On this page
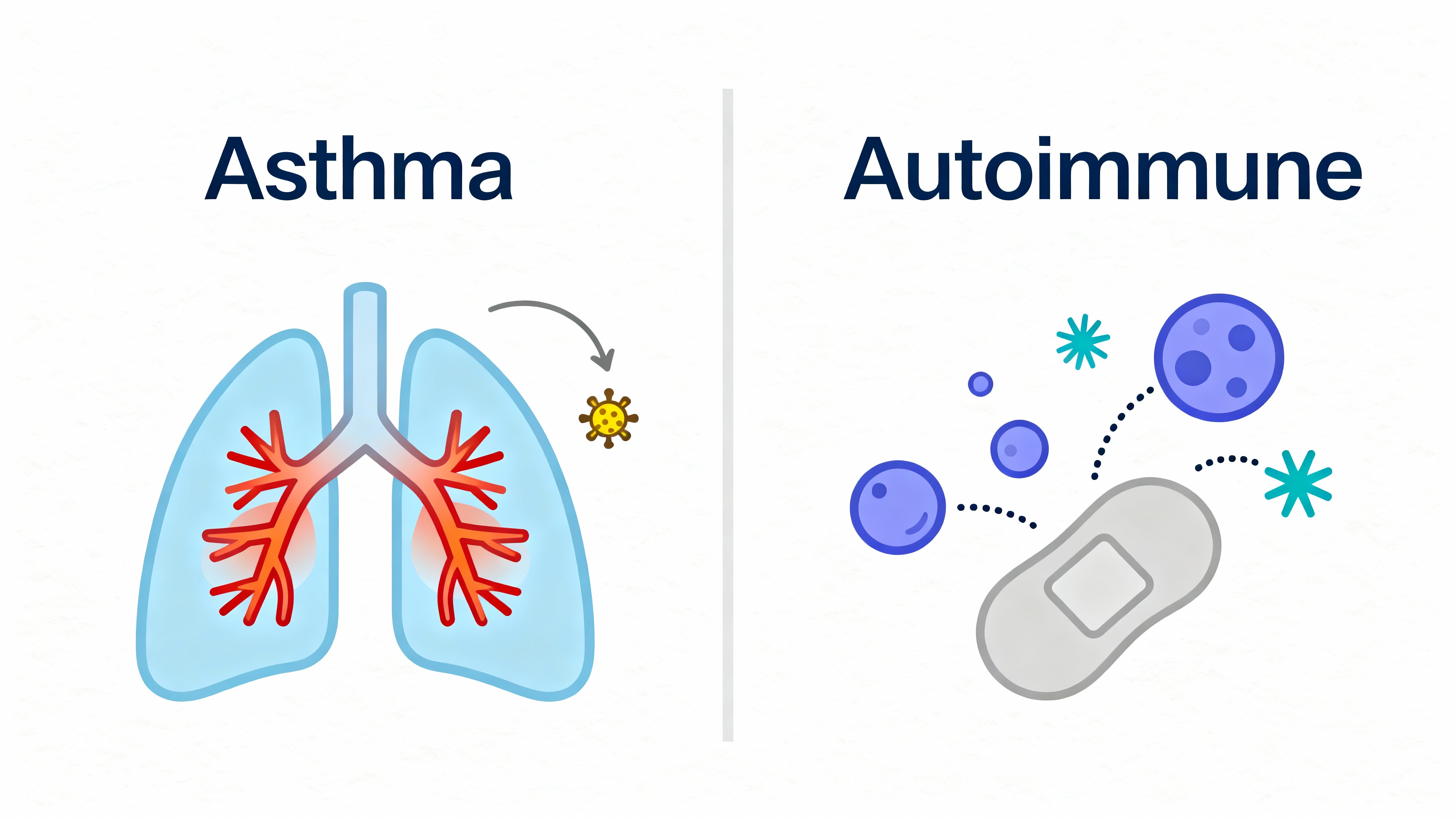
No. Asthma is not an autoimmune disease. It is a chronic inflammatory disease of the airways. Your immune system overreacts to things like pollen, dust, smoke, or cold air and your bronchial tubes get swollen and tight. In autoimmune diseases, the immune system attacks the body’s own tissues. That is not what happens in asthma.
One-liner: Asthma is trigger-driven airway inflammation, not a self-attack by the immune system.
Why Asthma Is an Inflammatory Disease, Not Autoimmune
In asthma, a harmless trigger enters your airways and your immune system reacts too strongly. The airway lining swells, makes extra mucus, and the muscles around the tubes tighten. That’s why you can wheeze, cough, or feel chest tightness.
Autoimmune disease is different. In autoimmune conditions, the immune system targets the body itself (for example, joints in rheumatoid arthritis or insulin-making cells in type 1 diabetes). Asthma doesn’t target self-tissue. It’s an overreaction to outside triggers.
Think of it this way: asthma is a false alarm; autoimmunity is friendly fire.
Rule of thumb: External triggers drive asthma; internal self-targeting defines autoimmunity.
Understanding Asthma’s Triggers and Immune Response
Common triggers include:
- Allergens: pollen, dust mites, mold, pet dander
- Irritants: tobacco smoke, strong odors, air pollution
- Other: viral colds, exercise, cold air
What happens next:
- IgE and mast cells: In allergic asthma, IgE antibodies (allergy antibodies) recognize the allergen and tell mast cells to release chemicals like histamine.
- Eosinophils: Eosinophils (inflammation-driving white blood cells) add to swelling and mucus in the airways.
- Bronchoconstriction: Airway muscles tighten, making it hard to move air.
This is an immune overreaction to something from outside your body. It is not the immune system attacking lung tissue on purpose.
Key idea: In asthma, remove the trigger and calm the inflammation, and breathing usually improves.
How Autoimmune Reactions Differ
Autoimmune diseases happen when the immune system goes after the body’s own cells (self-antigens). For example, in type 1 diabetes it destroys insulin-making cells, and in rheumatoid arthritis it attacks joint lining. These attacks commonly involve autoantibodies or misdirected T cells and can affect many body parts.
Asthma does not fit this pattern. It mainly affects the lungs and flares with triggers. No self-tissue is the target.
Quick check: Autoimmunity targets self; asthma reacts to exposures.
Asthma vs. Autoimmune Disease: Key Differences
Quick compare: asthma flares are triggered by outside exposures; autoimmune flares come from the immune system targeting the body.
| Topic | Asthma | Autoimmune diseases |
|---|---|---|
| Main driver | Outside triggers (allergens, irritants, infections, cold air) | Immune system targets the body’s own tissues |
| Immune target | No self-tissue target; reaction to inhaled substances | Self-tissue (e.g., joints, pancreas, nerves) |
| Key immune pattern | Type 2 inflammation; IgE, mast cells, eosinophils | Often Th1/Th17 pathways; autoantibodies or self-reactive T cells |
| Where it shows up | Mostly the lungs/airways | One or multiple organs; can be systemic |
| Onset of flares | Usually tied to trigger exposure | Can flare without external trigger |
| Treatment focus | Reduce airway inflammation and avoid triggers; inhalers, sometimes biologics | Calm immune attack; systemic immunosuppressants and disease-modifying drugs |
| Examples | Asthma (allergic or eosinophilic subtypes) | Rheumatoid arthritis, lupus, type 1 diabetes, multiple sclerosis |
Note: Immune profiles vary by condition; Th1/Th17 vs Th2 is a general pattern, not an absolute.
Asthma and the Immune System: Overreaction vs Autoimmunity
Having asthma does not mean you are immunocompromised. Asthma reflects an overactive response in the airways, not a weak defense system. People with asthma can usually fight infections normally. Colds and other infections can trigger flares, which can make asthma feel worse.
If someone’s immune system is weakened for another reason (for example, certain illnesses or treatments), they can catch more respiratory infections—and infections can set off asthma symptoms more frequently.
Here’s the science: allergic conditions like asthma are linked to a Type 2 (Th2) immune profile, while many autoimmune conditions lean more Th1/Th17. Some studies suggest these profiles can push in opposite directions, so people with strong allergic tendencies might have a lower risk of some autoimmune diseases. This is a trend, not a rule.
Bottom line: Asthma involves an over-alert immune response, not a broken one.
Eosinophilic Asthma and Autoimmunity — What’s the Connection?
Eosinophilic asthma is a severe form marked by high levels of eosinophils (a type of white blood cell) in the airways. It can be intense, and sometimes there isn’t a clear allergen trigger.
A rare autoimmune vasculitis called EGPA (formerly Churg-Strauss) includes asthma symptoms as part of a broader autoimmune process; that’s different from typical eosinophilic asthma, which isn’t autoimmune.
Even so, it is not classified as an autoimmune disease. There’s no specific self-target the immune system is attacking. Care focuses on calming Type 2 inflammation. Doctors sometimes prescribe targeted biologics that reduce eosinophils or block Type 2 signals.
Key point: Severe inflammation does not equal autoimmunity.
How Knowing the Difference Affects Treatment
Because asthma is an inflammatory airway disease, treatment aims to reduce airway swelling and prevent flares. Common tools include inhaled medicines at home, bronchodilators (to open airways), and trigger control. For tough cases, doctors can add targeted biologics.
Autoimmune diseases often need body-wide immune calming with immunosuppressants or disease-modifying drugs. Those aren’t standard for asthma.
If you use inhaled medicines at home, a portable mesh nebulizer like TruNeb™ can help you take your doctor-prescribed treatments when symptoms spike or when a mask/mouthpiece fits better than a handheld inhaler. It doesn’t replace your care plan. It just helps you stick to it when breathing feels hard.
Practical takeaway: Treat asthma by calming airway inflammation and managing triggers—very different from suppressing an autoimmune attack.
Safety Note
- Do not change or stop your medications on your own. Your doctor can adjust your plan if needed.
- Inhaled steroids can slightly raise the risk of certain infections in the mouth or airways at higher doses. Rinsing your mouth after use can lower this risk—follow your doctor’s instructions.
- Talk to your doctor before trying a new medication.
- Emergency: If you have severe trouble breathing, blue lips/face, or cannot speak in full sentences, call 911 or seek emergency care immediately.
- When to escalate: Talk to your doctor if your symptoms don’t improve, keep getting worse, or you’re considering changing your treatment.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Asthma is a chronic inflammatory airway disease triggered by external exposures (like pollen, dust, smoke, or cold air), not a self-directed immune attack.
Asthma involves the immune system, but it isn’t an immune deficiency or an autoimmune disease. It’s an overreaction to outside triggers that causes airway inflammation.
Generally, no. Asthma reflects an overactive response in the airways, not a weak defense. Infections can trigger flares, and some medicines may slightly raise infection risk.
No. Asthma is an overactive immune response in the airways to triggers. An immune deficiency means the body can’t fight infections well.
No. They are different conditions. Someone could have both, but one doesn’t cause the other.
No. Allergic asthma is driven by IgE and Type 2 inflammation in response to allergens; autoimmune disease is a self-directed immune attack.
Some autoimmune diseases can affect the lungs (for example, lung involvement in rheumatoid arthritis or lupus, or vasculitis like EGPA). These involve immune attack on self-tissue and are not asthma.
Key Takeaways
- Asthma is an inflammatory airway disease, not an autoimmune disease.
- Triggers matter: pollen, dust, smoke, cold air, and infections can set off flares.
- Autoimmune means self-attack; asthma does not do that.
- Treatment differs: asthma care calms airway inflammation and avoids triggers; autoimmune care suppresses self-directed immune attacks.
- You can manage asthma well with the right plan and follow-up. If symptoms are hard to control, ask your doctor about next steps.
Plain truth: Calm the airway inflammation, reduce triggers, and you can breathe easier.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice. Always talk to your doctor about your symptoms and treatments.