On this page

Epiglottitis is a sudden throat infection that swells the epiglottis, the flap that guards your airway. Swelling can block breathing within hours. This is an emergency.
Croup is a common viral illness that inflames the voice box and windpipe. It causes a barky cough and a harsh, high-pitched breath sound called stridor. Most cases are mild and improve over a few days with simple care.
Clear signs help you act fast and get the right help.
Rule of thumb: Epiglottitis threatens the airway fast; croup often sounds scary but is usually manageable.
Why It’s Critical to Distinguish Croup from Epiglottitis
Both can cause stridor, the harsh, high-pitched sound on breathing in. But the stakes are very different. Epiglottitis can close the airway quickly and needs 911 and hospital care. It is now rare in vaccinated children because of the Hib vaccine, but it still happens.
Croup is common in toddlers and preschoolers. It usually follows a cold and gets better with calming and a steroid ordered by a doctor. Mistaking epiglottitis for simple croup can delay emergency care and put a child’s life at risk. Croup is usually mild, but worsening breathing or stridor at rest needs medical attention.
A fast way to think about it: Drooling and sitting forward to breathe is a 911 sign. A barky cough after a runny nose points to croup.
Telling croup from epiglottitis matters because epiglottitis can block a child’s airway within hours, while croup is usually milder and treatable without emergency surgery.
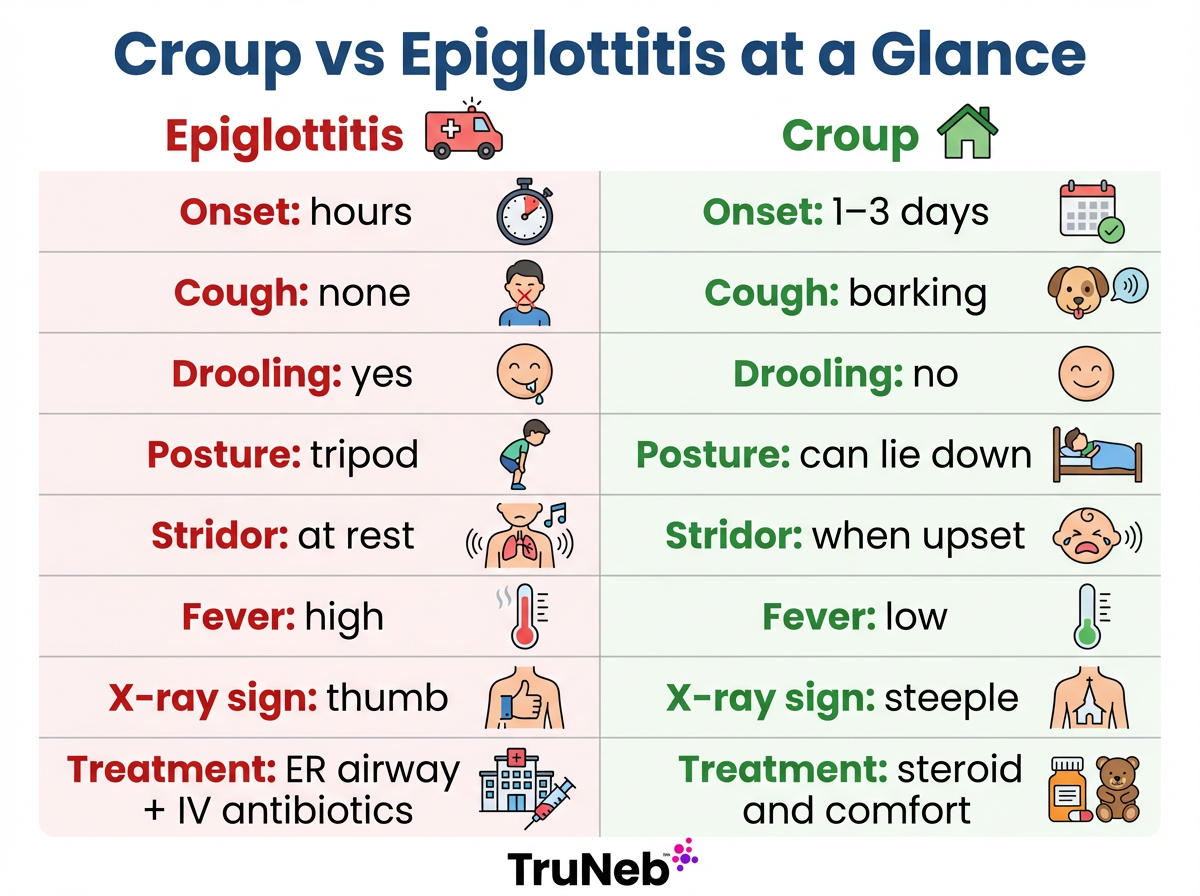
Use this quick chart to see the epiglottitis vs croup differences at a glance.
Croup vs Epiglottitis: Key Differences at a Glance
| Feature | Epiglottitis | Croup |
|---|---|---|
| Onset | Very sudden, within hours | Gradual, after 1–3 days of cold symptoms |
| Typical age | School-age children, teens, and adults; rare in fully vaccinated young children | 6 months to 3 years common |
| Fever | High | Low or mild |
| Cough | Little or none | Barking, seal-like |
| Voice | Muffled or very quiet | Hoarse cry or voice |
| Swallowing / drooling | Painful swallowing; drooling | Swallows saliva; no drooling |
| Stridor pattern | Even when calm; can become softer as the airway narrows | Mainly when crying or upset |
| Posture | Leans forward in the classic tripod position with drooling; dislikes lying down | Prefers upright, but can lie down |
| Appearance | Very ill, anxious, “toxic” (appears extremely sick) | Uncomfortable, usually not toxic |
| X-ray sign | Thumb sign (swollen epiglottis) | Steeple sign (narrow windpipe) |
| Cause | Bacterial (commonly Hib or other bacteria) | Viral (commonly parainfluenza) |
| Treatment needed | Emergency hospital care with airway protection and IV antibiotics | Single-dose steroid; calm care; ER epinephrine if severe |
Key takeaway: A barky cough favors croup; drooling with tripod posture favors epiglottitis.
Note: “toxic” means the child looks extremely sick.
Signs and Symptoms – How to Recognize Each Condition
Below is how epiglottitis symptoms vs croup symptoms usually look in real life.
Epiglottitis
Epiglottitis starts fast. A child can have a very sore throat, high fever, and trouble swallowing. Drooling happens because swallowing is too painful or blocked by swelling. The voice can sound muffled or very quiet. Breathing can be noisy even at rest. Children sit upright and lean forward to breathe. They look extremely sick and can panic if you try to make them lie down.
Croup
Croup usually begins like a regular cold with a runny nose and mild or no fever. Then the classic barky cough appears, typically worse at night. The voice is hoarse. Stridor happens mainly when the child is crying or upset and eases when calm. Most kids can drink, swallow saliva, and be consoled.
In short, epiglottitis usually looks worse than it sounds; croup usually sounds worse than it looks.
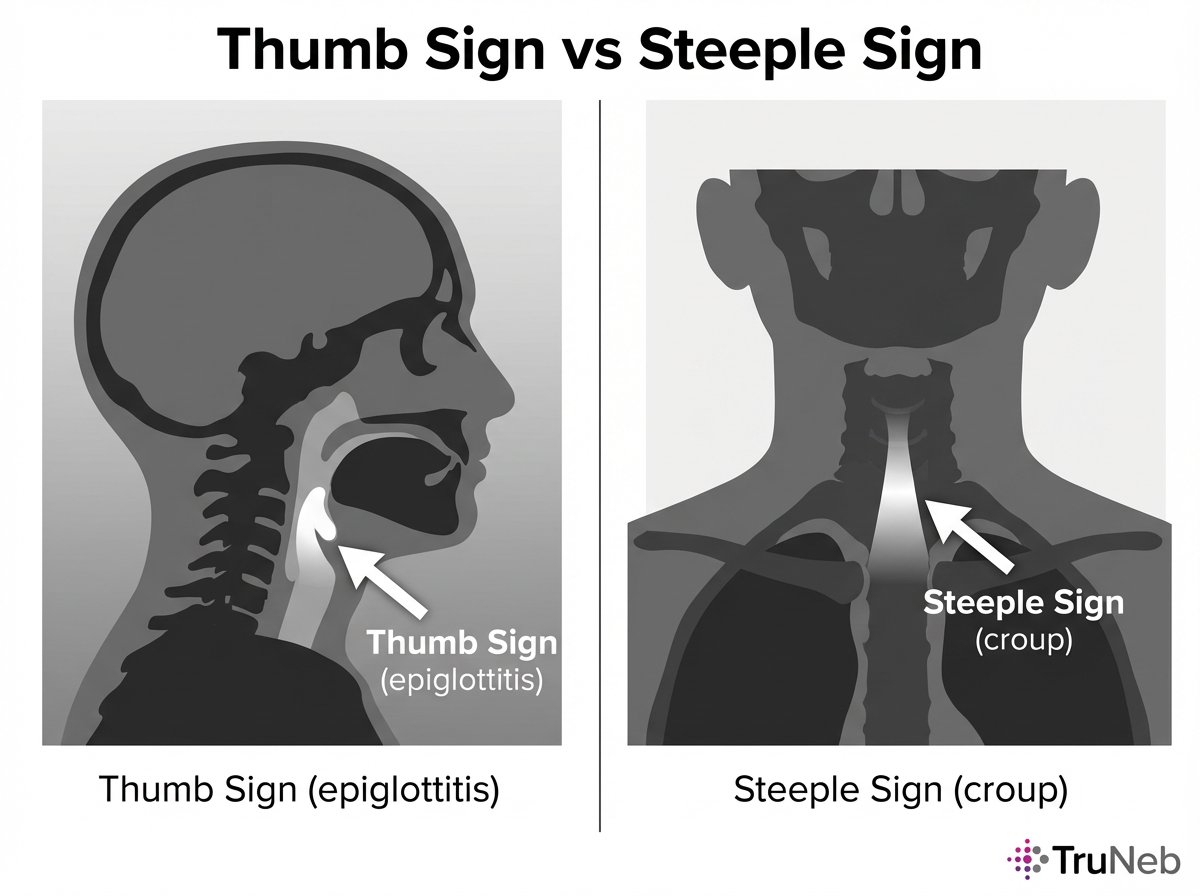
Thumb Sign vs Steeple Sign – What X-Rays Show
Doctors sometimes use a neck X-ray to support the diagnosis—this is what an epiglottitis vs croup X-ray can show. In epiglottitis, a side-view X-ray can show a swollen epiglottis that looks like a thumb. In croup, a front-view X-ray can show a narrow windpipe below the voice box that looks like a steeple.
Doctors decide if an X-ray is needed; you don’t need to request specific imaging.
Key point: If epiglottitis is suspected, do not delay airway care for imaging.
Croup vs Epiglottitis vs Tracheitis – Understanding All Three
Bacterial tracheitis is a rare, serious infection of the windpipe (commonly Staph aureus) that can follow viral croup or start on its own. Children usually have a high fever, look very ill, and have a harsh, wet cough with thick mucus. Stridor and breathing trouble are common, but drooling is less typical than in epiglottitis. It tends to affect slightly older children and can act like “bad croup” that does not improve with usual croup treatments. It needs urgent hospital care, antibiotics, and airway support.
Unlike epiglottitis, drooling is less common in tracheitis; unlike typical croup, the child usually looks very ill and doesn’t improve with usual croup treatment.
Simple clue: Tracheitis can look like severe croup that is not getting better.
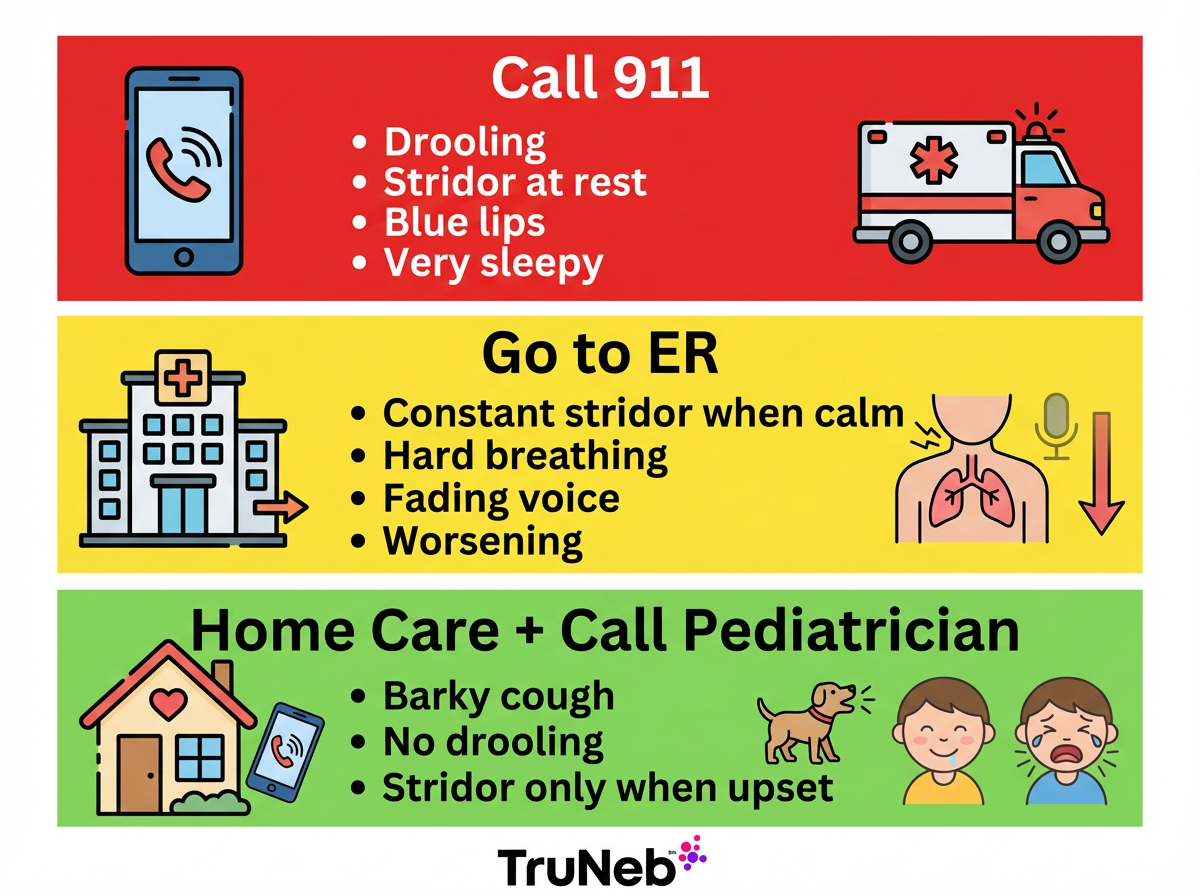
When to Worry: Stridor Action Plan
Most croup is mild, but some signs mean you need help right away. Stridor is that harsh, high-pitched noise when your child breathes in.
- Call 911 immediately: drooling or cannot swallow, stridor at rest with obvious struggle, lips or face turning blue, very sleepy or limp.
- Go to the ER now: stridor continues when calm, hard or fast breathing that does not ease, chest or neck skin pulling in with each breath (retractions), voice fading or barely heard, you are worried and symptoms are not improving.
- Manage at home and call your pediatrician: barky cough with no drooling, stridor only when upset and it settles when calm, drinking well and alert.
If you’re unsure which category your child fits, it’s safest to seek urgent medical care.
Safety note: Talk to your doctor before trying a new medication. If you suspect epiglottitis, skip home treatments and seek emergency care now.
In short, drooling, stridor at rest, blue lips, or extreme sleepiness are 911 signs, while a barky cough without drooling can usually be watched at home with your doctor’s guidance.
Treating Epiglottitis: Emergency Care Comes First
Epiglottitis is treated in the hospital right away. The first priority is protecting the airway. In a controlled setting, specialists such as anesthesiologists or ENT surgeons secure the airway with a breathing tube under sedation when needed. IV antibiotics are started, and the child is closely watched in the ICU. Fluids and medicines to reduce swelling can be used. With prompt care, most children recover well.
Epiglottitis treatment focuses on rapidly securing the airway in the hospital and giving IV antibiotics until the swelling goes down.
Do not try to treat suspected epiglottitis at home.
Managing Croup at Home – What Helps and When to See the Doctor
Keep your child calm and upright; crying makes stridor louder. Cool mist or brief cool night air can help mainly because it calms and soothes your child.
Your child’s doctor might prescribe a single dose of dexamethasone to reduce swelling; it usually helps within a few hours. In moderate or severe cases, ER teams give nebulized epinephrine and monitor. Most croup improves over 3–4 days. Antibiotics do not help because croup is viral. Only use medicines your child’s doctor has prescribed; don’t give leftover steroids or other medications without medical advice.
Most croup improves over a few days with calming care at home and a single steroid dose from your child’s doctor.
Nebulizers, Saline, and Chronic Care – Where They Fit In
Home nebulizers are not a primary fix for croup’s upper-airway swelling. In clinics and ERs, teams use nebulized epinephrine for short relief under monitoring. At home, a nebulizer helps if your child also has wheezing illnesses like bronchiolitis or asthma, when a doctor prescribes the medicine.
Croup vs bronchiolitis matters here: croup affects the upper airway, while bronchiolitis affects the lower airways (the small breathing tubes in the lungs), so treatments and the role of a nebulizer differ. Hypertonic saline can be used in some hospitals for bronchiolitis under a doctor’s guidance. A quiet portable mesh device like the TruNeb™ Portable Mesh Nebulizer can make prescribed bronchodilators or saline easier to take while your child sits upright and calm.
Important: steam inhalers are not nebulizers and should not be used to deliver prescription medications. A home nebulizer cannot fix the throat swelling in epiglottitis and should never delay emergency care. Only use nebulizer medicines that your child’s doctor has prescribed for them.
Home nebulizers mainly help deliver medicines for lower-airway problems like asthma or bronchiolitis, not the upper-airway swelling of croup or epiglottitis.
Frequently Asked Questions About Croup and Epiglottitis
This FAQ covers the most common questions parents ask about how croup and epiglottitis differ and when to seek help.
Tap or click a question below to see the answer:
A barky cough without drooling points toward croup. Drooling, trouble swallowing, and a very quiet or muffled voice—especially with tripod posture—suggest epiglottitis and need urgent care.
Yes. Epiglottitis can block the airway quickly and needs emergency care. Croup is usually mild and improves with simple care and a steroid from your child’s doctor.
No. Croup is usually diagnosed by history and exam. For suspected epiglottitis, doctors protect the airway first and only do imaging or scopes in a controlled setting when it’s safe. Never try to look at your child’s throat at home if you’re worried about epiglottitis; forcing the mouth open can make breathing worse.
It means a child sits upright, leans forward, and supports themselves with their hands. With drooling, it signals they’re working hard to breathe and is a red flag for epiglottitis.
Croup comes from cold viruses and spreads like a cold. Epiglottitis is typically caused by bacteria such as Hib, and vaccination has made it rare. Close contacts of a Hib case sometimes receive preventive antibiotics from a doctor.
No. They are different infections. Croup is viral. Epiglottitis is bacterial and uncommon in vaccinated children.
Adults rarely get croup because their airways are larger; the same viruses more often cause laryngitis. Adults can get epiglottitis, which is treated as an emergency.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about any questions you have about a medical condition or your child’s symptoms. If you think you are experiencing a medical emergency, call 911 right away.