On this page
How COPD Can Limit Your Ability to Work
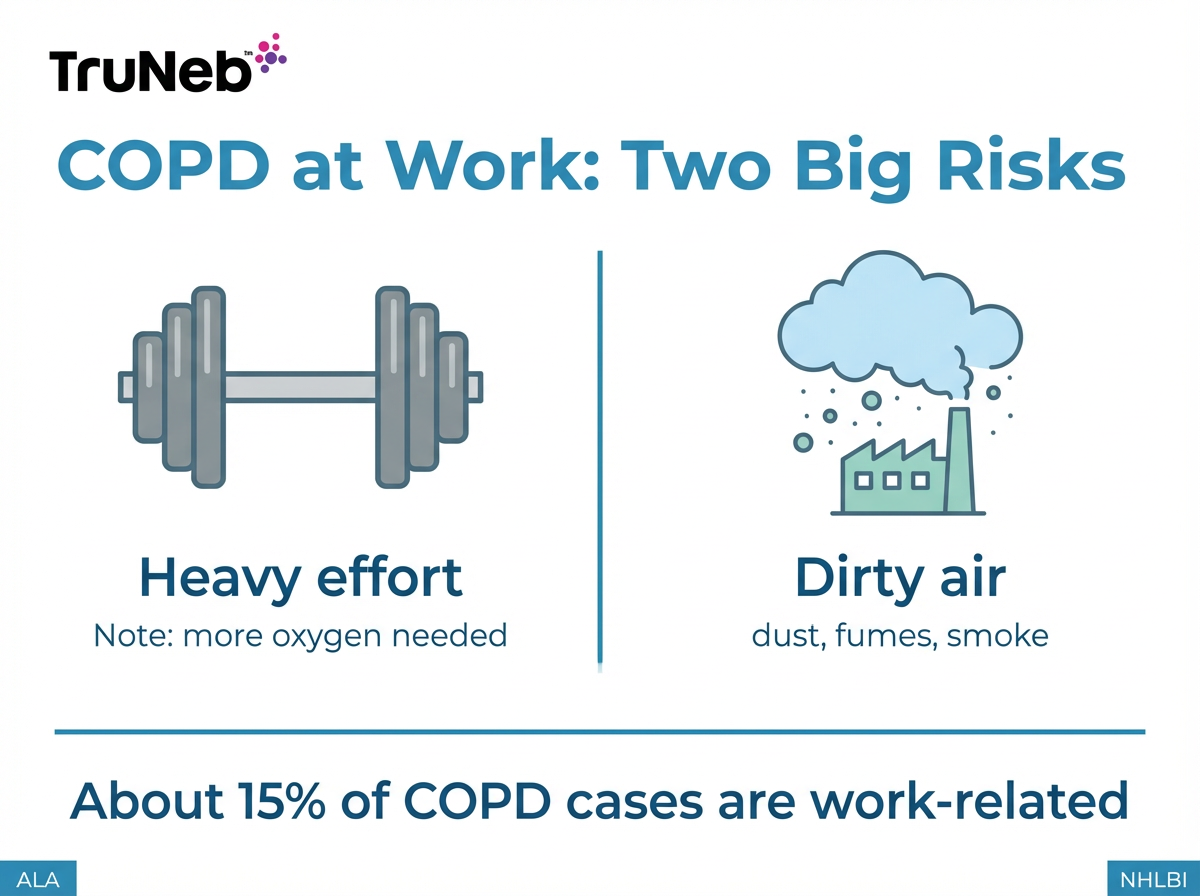
COPD reduces airflow, so tasks that were once easy can feel like a workout. Two things at work tend to make symptoms worse: heavy effort and dirty air.
- Physical strain raises your body’s need for oxygen. With COPD, your lungs can’t keep up, so lifting, climbing, or fast-paced work can leave you breathless.
- Airborne irritants like dust, fumes, smoke, and diesel exhaust can inflame your airways and trigger flare-ups.
Your day-to-day ability also depends on severity. With mild COPD, you can often handle light tasks in clean air. Doctors usually classify COPD as mild, moderate, or severe. Your work capacity tends to drop as the disease advances. With moderate to severe COPD, even routine exertion can be hard without adjustments.
Key takeaway: If a job makes you breathe harder or breathe in dirty air, it will likely make COPD symptoms worse.
Jobs to Avoid if You Have COPD
Avoid jobs that push your lungs hard or fill the air with irritants. Here are the main types of jobs to avoid with COPD and examples to watch out for.
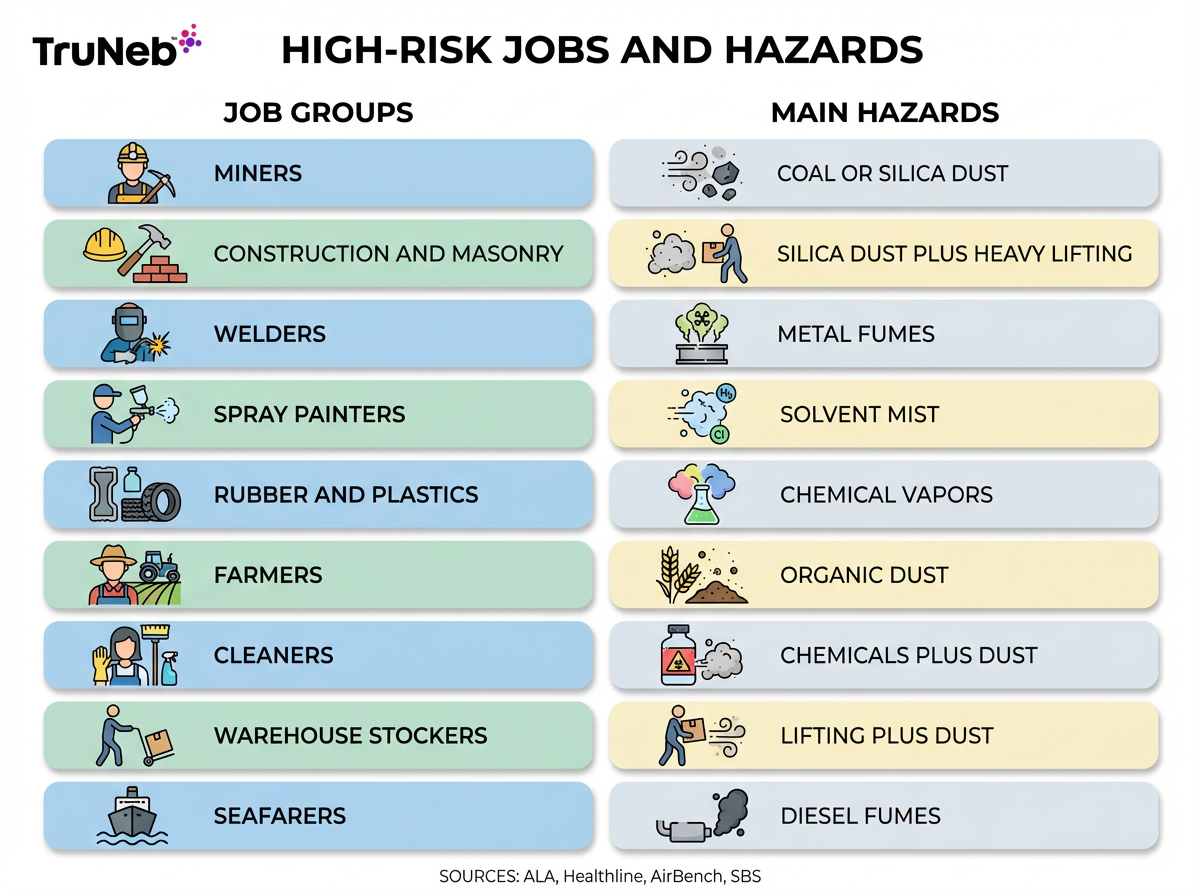
Physically Demanding Labor Jobs
- Construction labor, roofing, carpentry, landscaping
- Warehouse loaders and stock handlers
- Farm field work and other strenuous outdoor roles
- Firefighting or roles that require running with heavy gear
Why they’re risky: intense effort raises oxygen demand, which can cause severe shortness of breath and low oxygen levels during tasks.
Jobs with Dust and Particles
- Mining and quarry work (coal and silica dust)
- Stone cutting, masonry, cement and demolition
- Textile mills, grain elevators, flour mills, and bakeries
- Farming and animal handling (organic dust from hay and grain)
Why they’re risky: fine particles reach deep into the lungs, trigger inflammation, and can speed up decline.
Jobs with Chemical Fumes and Smoke
- Welding and metalworking (metal fumes)
- Spray painting, varnishing, and finishing (solvents and isocyanates)
- Rubber and plastics manufacturing (chemical vapors)
- Auto repair in enclosed garages (exhaust and solvents)
- Firefighting and industrial cleanup with smoke and chemical exposure
Why they’re risky: toxic vapors irritate and inflame the airways, setting off cough, wheeze, and flare-ups.
Jobs in Extreme Environments
- Outdoor work in freezing air or intense heat
- High-altitude roles with thin air (e.g., mountain operations)
- Confined, poorly ventilated spaces (e.g., engine rooms)
Why they’re risky: cold, heat, low oxygen, and bad ventilation strain already-limited breathing.
Other High-Risk Occupations to Note
- Cleaners and janitors (dust stirred up + strong cleaning agents)
- Warehouse stockers and packers (lifting + dusty storage)
- Seafarers and engine room crew (diesel fumes)
- Food and tobacco processing (organic dust and vapors)
Why they’re risky: these roles combine irritants (dust, fumes, strong chemicals) with lifting or poor ventilation, which can trigger symptoms or flare-ups.
Key takeaway: Avoid heavy labor and any job with dust, fumes, or smoke, and choose clean-air, low-exertion work instead.
Keep Your Lungs Safer on the Job
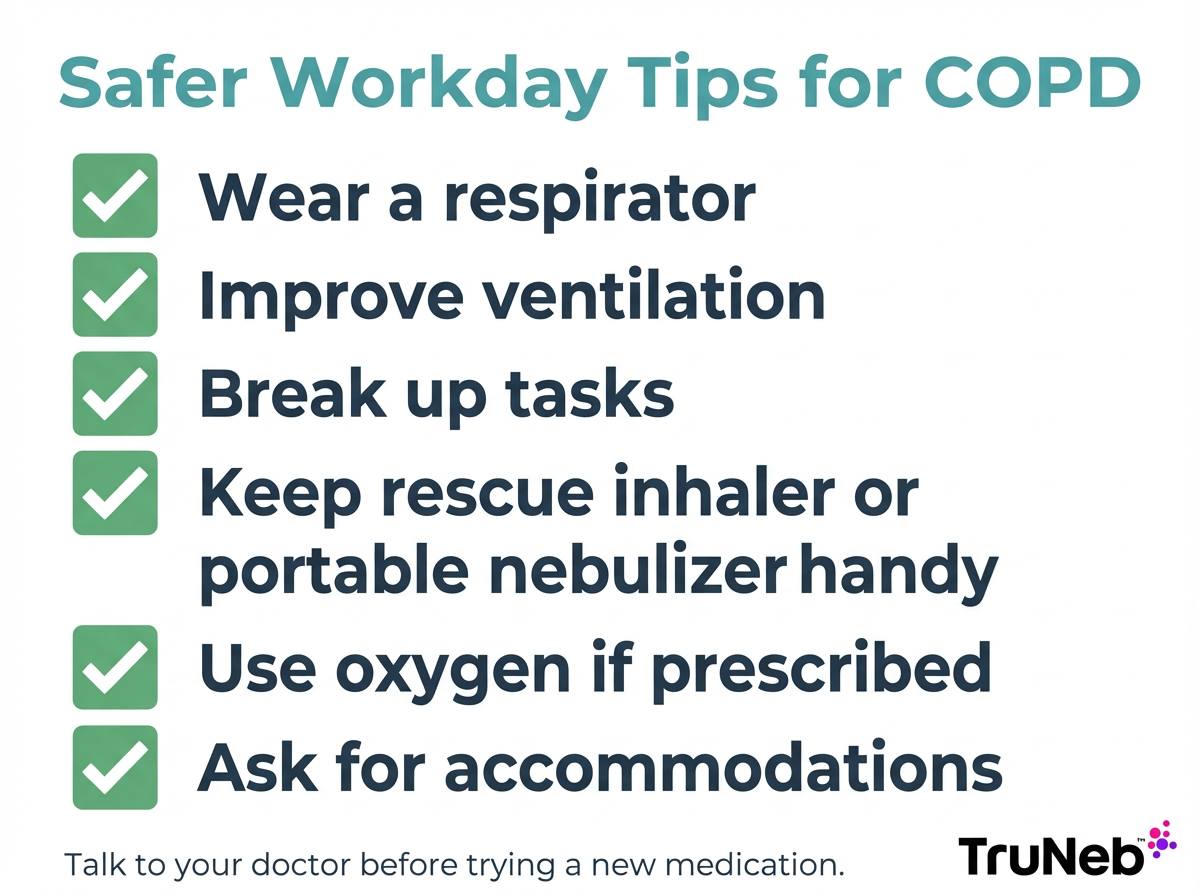
You might not be able to switch jobs right away. These steps can help you breathe easier at work.
Safety note: Talk to your doctor before trying a new medication.
- Wear the right mask. Use an N95 or job-specific respirator when dust or fumes are present.
- Improve ventilation. Ask for better local exhaust or air filtration where particles build up.
- Pace your effort. Break big tasks into smaller chunks and rest before you are wiped out.
- Keep quick relief nearby. Carry your rescue inhaler. If your doctor has prescribed nebulized medication, a portable mesh nebulizer can help you take a treatment during a break if symptoms spike.
- Use oxygen as prescribed. If your doctor ordered oxygen, use it at work as directed.
- Ask for adjustments. Request lighter duties, schedule tweaks, or a move to a cleaner area if possible.
- Build stamina safely. Pulmonary rehab skills (like pursed-lip breathing and gentle training) can make daily tasks feel easier over time.
⚠️ If you have severe shortness of breath, chest pain, blue lips or fingers, confusion, or trouble speaking in full sentences, call 911 or seek emergency medical care right away.
Key takeaway: Using a respirator, improving ventilation, pacing yourself, and keeping medications on hand can make tough workdays more manageable with COPD.
Know Your Rights and Options at Work
You have options if your job is harming your breathing.
- Ask for reasonable accommodations. Under laws like the Americans with Disabilities Act (ADA), you can ask for reasonable accommodations that help you do the essential parts of your job. Many employers can adjust duties, schedules, or workspaces so you can do the essential parts of your job more safely. Examples: moving to a cleaner area, lighter tasks, or partial remote work.
- Consider a role change. If dust, fumes, or heavy labor are baked into your current role, look for indoor work with clean air and minimal physical effort that uses your skills in new ways (like training, inspecting, scheduling, or desk-based work). State vocational rehabilitation or job retraining programs can help you transition to safer work.
- If work is no longer safe or possible, explore disability benefits. Severe COPD often qualifies for Social Security Disability Insurance (SSDI), depending on your test results and symptoms. Your doctor’s notes and lung function tests help document need.
- Take care of your health first. Switching roles or stepping back is hard, but protecting your lungs can prevent more serious setbacks.
If you’re unsure where to start, talk with your doctor and HR. They can help with paperwork, task adjustments, or time off for recovery.
Key takeaway: If your job harms your breathing, ask for accommodations, consider safer roles, or explore disability with your doctor’s support.
FAQs: Working with COPD
Tap or click a question below to see the answer:
Yes. Many people keep working by choosing lighter-duty indoor roles with good air quality and making smart adjustments. The right approach depends on your COPD severity and your job’s demands. Talk with your doctor and HR about accommodations.
Look for indoor, low-exertion roles with clean air. Examples: office admin, accounting, librarian, IT, call center, remote customer support, writing, or design. The key is avoiding heavy labor and air irritants.
Prepare and pace. Keep your rescue inhaler handy, and consider using a portable nebulizer during breaks if your doctor has prescribed nebulized medication. Take short, planned rests, use pursed-lip breathing with effort, and work in cool, well-ventilated spaces. Always check with your doctor before starting any new medication or changing how you use your current ones.
Call your doctor first to update your plan. Then speak with your employer about adjustments, use protective gear, and reduce exposure. If symptoms stay bad, consider moving to a different role or taking time off to protect your lungs.
It can be. If COPD substantially limits your breathing or activity, you could qualify for workplace accommodations. If you can’t work safely despite accommodations, you could qualify for SSDI if you meet Social Security’s criteria. Your doctor’s documentation is essential.
Key takeaway: Most people with COPD do best in clean-air, low-exertion roles, with a clear plan from their doctor and practical workplace adjustments.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, work situation, and any changes to your treatment plan.