of breath.
- Infection risk: Trapped mucus can lead to pneumonia behind the blockage.
- Worse outcomes in COPD: In studies, COPD patients with mucus plugs seen on CT scans had faster lung function decline and higher long-term mortality.
- Emergency risk (rare): A big plug high in the airway can cause severe distress and needs urgent care.
Bottom line: Don’t ignore persistent plugs—clearing them protects your breathing and lowers infection risk.
How doctors diagnose a mucus plug
- Exam: Your doctor listens for wheeze or reduced breath sounds on one side.
- Chest X-ray: Can show a collapsed lobe or an area that looks plugged (usually indirectly).
- Chest CT scan: Shows plugs more clearly and where they sit in the airway.
- Bronchoscopy: A thin scope looks inside the airways. Doctors can see the plug and often suction it out.
Simple rule: If symptoms are severe or not improving, imaging or bronchoscopy is sometimes needed to find and remove the plug.
Effective ways to clear a mucus plug from your lungs
People use a mix of techniques to clear plugs. Combining methods usually works best. Ask your doctor which approach fits your situation.
- Controlled coughing (deep or huff cough): A respiratory therapist can teach controlled and huff coughing to move mucus higher so it’s easier to clear.
- Postural drainage: Using gravity positions to drain lung segments; a doctor or respiratory therapist can show safe positions.
- Hydration and warm steam: Drink water, tea, or broth. Warm showers or humidified air can loosen thick mucus so it moves.
Heads up: Steam inhalers are not nebulizers and aren’t used to deliver prescription breathing medicines.
- Chest physiotherapy (percussion): Gentle clapping on the chest/back over the affected area or a high-frequency chest vest helps shake mucus loose.
- Airway clearance devices: Positive expiratory pressure (PEP) devices (like flutter-style valves) create back pressure and vibrations to move phlegm.
- Medicines that help mucus move: Bronchodilators open airways; expectorants like guaifenesin can thin secretions; prescribed mucolytics, including nebulized saline or N-acetylcysteine, can break up thick mucus. In some conditions, doctors prescribe hypertonic saline.
- Cough-assist device (mechanical insufflation–exsufflation): If your cough is weak (for example with ALS or spinal cord injury), a cough-assist device can help—ask your doctor if it’s appropriate.
- Suctioning: If you have a trach or a very weak cough, trained caregivers can suction mucus from the mouth or trach.
- Bronchoscopy (hospital): For a stuck or severe plug, doctors can see it and remove it with a scope.
A portable mesh nebulizer can deliver saline or prescribed medicines as a fine mist, which can help loosen thick mucus before you cough.
If you can’t breathe well, have chest pain, or your lips look bluish, seek emergency care.
Most people clear a mucus plug by layering techniques: open the airways, loosen the mucus, then cough it out.
Clearing mucus plugs when you have COPD
- Stick with your daily plan: Inhalers as prescribed, then huff coughing, then a PEP device if you have one, can make clearance easier.
- Add movement: Gentle activity and pulmonary rehab exercises can strengthen your cough.
- Act early: If you feel more blocked than usual, start your clearance routine right away and stay hydrated.
COPD tip: Small daily steps to move mucus can help prevent bigger plugs and flare-ups.
| Method | How it helps | When to use |
|---|---|---|
| Controlled/huff cough | Moves mucus higher so it’s easier to clear | First step for most plugs |
| Postural drainage | Gravity helps drain lung segments | After inhalers or humidified air |
| Hydration + humidified air | Thins and loosens mucus | All day, especially during colds |
| Chest percussion/vest | Vibrates mucus loose from airway walls | Chronic mucus or hard-to-move plugs |
| PEP device (flutter-style) | Back pressure opens small airways and vibrates mucus | Daily COPD/bronchiectasis care |
| Nebulized saline or mucolytic (incl. hypertonic saline) | Moistens or breaks thick mucus | When mucus feels sticky and dry |
| Bronchodilator (inhaler) | Opens tight airways so mucus can move | Before cough/clearance sessions |
| Cough-assist device (MI–E) | Simulates a strong cough to clear secretions | Weak cough (e.g., ALS, spinal cord injury) |
| Suctioning | Physically removes mucus | Weak cough, trach, or severe distress |
| Bronchoscopy | Directly locates and removes a plug | Hospital care for stuck plugs |
Note: Check with a clinician before starting new devices or mucolytics; some require a prescription or training.
How to prevent mucus plugs
- Drink water through the day: Keeps mucus from getting sticky and thick.
- Don’t smoke and avoid irritants: This helps your cilia work and lowers mucus production.
- Daily airway routine: Breathing exercises, gentle postural drainage, or a PEP device morning and night can help keep mucus moving.
- Stay active and change positions: Moving helps mobilize mucus. After surgery, use your incentive spirometer as directed.
- Use humidity if your doctor recommends it: A room humidifier or appropriate humidification with oxygen or a trach helps keep airways moist.
- Keep vaccines up to date: Flu, COVID, and pneumococcal shots lower infection risk.
Simple habit: Hydration plus a short daily clearance routine can prevent most plugs.
⚠️ If you have severe trouble breathing, chest pain, bluish lips, confusion, or symptoms that don’t improve, call emergency services now. Talk to your doctor before trying a new medication or changing your inhaler or nebulizer plan.
Frequently Asked Questions
Tap or click a question below to see the answer:
If shortness of breath doesn’t improve, or you have high fever, chest pain, or repeated plugs, see a doctor or a pulmonologist for a plan to prevent and clear plugs.
Yes. With controlled or huff coughing, people can often dislodge and spit out a thick glob of mucus. If coughing doesn’t help and breathing is hard, seek medical care.
It can feel like something is stuck that won’t move with a normal cough. When it comes out, it can look like a thick, rubbery piece of sputum (phlegm). Color varies. Sputum color can change with infections, but color alone doesn’t diagnose infection—talk to your doctor if you’re unsure.
Usually indirectly—X-rays can show a collapsed area suggesting a plug; CT scans show plugs more clearly. Bronchoscopy can find and remove them.
No. The pregnancy mucus plug sits in the cervix. A lung mucus plug blocks an airway in the lungs.
Key takeaways
- A mucus plug is a thick blockage that stops air from reaching part of your lung.
- Clearing steps work best in layers: open airways, loosen mucus, then cough it out.
- Staying hydrated, active, and consistent with a simple daily routine can prevent most plugs.
- For frequent or severe plugs, work with a doctor on a personalized airway clearance plan.
Keep this close: Prompt clearing protects your breathing and can help prevent infections and flare-ups.
Disclaimer: This article is for informational purposes and isn’t a substitute for professional medical advice. Always talk with your doctor about your health and treatments.