On this page

Flu and Asthma: When to Go to the Hospital
If breathing suddenly feels hard, your lips look blue, or your inhaler stops helping, go to the ER right away.
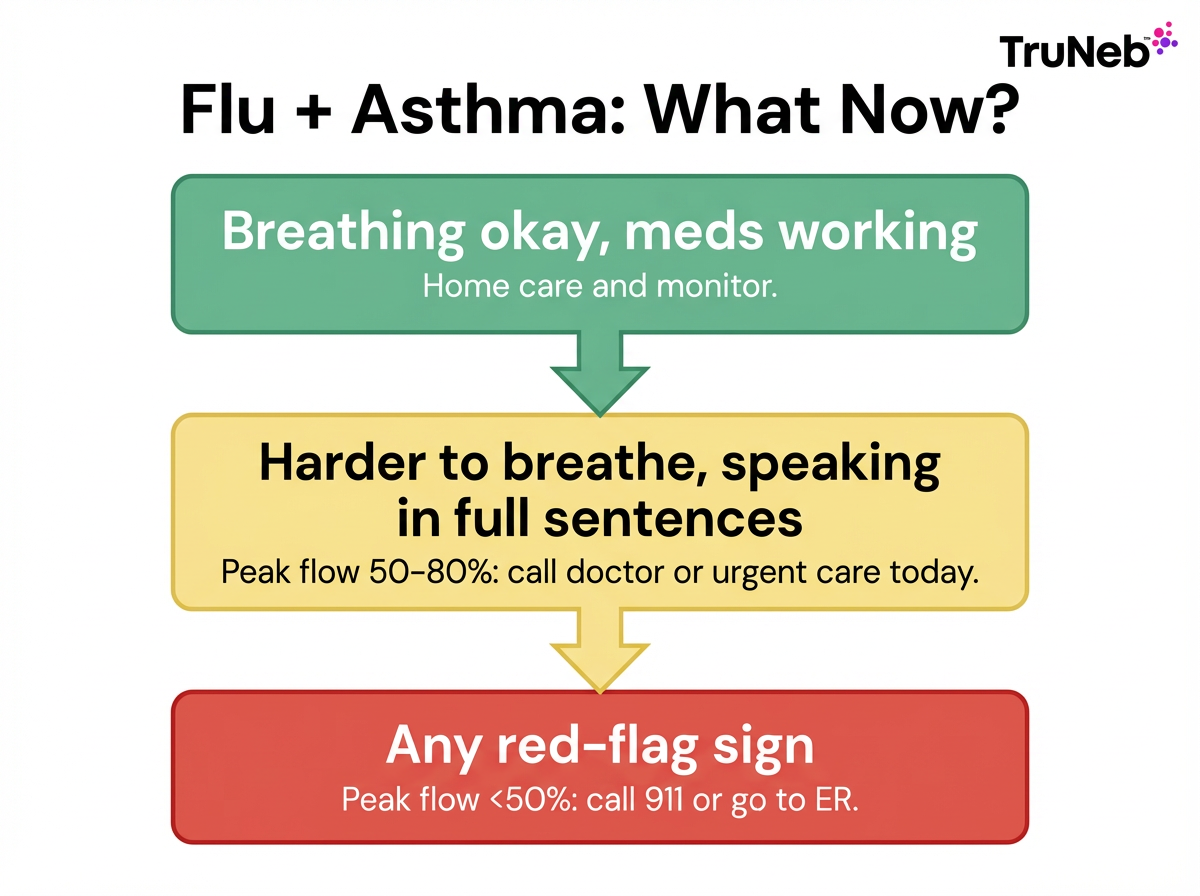
Here’s a clear guide to when to stay home, call your doctor, use urgent care, or go straight to the ER. This guide can help you decide when to seek same-day or emergency care during flu season, but it doesn’t replace advice from your doctor.
Why Flu Is Especially Risky If You Have Asthma
Flu inflames your airways. With asthma, those airways are already sensitive. The swelling and extra mucus can quickly trigger an asthma flare and make breathing much harder. When the flu hits, breathing tubes swell and clog with mucus; with asthma, that narrowing happens faster and air has a harder time moving.
People with asthma are in a high-risk group for flu complications, and groups like the CDC and AAFA say so plainly. Doctors see more ER visits and hospital stays for people with asthma during flu season, including complications like pneumonia. The risk is higher for kids, older adults, and anyone with moderate to severe asthma.
Act early, stick to your Asthma Action Plan, and use the red-flag signs below to decide when to get help.
Flu hits people with asthma harder because it adds swelling and mucus to already sensitive airways, which can quickly make breathing a lot more difficult.
Red-Flag Symptoms: When to Get Emergency Medical Help Immediately
Emergency doctors recommend going to the ER or calling 911 if any of these happen during the flu:
- Breathing is very hard: You can’t speak in full sentences without gasping.
- Blue or gray color: Lips, face, or fingernails turn blue or gray (cyanosis).
- Silent chest: Wheeze stops and your chest sounds quiet even though you’re struggling to breathe. This means very little air is moving, not that your asthma is better.
- Confusion or faintness: You feel dizzy, very drowsy, or not fully alert.
- Chest pain or pressure: Any severe chest pain or tight pressure.
- Very fast breathing: Rapid breaths or using neck and rib muscles to pull in air.
- Quick-relief (rescue) inhaler not helping: Little or no relief after repeated quick-relief doses.
- Peak flow red zone: Less than 50% of your personal best after following your action plan.
- Got better, then got worse: Flu seemed to improve, then your fever and cough came back stronger than before. This can be a sign of pneumonia or another serious complication.
For children, also watch for:
- Fast breathing or ribs pulling in between breaths.
- Cannot drink or signs of dehydration (no tears, very few wet diapers).
- Blue lips.
- Not waking/behaving normally or going floppy.
⚠️ If you have any of these signs, do not drive yourself if you’re very short of breath. Call 911 or your local emergency number.
Bottom line: if you feel like you can’t breathe or something about your breathing feels very wrong, it’s time to get emergency care.

Urgent Care or Doctor: How To Decide Your Next Step
Not every flare needs the ER, but if your symptoms are getting worse, you still need quick attention.
- Go to urgent care if: Breathing is harder than usual but you can still talk in full sentences, walk, and there’s no blue color. Your peak flow is in the yellow zone (about 50–80% of your best) and not improving.
- Call your doctor or use telehealth when: Symptoms are mild to moderate and you’re not in immediate distress; you need advice on meds; or you tested positive for flu and may need an antiviral. In the UK, contact your GP or call 111 for guidance if your reliever isn’t helping or shortness of breath increases.
- Head to the ER right away if: Any red-flag sign appears, symptoms escalate fast, or your gut says something is seriously wrong. If you’ve ever needed ICU care or intubation for asthma, go straight to the ER earlier rather than later.
Rule of thumb: if you’re not sure what to do and your breathing is getting worse, it’s safer to be seen by a doctor the same day.
Telehealth isn’t appropriate if you’re struggling to breathe or have any red-flag signs—use 911 or go to the ER instead.
How To Manage Flu and Asthma at Home
Follow your Asthma Action Plan at the first sign of trouble.
- Use meds as directed: Stay on your controller inhaler. Use your quick-relief medicine exactly as your plan says for illness days.
- Nebulizer support: When you feel weak or congested, a portable mesh nebulizer can make breathing treatments easier to take. A device like the TruNeb™ Portable Mesh Nebulizer is handheld, so you can rest while taking your prescribed medication, if your doctor has recommended nebulized treatments. It supports daily management, but it never replaces emergency care.
- ⚠️ If you see products labeled "steam inhaler", remember these are not nebulizers and shouldn’t be used to breathe in prescription asthma medications.
- Mucus help with guidance: Some clinicians use nebulized hypertonic saline (3% or 7%) to loosen thick mucus. In simple terms, it’s a salty mist you breathe in that helps thin and move mucus. Do this only if your doctor recommends it and tells you how to use it safely. This article isn’t telling you to start hypertonic saline on your own—only your doctor can decide if it’s right for you and how you should use it.
- Rest, fluids, and comfort: Sleep, hydrate well, and use fever reducers as advised. Warm liquids can help thin mucus.
- Watch your numbers: Check peak flow twice a day. A drop often shows up before you feel much worse.
Safety note: Talk to your doctor before trying a new medication.
In short, manage flu and asthma at home by following your action plan, using your prescribed treatments as directed, resting, and watching your numbers so you can act fast if things start to change.
Stay Ahead With Prevention and a Ready Plan
A few steps now can lower your risk later.
- Get your flu shot every year: Doctors generally recommend that people with asthma get a flu shot each year. Ask close contacts to get vaccinated, too.
- Ask about the pneumococcal (pneumonia) vaccine if your doctor recommends it.
- Reduce exposure: Wash hands, avoid crowded indoor spaces during peak season, and stay home when sick.
- Tune up your plan: Review your Asthma Action Plan with your doctor and keep rescue meds and your nebulizer ready.
- Set up follow-up: After any ER or urgent visit, book a check-in to update your plan.
Flu and pneumococcal vaccines lower the chance of severe lung infections that could trigger dangerous asthma flares.
Staying vaccinated, keeping your asthma plan up to date, and having your medicines and nebulizer ready can greatly lower your chances of a flu-related asthma emergency.
Frequently Asked Questions
These quick answers pull together the key signs, steps, and tools to help you stay safer when flu and asthma collide. Tap or click a question below to see the answer:
Go to the ER for severe breathing trouble (you can’t speak in full sentences), blue or gray lips or nails, or chest pain or confusion. If your quick-relief inhaler isn’t helping or your peak flow drops into the red zone, that’s an emergency, too. See the Red-Flag Symptoms section above for the full checklist.
Choose urgent care if you’re breathing harder but can still talk in full sentences, have no blue color, and your peak flow is about 50–80% of your best. Go straight to the ER or call 911 if any red-flag sign appears or symptoms are rapidly getting worse.
A dangerous flare shows bigger breathing limits: trouble talking, needing your inhaler very frequently with little relief, or a sharp drop in peak flow into the red zone. Use your peak flow meter and your Asthma Action Plan to guide next steps.
Only as directed in your action plan or by your doctor. If you need treatments more frequently than prescribed or they’re not helping enough, that’s a sign to seek medical care. Talk to your doctor before trying new treatments or hypertonic saline.
Flu commonly triggers symptoms in people with asthma, but how much it worsens breathing varies. Plan for it to affect your lungs, act early with your action plan, and get help fast if red-flag signs appear.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, treatment options, and when to seek emergency care.