On this page

Why It's Hard to Tell
You can see a puff, hear a hiss, and still have no medicine coming out. Pressurized metered-dose inhalers (MDIs) use propellant gas that can spray even after the medicine runs out. So looks, sound, and shaking aren't reliable. The safe way is to track doses or use a built-in counter. If you use a dry powder inhaler (DPI), it behaves differently: there's no propellant mist, and most models include a dose counter—see the methods below.
Key point: you can't tell by sight, sound, or shaking. You need a counter or a dose log.
MDIs can still spray propellant after medicine is gone; mist is not proof of drug.DPI devices typically include a dose counter and don’t produce a propellant mist.Zero on the counter means empty—even if it still sprays.The water “float test” is not recommended.
Source: Medicines for Children

Reliable Ways to Know How Much Medicine Is Left
Check the Dose Counter
Most newer inhalers have a dose counter window that counts down each puff. If it shows 0 (or turns red), the inhaler is considered empty, even if it still sprays. If your counter seems stuck or not moving, don't trust it—switch to manual tracking or replace the inhaler. If you use a dry powder inhaler (DPI) like Diskus or Ellipta, check its dose window—these devices typically have built-in counters and don't produce a propellant mist. Some devices count inhalations rather than button presses, so follow your device's indicator.
Key takeaway: zero on the counter means it's empty.
Count Your Puffs (Manual Tracking)
If your inhaler doesn't have a counter, use this 3-step method:
- Find the total puffs in a new inhaler (for example, 200 or 120).
- Note how many puffs you use (daily plan or tally each use).
- Do the math to estimate the run-out date, then mark that date on the canister or your phone.
Use the quick table below to estimate how long your inhaler will last.
Example: 120 puffs at 4 puffs/day ≈ 30 days.
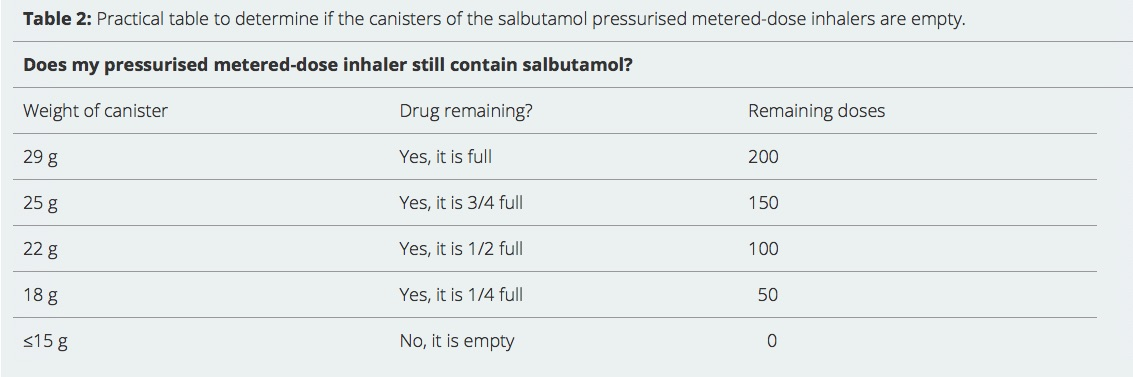
Weigh the Canister (Specific Brands Only)
Some metal canisters (for example, Ventolin Evohaler) can be weighed on a small kitchen scale and compared to known full vs empty weights. This works only for certain models and isn't practical for most people. Use counters or tracking as your main method.
Optional Tech Helpers
Smart caps and apps can track puffs and send reminders. If you have one, it can help you avoid running out.
Reliable ways to know what's left include checking a dose counter, tracking your puffs, and—for specific models—using a weight check.
| Inhaler size (puffs) | Your daily puffs | Estimated days |
|---|---|---|
| 200 | 2 | 100 |
| 200 | 4 | 50 |
| 200 | 8 | 25 |
| 120 | 2 | 60 |
| 120 | 4 | 30 |
| 120 | 6 | 20 |
Estimates assume consistent use. If relief feels weaker or the counter is near zero, replace sooner.
Myths and What Not to Do
- Don't rely on shaking or listening. An MDI can still slosh because propellant remains; that doesn't prove medicine is there.
- Don't test-spray into the air to "check." You might only see propellant, and you'll waste any remaining doses.
- Don't use the water "float test." It's not reliable and can damage the canister.
- You can't judge by taste or the cold feel of the spray either.
Bottom line: ignore quick tricks. Use a counter or track your puffs.
When to Replace Your Inhaler
- Replace when the counter hits 0 or you've used the labeled number of puffs. Keep in mind it can still spray propellant without medicine.
- Don't wait for the spray to stop. That's too late—you've likely had puffs without drug.
- Rescue inhalers: if you've had one for a long time, check the expiry date and consider keeping a fresh spare.
- Counter not working? Treat it as unreliable. Start manual tracking right away or replace the inhaler.
If you're using your reliever more than usual, talk to your doctor. Your asthma plan might need an update.
Simple rule: plan to swap before empty to avoid gaps in treatment.
Tips to Never Run Out
- Keep a backup. Carry a spare rescue inhaler.
- Set reminders. Use your phone to check the counter or your tally weekly.
- Write the start and expected end date on the canister or box.
- Refill early. Request a new inhaler before you're low.
- Clean the mouthpiece as instructed to prevent clogs.
- If you travel, pack your spare in a separate bag.
Simple habits—keeping a spare, setting reminders, and writing your start and end dates—help you avoid last-minute surprises.
What Happens If You Use an Empty Inhaler?
If a rescue inhaler is empty, you won't get relief during breathing trouble, which can turn into an emergency. If a daily controller inhaler is empty, your symptoms can creep back because you're not getting your medicine. Inhaling propellant alone isn't the harm—the risk is untreated asthma. Have a plan, and replace before empty.
If you have severe symptoms like trouble speaking, blue lips or face, chest pulling in, or your reliever isn't helping, call 911 or seek emergency care.
An empty inhaler gives you no medicine—the risk is untreated asthma, not the propellant.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Shaking and listening aren't reliable because propellant can remain and make noise even when medicine is gone.
No. Experts do not recommend it. It's unreliable and can damage the canister.
Common sizes are 200 puffs for many rescue inhalers and 120 puffs for many controller inhalers. Check your box or leaflet for the exact number.
Treat it as unreliable. Start manual tracking right away or replace the inhaler so you don't run out unexpectedly.
Most DPIs include a dose window or counter; follow the device's indicator and replace it when it reaches zero.
Bottom Line
Don't guess. Use a dose counter or track your puffs, plan your refill date, and keep a backup so you always have medicine when you need it.
Disclaimer: This article is for informational purposes only and isn't a substitute for professional medical advice. Always talk to your doctor about your symptoms, inhaler use, and treatment options.