On this page

How Long Does It Take for Your Lungs to Heal from Vaping?
If you've quit or are thinking about quitting, you're probably wondering: how long does it take for your lungs to heal from vaping? The short answer: your lungs start to repair within days, and improvements build over the next weeks to months. Below, you'll find a realistic timeline and practical steps to support recovery.
Why Vaping Damages Your Lungs and Quitting Lets Them Heal
Remove the irritants and your lungs switch from defense to repair within days.
Vaping sends tiny chemicals and heated aerosol deep into your airways. This irritates the lining, sparks inflammation, and slows your cilia—those tiny hair-like sweepers that move mucus up and out. When cilia slow down, mucus sits, airways clog, and breathing feels tight.
Some vape ingredients can be especially harsh. Flavorings like diacetyl have been linked to small-airway scarring nicknamed popcorn lung. Oils and thickeners can trigger chemical pneumonia (a type of lipoid pneumonia). In rare cases, people develop a serious illness called EVALI. EVALI is an acute vape-related lung injury that can cause severe breathing problems and sometimes requires hospital care. The more frequently and longer you vape, the more your lungs are exposed to these irritants.
Here’s the good news. When you stop vaping, you remove the source of irritation. Inflammation starts to fall. Cilia wake back up and begin clearing out mucus and debris. Your lungs are built to heal where they can—and they get to work as soon as the exposure stops.
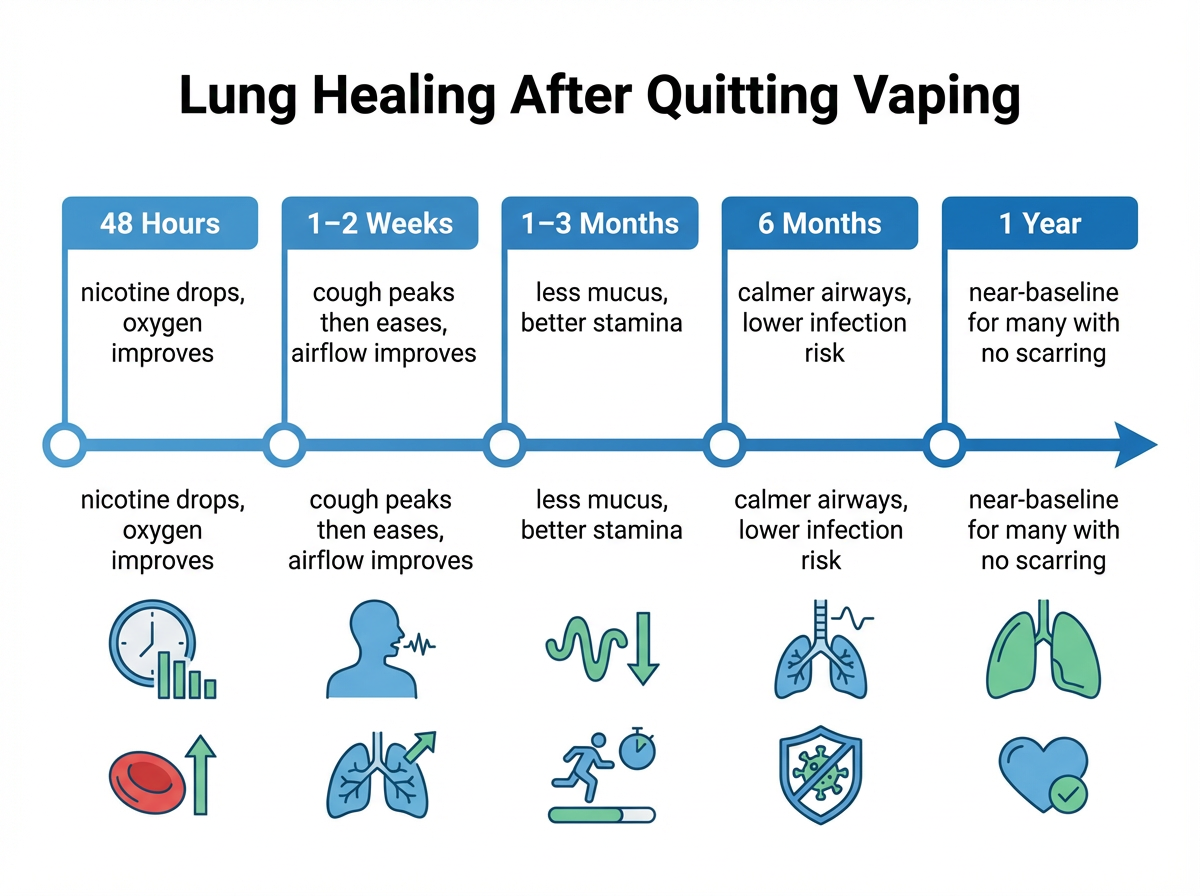
Lung Recovery Timeline After Quitting Vaping
Most people breathe easier within weeks and see major gains between 3 and 12 months. Because vaping is newer than smoking, these timeframes draw from smoking-cessation research and early vaping studies; the evidence is still evolving.
Within 24–48 hours
- Nicotine levels fall fast. Heart rate and blood pressure begin to normalize. Blood oxygen improves as your body clears lingering gases.
- Cravings and withdrawal often peak around day 3 for nicotine users, but timing can vary. A short burst of extra coughing is common as cilia wake up.
1–2 weeks
- Cilia are sweeping again. It’s common to cough up more mucus at first—that’s your cleanup phase. Then the cough starts to ease.
- Airflow begins to improve. Climbing stairs or walking hills starts to feel easier.
1–3 months
- Less coughing and less mucus. Breathing during exercise feels more natural.
- Measurable lung function improvement shows up on breathing tests. Endurance and recovery after activity pick up.
6 months
- Airway lining is calmer. Daily breathing takes less effort. Many people no longer think about their breathing during normal activities.
- Your lungs’ defenses (cilia and immune cells) are working well again, so infection risk drops.
1 year and beyond
- If no permanent scarring occurred, lung function can be close to your personal baseline, especially in people who didn’t smoke.
- If you had a severe injury (like EVALI or small-airway scarring), some changes can persist—but quitting prevents more damage and can bring meaningful symptom relief.
What Affects How Fast Your Lungs Heal
Healing speed depends on how long and how frequently you vaped, your health, and what you vaped.
Duration and intensity
- Heavy, long-term use means more irritation and sometimes more healing time. Shorter, lighter use usually bounces back faster.
Age and overall health
- Younger lungs tend to repair faster. Underlying health issues can slow recovery.
Pre-existing lung conditions
- Asthma, COPD, or repeated bronchitis can make recovery slower. You can still improve a lot, but some baseline treatment might be needed, as your doctor recommends.
What you vaped
- Nicotine e-liquids commonly cause irritation that improves after quitting.
- THC oils (especially those linked to EVALI) can cause acute injury. Recovery can take longer and may leave scars.
Environmental exposures
- Breathing secondhand smoke, workplace fumes, or heavy pollution can slow recovery.
Smoking history
- If you smoked and vaped, damage can be layered. Quitting everything helps, but some changes from smoking may be long-term.
Bottom line: most ex-vapers see strong gains within the first year. Severe injuries and long histories can need more time and medical follow-up.
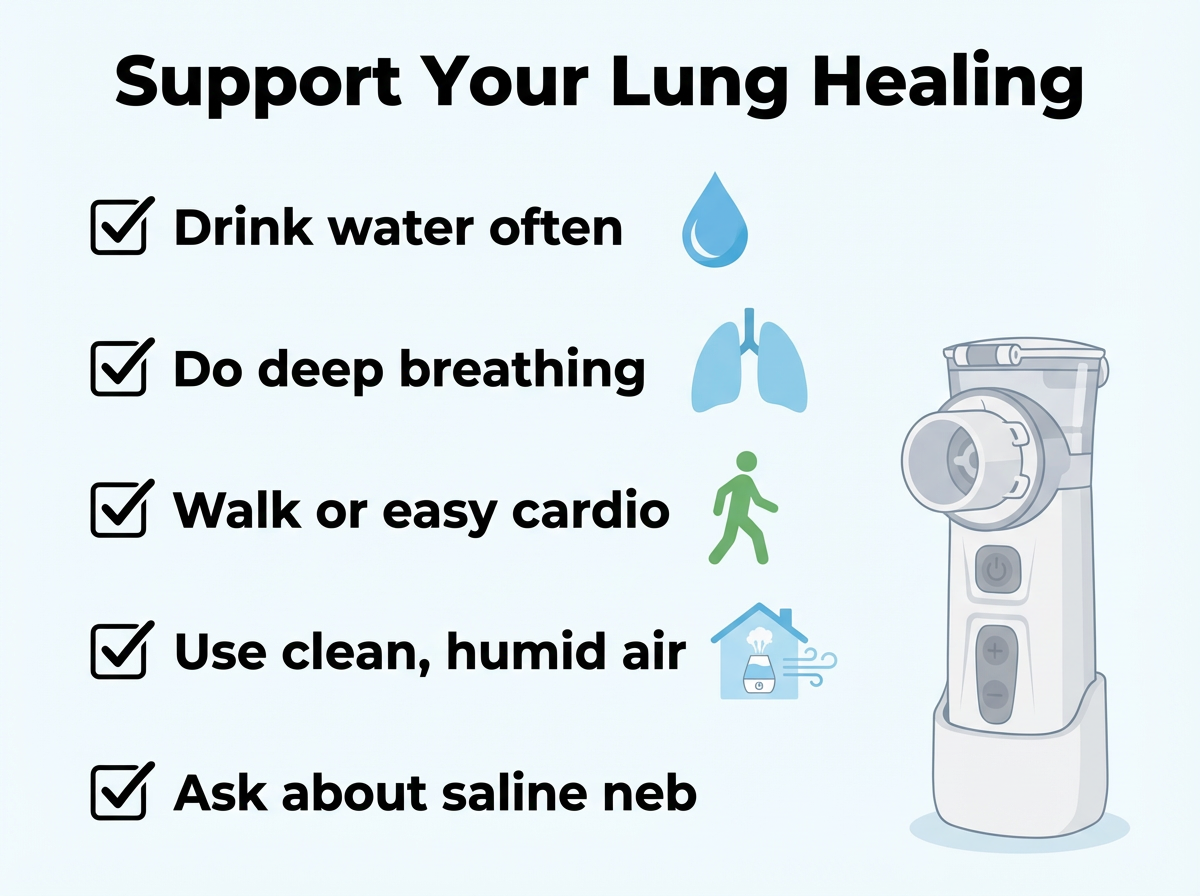
Five Ways to Help Your Lungs Recover
Small daily steps make breathing easier while you heal. Simple daily habits like hydration, gentle movement, clean air, and balanced nutrition support your lungs as they repair after vaping.
1) Drink more water
- Hydration thins mucus so your recovering cilia can move it out. Warm tea can soothe a scratchy throat from extra coughing.
2) Breathe deeper and move your body
- You can try easy drills like diaphragmatic or pursed-lip breathing if your doctor has cleared you for activity.
- Light cardio—walking, cycling, or swimming—can gently help build lung capacity if it feels comfortable and fits with your doctor’s advice.
3) Keep your air clean
- Avoid smoke, secondhand vape, dust, and harsh fumes. A simple humidifier or a HEPA air purifier at home can make airways feel better.
4) Eat for lung health
- Build meals with fruits, veggies, nuts, and fish. Antioxidants and omega-3s can help support your body’s natural repair processes.
5) Ask about nebulized support if mucus lingers
- Some people feel better using a portable mesh nebulizer like TruNeb™ to inhale sterile saline. Hypertonic saline (3% or 7%) draws water into the airways to loosen thick mucus so it’s easier to cough out. It’s usually used under a doctor’s guidance, especially for asthma or COPD. Nebulized saline supports mucus clearance and comfort; it doesn’t reverse scarring or structural damage.
- If you have wheeze or asthma, your doctor might prescribe a bronchodilator (a medicine that opens your airways) to use with a nebulizer.
Safety note: ⚠️ Talk to your doctor before trying any new medication or nebulized saline. These options support mucus clearance and comfort, but they don’t replace medical care.
When to See a Doctor
⚠️ If you have severe shortness of breath, chest pain, or are coughing up blood, seek emergency medical care right away.
Call your doctor right away if you notice:
- Severe shortness of breath at rest or with very little activity
- Chest pain or pain with deep breaths
- Coughing up blood
- High fever, chills, or signs of pneumonia
- A heavy cough that doesn’t improve after 8 weeks
These can signal problems that need treatment, like infection, an asthma flare, a vaping-related lung injury, or—in rare cases—a collapsed lung; your doctor can determine what’s going on.
Medical care matters here. Mild issues can improve with rest and support, but serious cases sometimes need treatments like oxygen or steroids in a clinic or hospital. If you’re unsure whether your symptoms are serious, it’s safer to call your doctor.
See a doctor if your breathing gets worse instead of better after quitting vaping, or if you have red-flag symptoms like chest pain, high fever, or coughing up blood.
Frequently Asked Questions
These quick answers cover how your lungs heal after quitting vaping and how tools like nebulizers fit in. Tap or click a question below to see the answer:
Many people recover fully, especially if there is no permanent scarring. Because vaping is relatively new, long-term research is still catching up, but early evidence and clinical experience suggest that a wide range of vaping-related changes improve after quitting. If serious injury or scarring occurred, some changes may last.
A short spike in coughing during the first 1–2 weeks is common as cilia clear built-up mucus. By 1–2 months, most people notice far less coughing. If a heavy cough lingers beyond 2–3 months, schedule a visit with your doctor.
Usually yes, because vaping doesn’t leave tar in the lungs the way cigarettes do. That said, data on people who only vaped and never smoked is limited, and individual recovery varies.
You can’t hack healing, but you can support it: hydrate, practice gentle deep-breathing and light cardio, keep your air clean, and eat a produce-rich diet. Ask your doctor about tools like nebulized saline if mucus is stubborn.
It can help with symptoms and medication delivery. A portable mesh nebulizer like TruNeb can deliver saline or prescribed medicine right to your airways. Saline can thin mucus so you can clear it more easily. Nebulizers support comfort and mucus clearance—they don’t heal scar tissue or erase underlying damage. Use hypertonic saline under your doctor’s guidance.
Always check with your doctor before starting any new treatment.
Bottom line: your lungs start healing within days of quitting vaping, and most people see major improvements within the first year. If you’re worried about symptoms or progress, talk to your doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your health concerns, symptoms, and treatment options.