On this page

What Is Mucomyst and How Does It Help? (Definition & Uses)
Mucomyst is the brand name for acetylcysteine, a prescription mucolytic inhalation solution used in a nebulizer to thin and loosen thick mucus in your lungs. A mucolytic is a medicine that breaks down thick mucus so it's easier to cough out.
Doctors use nebulized acetylcysteine for mucus‑heavy lung problems like cystic fibrosis, chronic bronchitis (COPD), bronchiectasis, and sometimes pneumonia or severe asthma. A Mucomyst nebulizer treatment delivers the medicine right where it's needed: into your airways.
Important note: the Mucomyst brand has been discontinued in the U.S. You will typically receive generic acetylcysteine inhalation solution. It's prescription‑only.
How it helps:
- Thins thick, sticky mucus.
- Makes coughing mucus out easier.
- Can support airway clearance with chest physiotherapy (percussion, positioning, and other techniques to move mucus).
In short: Mucomyst (acetylcysteine) is a prescription medicine you inhale to thin stubborn lung mucus.
Who Needs Nebulized Mucomyst? (When and Why It’s Prescribed)
Doctors consider nebulized acetylcysteine when mucus is so thick that simple steps like hydration, guaifenesin, chest physiotherapy, or saline aren't enough. It's commonly used for people with cystic fibrosis, chronic bronchitis/COPD, or bronchiectasis during times when mucus becomes hard to clear.
In practice, most doctors start or supervise the first doses in a clinic or hospital, especially if you have reactive airways like asthma. This lets them watch for wheezing or chest tightness and adjust the plan if needed.
Mucomyst isn't for routine cold or flu congestion or self‑treatment. It's typically used in specialty care (pulmonology, CF centers) or hospital settings for very stubborn secretions. In hospitals, doctors sometimes use nebulized acetylcysteine to help loosen mucus plugs or collapsed areas of lung (atelectasis) under close monitoring.
Rule of thumb: Doctors reserve nebulized acetylcysteine for people with very thick, hard‑to‑clear mucus that hasn't improved with simpler treatments.
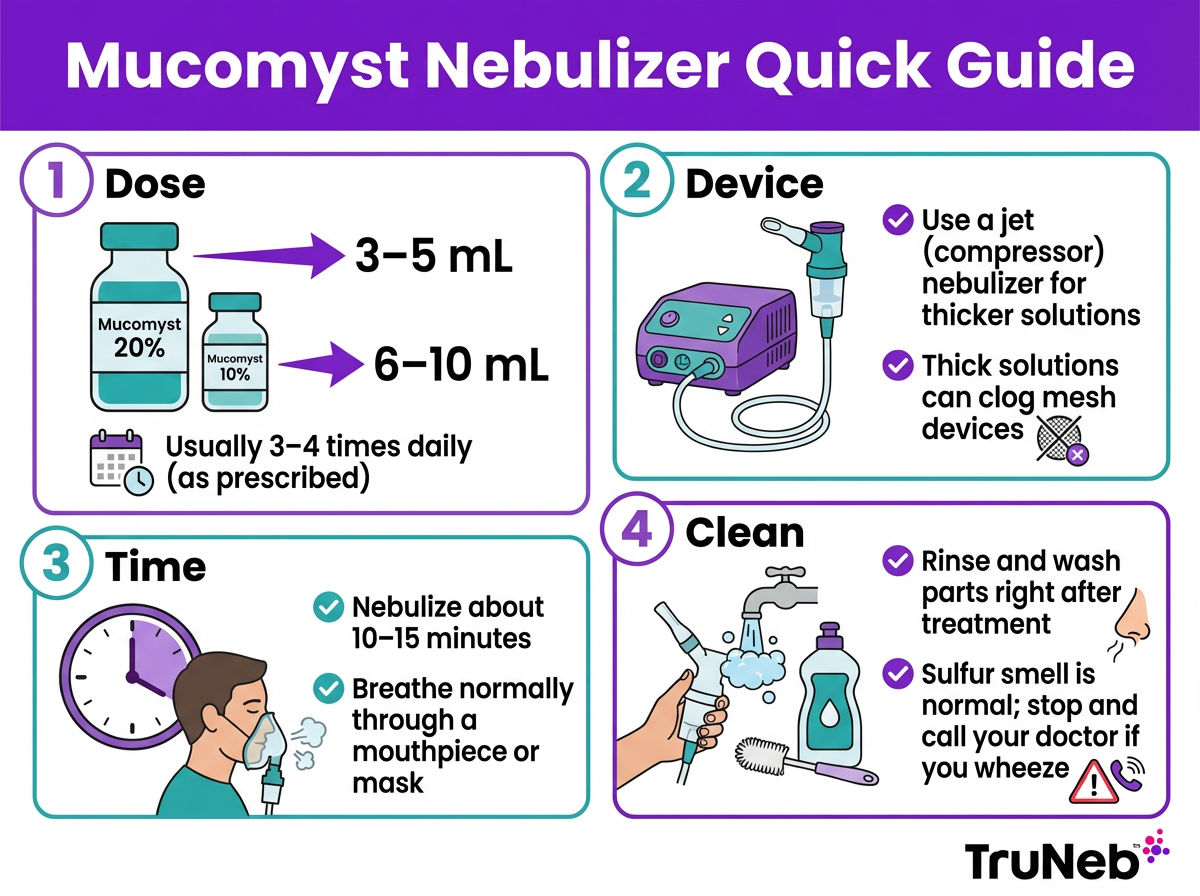
How to Use Mucomyst with a Nebulizer (Dosage & Administration)
Use Mucomyst exactly as prescribed. The label will list the strength (10% or 20%) and how frequently to use it. The details below are general information from drug references. Always follow the exact directions on your prescription label and what your doctor tells you.
Reference dosing (for context only—follow your prescription):
- References like GoodRx note that doctors typically prescribe 3–5 mL of 20% solution or 6–10 mL of 10% solution per nebulizer treatment, usually 3–4 times per day. Your exact dose and schedule come from your doctor.
If your doctor prescribes Mucomyst, a typical nebulizer session looks like this:
- Check the vial: Confirm 10% vs 20%.
- Measure the dose: Use the amount on your prescription. If your doctor told you to dilute, mix with the specified amount of sterile saline or sterile water.
- Pick the right device (see the device section below).
- Fill the cup: Pour the dose into the nebulizer medicine cup. Don't mix other medications in the same cup unless your doctor told you to.
- Breathe the mist: Sit upright. Use a mouthpiece or mask. Turn on the machine and take slow, relaxed breaths through your mouth. Treatments usually take about 10–15 minutes.
- Expect the smell: A sulfur or "rotten egg" odor is normal. Crack a window or use a small fan if it bothers you.
- Finish and clean: Turn off the compressor, discard any leftover solution, and clean the nebulizer parts right away so residue doesn't build up.
A few extra pointers:
- If you have asthma or tend to wheeze, your doctor might have you use a bronchodilator first.
- If your breathing suddenly feels tighter during a treatment, stop and follow the safety guidance below.
- Use the plastic parts intended for your nebulizer (see the safety section for details).
Mucomyst and Nebulizer Types (Why Device Choice Matters)
Acetylcysteine is thicker than most nebulizer medicines, so device choice affects performance.
- Jet (compressor) nebulizers are usually preferred for viscous solutions like Mucomyst.
- Mesh devices have fine membranes that can clog with thicker solutions. A device like the TruNeb™ portable mesh nebulizer is great for thin solutions (saline or bronchodilators), but it's not ideal for acetylcysteine unless your doctor and device manual say it's compatible.
- Always check your device manual and confirm with your doctor.
- ⚠️ Don't use Mucomyst in a steam inhaler or humidifier. Those devices aren't made to deliver medications safely to your lungs.
Key takeaway: Jet (compressor) nebulizers are the safer choice for nebulized acetylcysteine; mesh devices are better for thinner solutions like saline or bronchodilators.
| Device type | Mucomyst compatibility | Best for | Notes |
|---|---|---|---|
| Jet (compressor) | Generally compatible | Viscous solutions like acetylcysteine | Steady output; wall power; louder than mesh |
| Mesh (including TruNeb portable mesh) | Not recommended for thick solutions | Thin solutions: saline, bronchodilators | Small and quiet; thick solutions can clog the mesh |
Always check your device manual and your doctor’s instructions before using any medicine.
In short: A typical Mucomyst nebulizer treatment involves inhaling a small prescribed dose of 10% or 20% acetylcysteine through a jet nebulizer for about 10–15 minutes, several times a day as directed by your doctor.
Side Effects and Precautions of Mucomyst Inhalation
Most people do fine with nebulized acetylcysteine, but side effects can happen.
Common side effects:
- Coughing, throat or chest irritation.
- Nausea or vomiting; bad taste or smell.
- Runny nose, sore throat, mouth sores.
- Drowsiness or clammy skin (less common).
Serious reactions (call your doctor right away):
- Wheezing or chest tightness (bronchospasm—sudden tightening of the airways that causes wheezing or trouble breathing).
- Trouble breathing.
- Rash or signs of allergy.
Safety tips:
- Asthma: Use with caution. Your doctor might recommend a bronchodilator before Mucomyst.
- Device materials: Use the plastic parts meant for your nebulizer. The official Mucomyst label warns against certain metals and rubber; this warning comes from the product label.
- Don't mix in the cup unless told to: Acetylcysteine can interact with some meds if combined.
- Clean immediately after each use: This solution can leave residue. Wash and dry parts to help prevent clogging and germs.
- Storage: Follow your label for how to store opened vials. Most vials are single‑use; if multi‑dose, ask your pharmacist how long they remain good.
If you feel worse during a treatment, stop and contact your doctor.
⚠️ If you have severe trouble breathing, swelling of your face, lips, tongue, or throat, or widespread hives, stop the treatment and call 911 or your local emergency number right away.
If your symptoms don't improve after a few days of treatment, or if your mucus or breathing suddenly gets worse, contact your doctor to review your plan.
If you're pregnant or breastfeeding, talk with your doctor before using inhaled acetylcysteine so they can weigh the benefits and risks for you and your baby.
In short: Nebulized Mucomyst usually causes mild issues like cough or throat irritation, but it can sometimes trigger wheezing or allergy, so call your doctor if your breathing gets worse.
Alternatives to Mucomyst: Saline, Enzymes, and Other Mucus Thinners
There are other ways to thin mucus if acetylcysteine isn't right for you.
- Hypertonic saline (3% or 7%): Nebulized saltwater draws water into the airways and thins mucus so it's easier to clear. It's usually used daily in CF and bronchiectasis and works well with portable devices. TruNeb offers pre‑measured 3% and 7% saline vials that you can ask your doctor about if they recommend hypertonic saline. Use under a doctor's guidance.
- Dornase alfa (Pulmozyme): An inhaled enzyme used mainly in cystic fibrosis. It breaks down DNA in sticky secretions.
- Oral expectorants (guaifenesin): Helpful for milder congestion. Not as strong as inhaled therapy but can support mucus clearance.
- Chest physiotherapy and hydration: Postural drainage, percussion, oscillation devices, and drinking enough fluids all help move mucus.
Some treatment plans combine options—such as daily hypertonic saline with a portable nebulizer and reserving acetylcysteine for especially thick mucus—to match each person's lungs and condition.
In short: Doctors sometimes combine options—using daily hypertonic saline for maintenance and reserving acetylcysteine for very thick mucus—based on your condition and your doctor's guidance.
FAQs about Mucomyst and Nebulizer Therapy
Tap or click a question below to see the answer:
Yes. Acetylcysteine inhalation is prescription‑only. A doctor has to decide if it's appropriate for you.
Thick solutions can clog fine mesh. Most doctors prefer a compressor (jet) nebulizer for acetylcysteine. Check your device manual and ask your doctor which device you should use.
The Mucomyst brand was discontinued in the U.S. Pharmacies dispense generic acetylcysteine inhalation solution when prescribed.
A common prescription calls for 3–4 treatments per day, but always follow your doctor's exact schedule.
The medicine works during the 10–15 minute treatment to thin mucus. Clearing that mucus can take time and can be easier with chest physiotherapy.
Contact your doctor. They might add chest physiotherapy, adjust dosing, or consider alternatives like hypertonic saline or, in CF, dornase alfa.
Disclaimer: This article is for informational purposes only and isn't a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, medications, and treatment options.