On this page
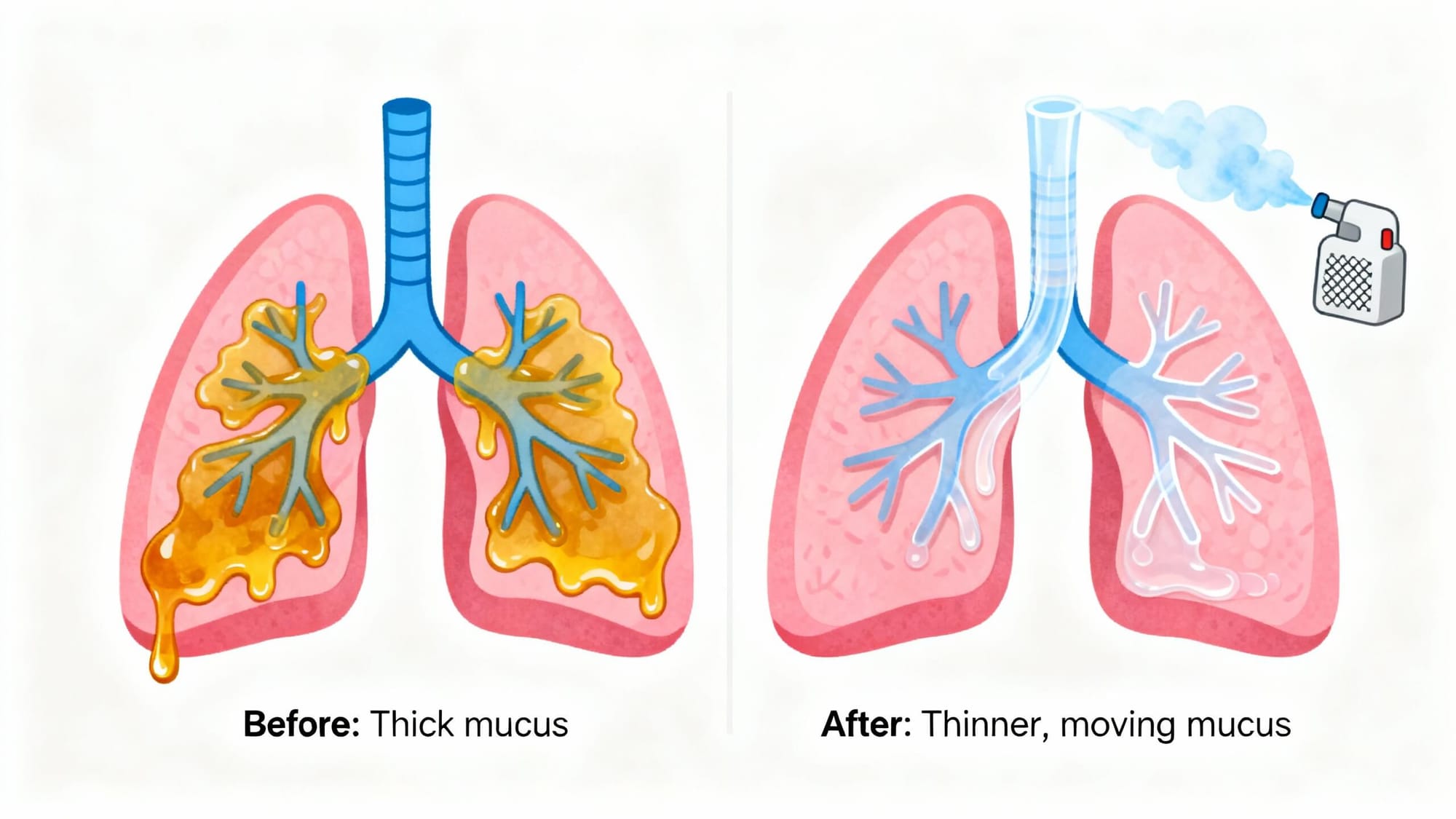
Yes, a nebulizer can help loosen lung mucus so you can cough it out. It turns liquid into a fine mist that you breathe in. That moist mist reaches deep into your airways and can thin sticky phlegm. The mist helps your lungs’ cilia move loosened mucus upward so you can cough it out.
Moisture loosens the gunk so your lungs’ cilia and a good cough can move it up and out.
Key idea: a nebulizer doesn’t make mucus vanish; it helps your body clear it.
How Nebulizers Help Clear Lung Mucus
- A nebulizer makes a cool, fine mist you inhale through a mask or mouthpiece.
- Moisture can thin thick secretions and make coughing more effective.
- Opening tight airways with certain medicines can make your cough work better, too.
This natural cleanup is called mucociliary clearance, where tiny hair-like cilia sweep mucus up toward your throat so you can cough it out. If you cough more right after a session, mucus is likely moving. With chronic lung conditions like COPD, bronchiectasis, or cystic fibrosis, regular airway-clearance routines can help reduce mucus plugs.
Tip: Sitting upright and taking slow, deep breaths, holding for 1–2 seconds before exhaling, can help the mist reach deeper.
Inhaling saline mist adds moisture that thins sticky mucus so your cough can move it out.
What to Put in a Nebulizer for Mucus Relief
Nebulized Saline (0.9%)
Sterile saltwater adds moisture to your airways. This can thin mucus and ease coughing. It’s commonly used and is gentle for most people.
Hypertonic Saline (3%–7%)
Higher-strength saltwater draws extra water into thick mucus, which can loosen stubborn phlegm so it’s easier to clear. It’s commonly used in cystic fibrosis and bronchiectasis care, and some people use it with a bronchodilator if their lungs are sensitive (doctor-directed). It can trigger coughing and, in some people, airway irritation.
Bronchodilators (for example, albuterol)
These medicines open tight airways. They do not chemically thin mucus, but by opening the pipes, they can help you move mucus out with a better cough.
Other medications
Prescription mucolytics are condition-specific, such as acetylcysteine (Mucomyst) and dornase alfa for cystic fibrosis. Use these only under a doctor’s direction.
Only use sterile, neb-ready vials. Don’t use tap water. Never put essential oils or homemade mixtures in a nebulizer, and note that steam inhalers are not for medications.
Saline thins mucus; bronchodilators open airways but don’t chemically thin it.
Nebulizer vs Humidifier: Which Helps With Mucus?
Use a nebulizer for targeted lung delivery; use a humidifier to moisten room air for general comfort.
| Device | What it does | Best use | Reaches | Delivers meds/saline | Cleaning needs |
|---|---|---|---|---|---|
| Nebulizer | Aerosolizes sterile saline or medication for inhalation | Chest mucus, wheeze, targeted lung delivery | Deep airways | Yes — neb-ready saline and prescribed meds | Wash parts after each use; disinfect per maker |
| Humidifier (room) | Adds moisture to room air | Dry air, mild congestion, nose/throat comfort | Mostly upper airways | No | Clean tank regularly; prevent mold |
Note: Do not put medications, essential oils, or homemade mixtures into humidifiers or steam inhalers—they are not designed for drug delivery. Use only sterile, neb-ready saline or prescribed solutions in a nebulizer.
Make Your Nebulizer Work Better: Simple Techniques
- Sitting upright and taking slow, deep breaths, holding for 1–2 seconds, can help the mist reach deeper.
- A few huff coughs right after a session can help move mucus up.
- Chest clapping or a vibrating airway-clearance device can help if your care team has shown you how. Some people also use positive expiratory pressure (PEP) devices (Acapella or Flutter) as taught by a clinician.
- Side-lying positions for drainage can help if your doctor recommends them.
- Drink water after to soothe your throat and keep mucus thin.
Breathe slowly, then do a few huff coughs right after the treatment to bring mucus up.
Using a Nebulizer for Kids
- Saline nebulization can help little ones cough out mucus more comfortably, including during colds or bronchiolitis.
- Use a mask, keep them upright, and make it calm with a story or video.
- If a medication was prescribed for wheeze or asthma, follow the pediatric plan exactly.
- If your child is crying hard, pause and soothe—crying reduces effective inhalation.
- Expect some coughing after the treatment, that can be a good sign.
If your child is working hard to breathe, isn’t drinking, or seems worse, seek care right away.
For kids, saline nebulization can make coughing out mucus more comfortable—use medications only if prescribed.
Aftercare: Dos and Don’ts
- Do: Clean your nebulizer parts with warm soapy water, rinse, and air-dry.
- Do: Cough and spit out mucus after your session.
- Do: Drink water to keep secretions thin.
- Do: Use only sterile, neb-ready saline vials; don’t use tap water.
- Don’t: Share masks or mouthpieces without thorough cleaning.
- Don’t: Add oils or homemade mixes to the cup.
- Don’t: Start new medications without talking to your doctor.
- Don’t: Overuse medications beyond your plan.
Freshly treated airways can be sensitive. If cold air bothers you, cover your mouth and nose when you go outside.
Clean your nebulizer after every use and avoid adding anything not made for nebulizers.
When to See a Doctor
⚠️ Call 911 or seek emergency care now if breathing is very hard, lips or face turn blue, you feel confused, or you can’t speak in full sentences.
- High fever, chest pain, or bloody mucus.
- Breathing that is very hard, fast, or noisy.
- Symptoms that don’t improve after several days of proper treatments.
- Repeated mucus blockages or frequent infections.
- For infants and toddlers: poor feeding, dehydration signs, or labored breathing.
If a nebulizer isn’t helping after a few days, talk to your doctor. These signs can mean you need a different plan or testing.
If breathing is very hard or symptoms don’t improve after a few days, get medical help.
A Portable Option That Fits Real Life (TruNeb™)
The TruNeb™ portable mesh nebulizer is small, quiet, and easy to pack, so you can do saline sessions at home or on the go. That kind of flexibility helps keep your routine steady when you’re traveling, working, or caring for a child.
Note: Use only neb-ready saline or prescribed meds, and follow your care plan.
Frequently Asked Questions
Tap or click a question below to see the answer:
It helps loosen and move mucus so you can cough it out. The device doesn’t erase mucus; your cough clears it.
Not directly. Albuterol opens airways so you can breathe and cough better. Saline is what adds moisture to thin secretions.
For very thick mucus, hypertonic saline (3%–7%) can loosen secretions more. Some people find it irritating; ask your doctor.
A nebulizer gives targeted lung delivery. A humidifier moistens room air. Many people use both—nebulizer for chest mucus and humidifier for comfort.
Follow your plan; your clinician will set the frequency for your condition. Do not exceed what your prescriber recommends.
Yes. A portable mesh unit fits in a carry-on; bring saline ampoules and spare batteries if needed.