On this page
What Are Hospital Nebulizers vs Home Nebulizers?
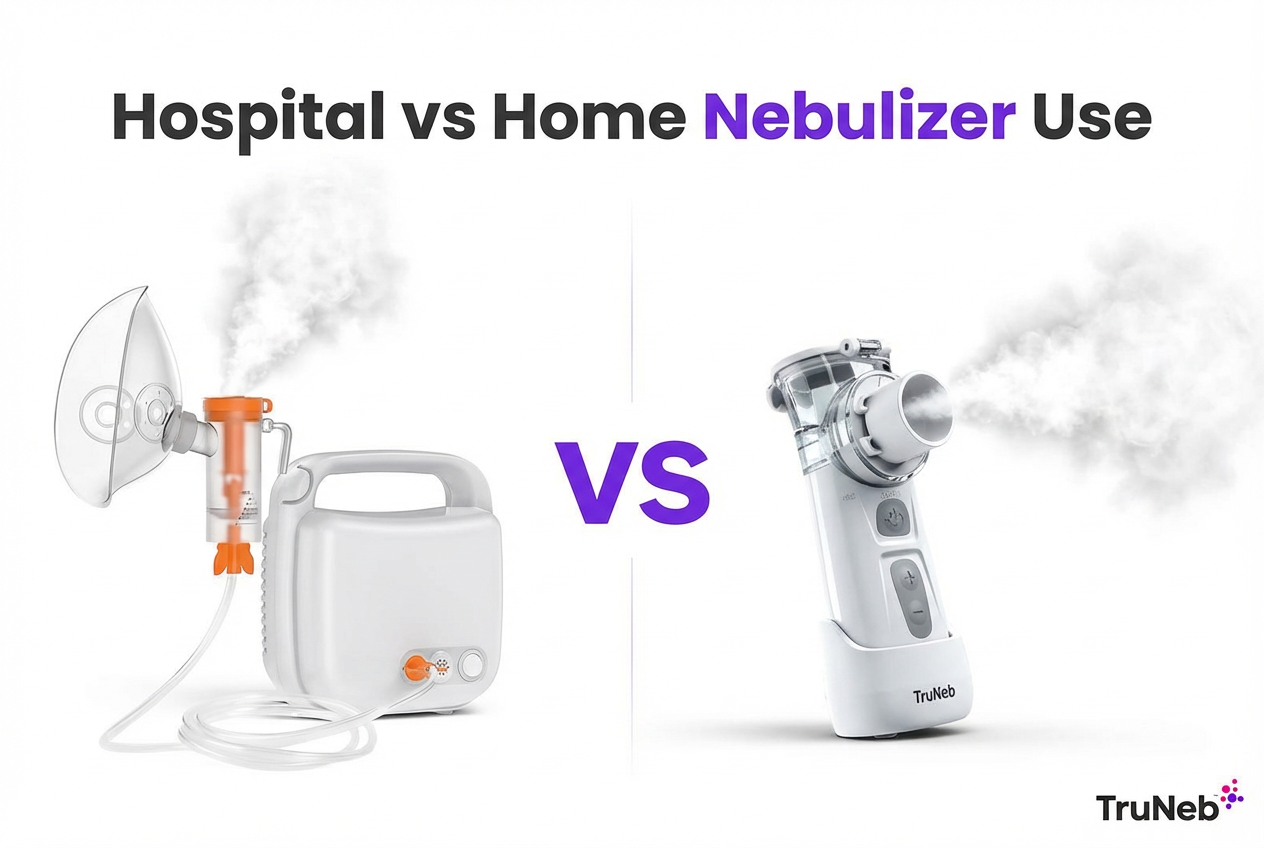
A nebulizer turns liquid medicine into a fine mist you breathe in. A hospital nebulizer is the breathing machine used in ERs and clinics, set up and watched by medical staff. It’s built for fast, high‑demand care.
A home nebulizer is a compact device you use yourself for daily treatment or mild flare‑ups as part of at‑home respiratory therapy. Most people use either a plug‑in tabletop compressor or a small handheld vibrating mesh nebulizer that runs on batteries. You might hear “medical nebulizer” for hospital gear and “household nebulizer” for home devices—they do the same job in different settings.
Doctors use nebulizers for conditions like asthma, COPD, cystic fibrosis, bronchiectasis, and pneumonia. During an acute asthma attack or COPD exacerbation, treatment is usually supervised in the hospital.
Both have the same goal: getting medicine into your lungs, just in different settings with different power, monitoring, and upkeep. ⚠️ Steam inhalers aren’t the same as nebulizers. They’re not meant for breathing prescription medicines and shouldn’t replace your nebulizer treatments.
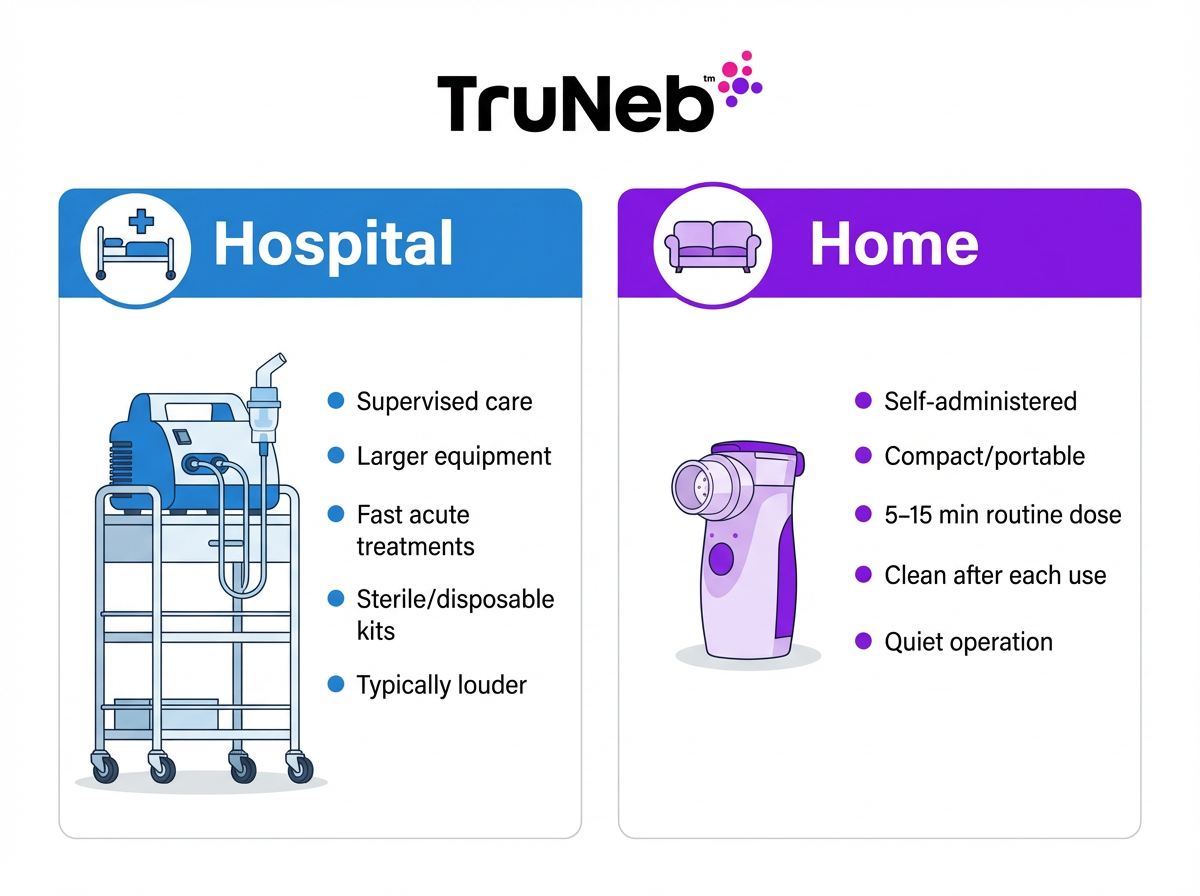
In short: hospital nebulizers are supervised, high‑power devices for acute care; home nebulizers are compact, self‑use devices for daily management.
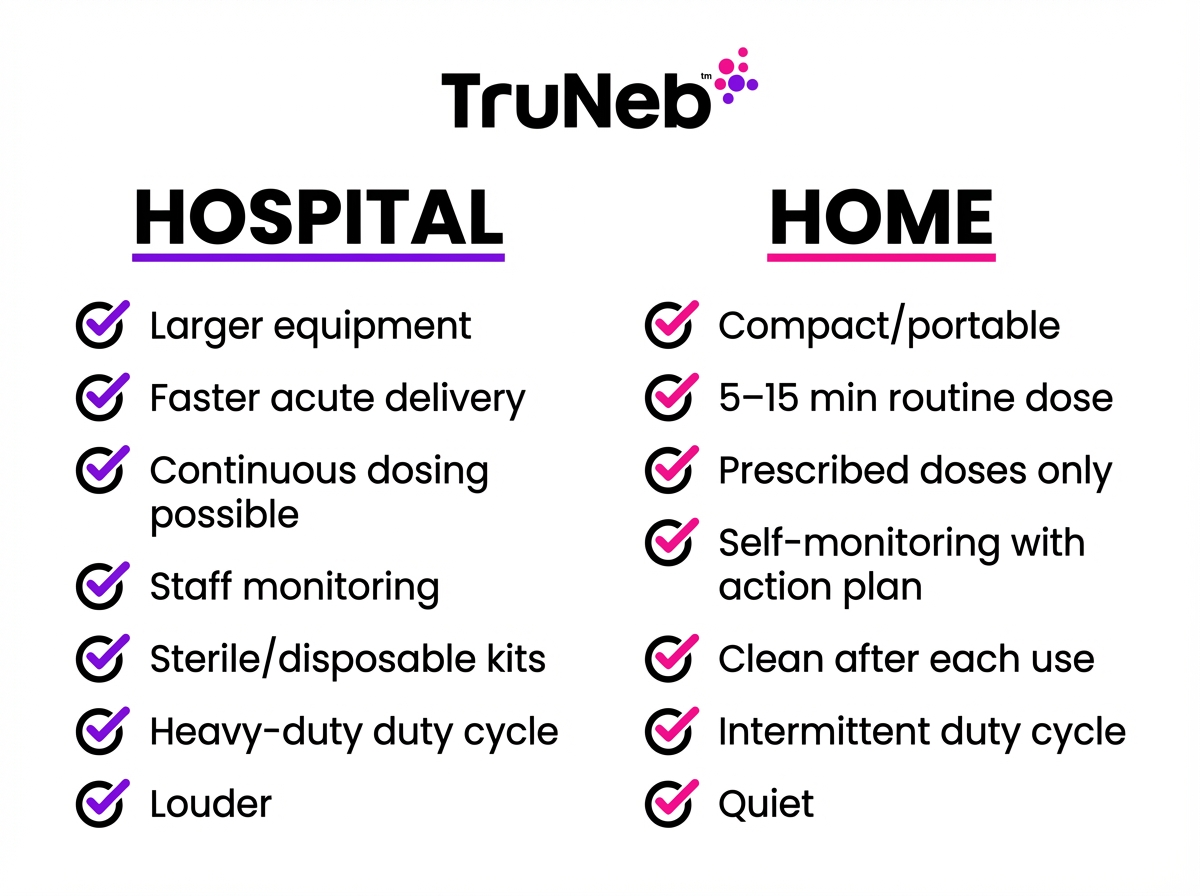
Key Differences Between Hospital and Home Nebulizer Treatments
The goal is the same—getting medicine into your lungs, but the setup and experience are different.
People ask, “Are home nebulizers as effective as hospital nebulizers?” Both can be effective at delivering medicine; the big differences are setting, supervision, and treatment intensity.
| Factor | Hospital Treatment | Home Nebulizer | Why It Matters |
|---|---|---|---|
| Size & Portability | Larger units, wall air/O2, built for all-day use | Tabletop compressors or pocket-size mesh devices | Home gear is easier to carry and store |
| Performance & Particle Size | Strong flow, very fine mist; may include ultrasonic units | Modern mesh produces a fine mist similar to hospital | Finer droplets reach deeper into the lungs |
| Medication & Intensity | Back-to-back or continuous treatments for severe flare-ups | Use exactly what your doctor prescribed on schedule | Hospitals can rapidly escalate care when needed |
| Monitoring | Supervised by nurses/RTs with oxygen and add-on therapies | Self-administered with an action plan | Supervision improves safety during emergencies |
| Safety & Cleaning | Sterile or single-patient kits; strict protocols | Wash, disinfect, and dry parts fully | Reduces germ growth and infection risk |
| Durability & Duty Cycle | Heavy-duty for constant use | Designed for a few sessions a day | Prevents overheating and extends device life |
| Noise & Comfort | Compressors can be louder | Mesh units are very quiet | Quiet devices fit daily routines and sleep |
| Cost & Convenience | Part of a clinical visit; can be costly | Cost-effective for long-term care; fewer trips | Saves time and money over repeated visits |
Size, design, and portability
- Hospital: Larger plug-in systems or wall air/oxygen. They’re built to run all day and be ready in seconds when someone can’t breathe.
- Home: Tabletop compressors or pocket-size mesh nebulizers you can take anywhere.
Power, particle size, and performance
- Hospital machines typically deliver a strong flow and very fine mist for fast, deep delivery. Smaller droplets reach deeper into your lungs, which is why the fineness of the mist matters.
- Hospitals sometimes also use ultrasonic nebulizers, which use sound waves instead of compressed air to create a fine mist quickly.
- Older home compressors can be slower, but modern vibrating mesh devices create a fine mist that’s much closer to what you’d get in the hospital.
Medication dose and treatment intensity
- Hospital: Staff can give back-to-back or continuous treatments and adjust dosing in real time for severe attacks.
- Home: You use the exact medication and dose your doctor prescribed, on a set schedule. Common nebulized medicines include bronchodilators like albuterol, combination meds such as albuterol with ipratropium (e.g., Duoneb), and inhaled steroids like budesonide (e.g., Pulmicort) for long-term control.
That’s why severe asthma or COPD flare-ups are treated in the ER, while mild or early symptoms are usually handled with your home nebulizer as part of your doctor’s plan.
Monitoring and supervision
- Hospital: Nurses or respiratory therapists watch oxygen, pulse, and breathing, and can add oxygen or other treatments right away. That safety net is a big reason serious breathing problems belong in the hospital, not just at home.
- Home: You self-administer and follow an action plan from your doctor.
Safety and infection control
- Hospital: Sterile or single-patient kits and strict cleaning protocols.
- Home: You help prevent germs by washing parts after each use, disinfecting regularly, and drying completely to avoid bacteria or mold.
Device durability and duty cycle
- Hospital devices are made for constant use.
- Home devices are built for a few sessions a day. Some compressors need a cool-down between sessions, while mesh devices avoid motor heat but depend on charged batteries. That “duty cycle” is simply how long a machine can safely run before it needs a rest.
Noise and comfort
- Hospital compressors can be louder, which is fine in urgent care.
- Home mesh units are very quiet, which helps with daily use and sleep routines.
Cost and convenience
- A hospital session is part of a medical visit and can be costly.
- A home nebulizer is usually more cost-effective for long-term management and saves trips, especially with a care plan in place.
This is the key difference in a home nebulizer vs hospital breathing treatment: supervised intensity and monitoring in the hospital versus convenience and self-care at home.
In short: hospitals handle urgent, high-intensity breathing care under supervision; home nebulizers handle regular, self-managed treatment.
When to Use a Hospital Nebulizer vs a Home Nebulizer
Home nebulizers are usually part of routine care and mild‑to‑moderate symptoms that respond to your action plan from your doctor.
Go to the hospital or call emergency care if:
- You have severe trouble breathing (fast breathing, chest pulling in, or you can’t speak full sentences), such as during a severe asthma attack.
- Your lips or fingers look blue or gray.
- You don’t feel better after 1–2 home treatments as directed by your action plan.
- A new or strong reaction (chest pain, faintness, or confusion) appears during a treatment.
⚠️ These are examples, not a complete list. If you’re ever unsure or feel dangerously short of breath, call 911 or your local emergency number right away.
Home care fits best when:
- You are following your doctor’s plan for daily control or early flare‑ups.
- You can sit upright, breathe steadily, and symptoms improve after treatment.
In short: home nebulizers are for day‑to‑day control and early symptoms, while hospitals handle severe breathing emergencies with supervised, high‑intensity treatments.
Bridging the Gap with Modern Portable Nebulizers
New tech makes home treatments faster, quieter, and easier. Vibrating mesh devices create a fine mist without a bulky compressor, so medicine reaches deep airways with less noise and hassle.
Some therapies first used in clinics, like hypertonic saline (extra‑salty saline solution) to thin mucus, can also be part of home care when a doctor approves the dose and schedule. Some people use medical‑grade 3% or 7% hypertonic saline at home—such as TruNeb’s saline vials—only after their doctor reviews the dose and schedule. Hypertonic saline should only be used exactly as prescribed by your doctor; do not mix or adjust it yourself.
The device is one piece; your care plan from your doctor is the other.
In short: portable mesh nebulizers like TruNeb bring hospital‑style mist to daily life, but emergencies still need hospital care.
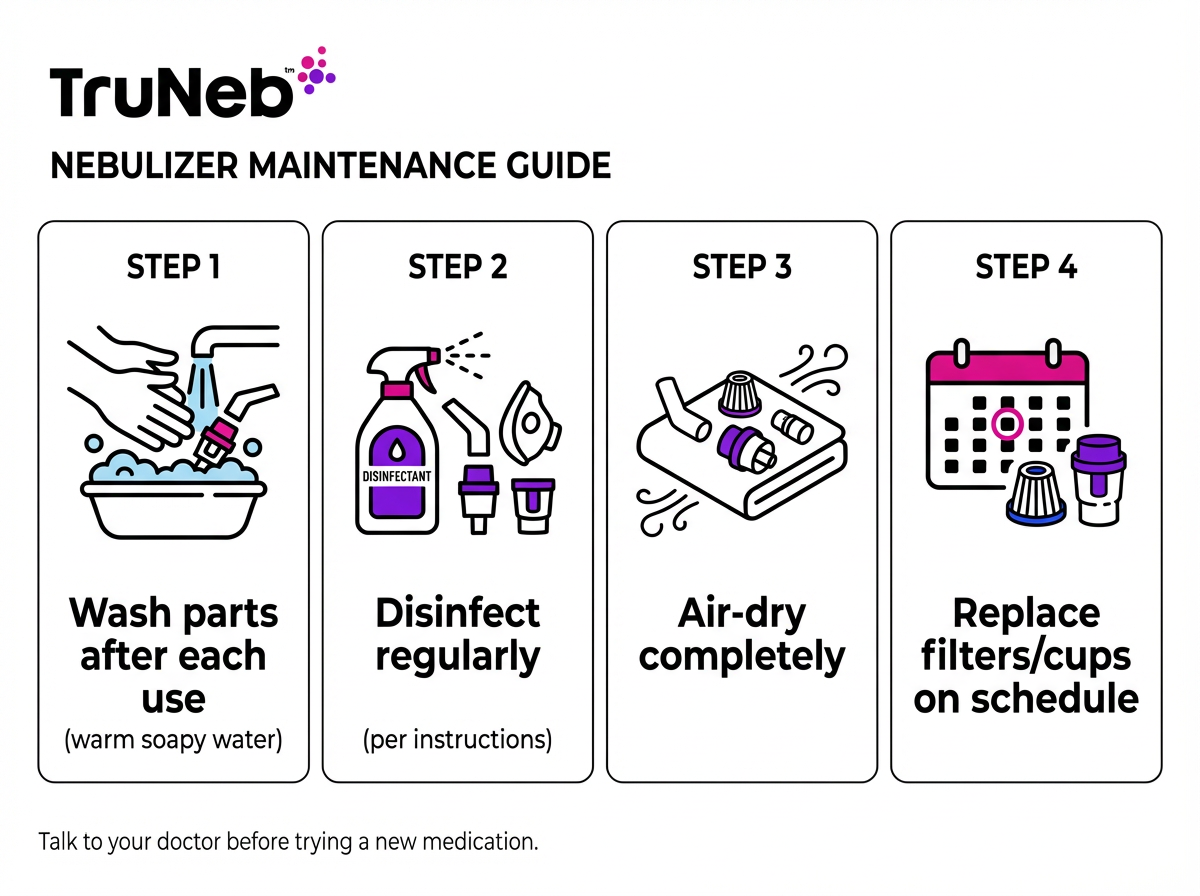
Tips for Safe and Effective Home Nebulizer Use
- Follow your prescription exactly. That includes any prescription bronchodilators or inhaled steroids your doctor ordered.
- Wash the cup and mouthpiece or mask after each use. Then air‑dry fully. Disinfect on a regular schedule. If parts stay wet or dirty, germs can grow and be pushed straight into your lungs next time.
- Replace parts on time. Follow your device instructions for filters, nebulizer cups, and mesh heads.
- Pick a clean spot. Try to nebulize in a smoke‑free, dust‑free area.
- Keep an action plan. Know what to do if symptoms get worse and when to seek help.
- Keep an eye on how you feel. If treatments stop helping or cause new symptoms, contact your doctor.
Safety note: Talk to your doctor before trying a new medication or hypertonic saline. Hypertonic saline should only be used exactly as prescribed by your doctor; do not mix or adjust it yourself. Do not start, stop, or change prescription medicines on your own.
In short: clean gear, follow your plan, and know when to call for help.
Frequently Asked Questions
Tap or click a question below to see the answer:
For daily management of conditions like asthma or COPD, a home nebulizer can work very well when you use it correctly. In emergencies, hospital treatments add close monitoring, higher-intensity dosing, and support like oxygen, so they’re the safer choice for severe symptoms.
Not in emergencies. A home nebulizer supports daily care and early flare-ups per your doctor’s plan. That’s the difference between a home nebulizer vs hospital breathing treatment—the home device is for routine care, the hospital for urgent, supervised treatment.
If you’re struggling to breathe, have blue or gray lips or fingers, can’t speak in full sentences, or your action plan says to seek urgent care, go now. These signs are similar to the red flags listed in the “When to Use” section—any time you see them, treat it as an emergency.
Hospitals commonly use jet nebulizers powered by wall air/oxygen and sometimes ultrasonic nebulizers for quick mist. At home, people use plug-in compressor units and portable vibrating mesh devices.
Clean after each use, disinfect regularly, let parts dry completely, and replace components on schedule. Follow your action plan and call your doctor if symptoms don’t improve.
You typically need a prescription for the medicines, and insurers usually require one for the device. Your doctor will match the device and medication to your condition.
In short: use your home nebulizer for regular, prescribed treatments, and rely on hospital care when symptoms are severe, unpredictable, or not improving.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and any questions about your medications or nebulizer treatments.