On this page
Does COPD Get Worse After You Quit Smoking?
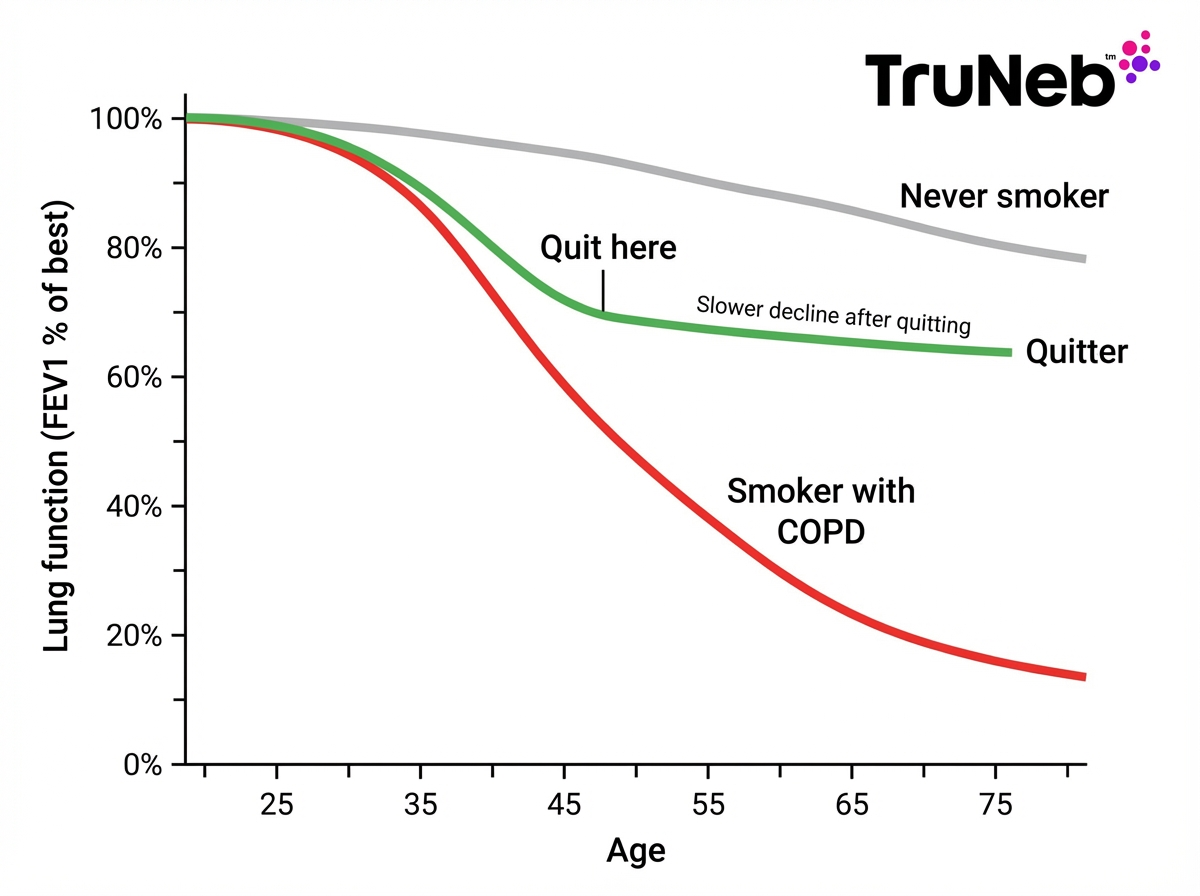
Yes. COPD still progresses over time, but quitting smoking slows it way down. COPD is a chronic, progressive disease. Damage that already happened doesn’t reverse. But when you stop smoking, you remove the main driver that speeds it up.
Think of it like hitting the brakes on a downhill slope. You won’t roll back uphill, but you can slow the drop a lot and protect the lung function you still have.
Whether your COPD is mainly chronic bronchitis or emphysema, research shows that after quitting, the steep decline in lung function becomes much gentler, closer to normal age-related decline. Lung function—often measured as FEV1 on spirometry—still goes down with age, but the slope flattens after you quit. That shift can mean more years of steadier breathing, fewer flare-ups, and a better day-to-day life.
Key takeaway: Quitting doesn’t reverse COPD, but it sharply slows how fast it gets worse.
How Quitting Smoking Changes the Course of COPD
Smoking cessation stops the daily smoke exposure that keeps your airways inflamed. Over time, swelling eases, cilia (the tiny cleaners in your airways) work better, and your lungs face fewer irritants. That helps you breathe easier and keeps COPD from worsening as fast.
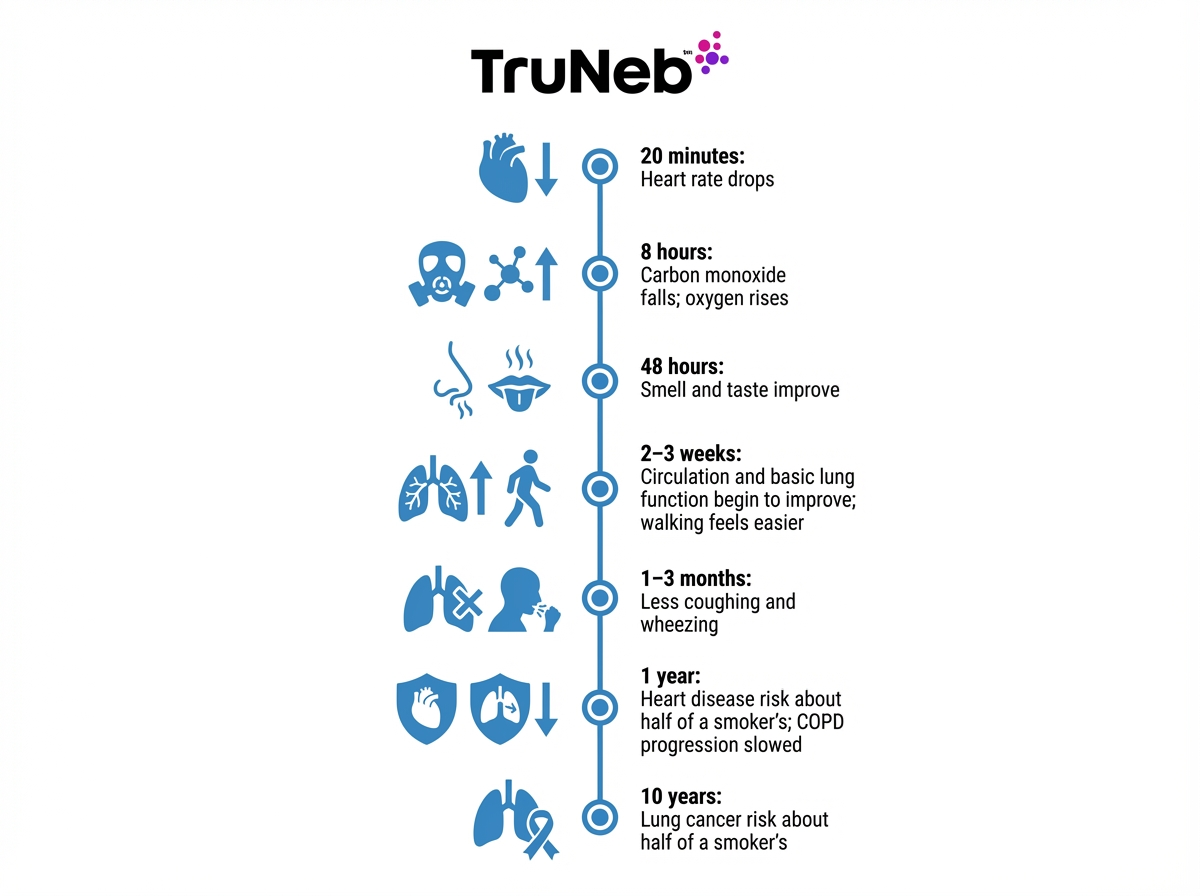
Quitting also lowers your risk of flare-ups (exacerbations), hospital stays, and serious illness. People who quit after a COPD diagnosis can improve their life expectancy compared with those who keep smoking. Smokers are about 12 times more likely to die from COPD than people who never smoked; quitting moves you off that high-risk path. Former smokers still have higher risk than never-smokers because of past damage, but it’s far lower than if you continued to smoke. In short, COPD progression after quitting smoking slows dramatically.
Here’s a quick comparison:
Quitting smoking slows COPD progression, reduces flare-ups and hospitalizations, and can improve your life expectancy compared with continuing to smoke.
| Outcome | Keep smoking | After you quit |
|---|---|---|
| Lung function decline | Faster, steeper drop | Slower, gentler slope |
| Exacerbations (flares) | More frequent and severe | Fewer and less severe on average |
| Hospitalizations | Higher risk | Lower risk |
| Life expectancy | Shorter | Improved compared with continuing to smoke |
| Daily symptoms | Worse cough, mucus, and breathlessness | Less cough and mucus, breathing feels easier |
Note: Results vary by COPD stage, other health conditions, and how closely you follow your treatment plan.
In short: remove the smoke, reduce the damage, and your decline slows.
Key takeaway: After you quit, COPD’s decline slows and your odds of flares and early death drop.
Improvements to Expect After Quitting Smoking
Some changes show up fast. Within hours, carbon monoxide in your blood drops and oxygen levels rise. Within days, smell and taste improve. In a few weeks, a lot of people notice it’s a bit easier to walk, climb stairs, or do chores without getting as winded. Over months, coughing and mucus can lessen as your airways calm down.
Improvements vary by COPD stage and other health conditions.
A heads-up: you might cough more for a few weeks right after quitting. That’s your lungs clearing out gunk. It usually settles, then gets better.
Quitting won’t restore destroyed air sacs, so breathing won’t return to “like new.” But the big win is this: shortness of breath stops worsening so quickly, and your stamina usually improves with time and activity. These symptom gains are part of why quitting is linked to longer life in COPD.
Key takeaway: A lot of people with COPD feel some breathing improvements within weeks of quitting, and their future lung decline usually slows down.
Why COPD Can Still Progress After Quitting
Some damage is permanent. COPD includes scarring and destroyed air sacs that don’t grow back. Even without smoke, those changes affect airflow.
Aging also plays a role. Everyone’s lung function slowly declines with age. With COPD, that normal decline starts from a lower point.
Other factors matter, too. Ongoing exposure to secondhand smoke, dusty air, chemical fumes, or heavy pollution can still irritate your lungs. Infections and flare-ups can cause stepwise drops in lung function that may not fully recover. And some people have genetic risks (like Alpha-1 antitrypsin deficiency, a genetic condition that can damage the lungs) that drive COPD on their own.
Progression is usually slower if you quit in mild or moderate stages than in very severe disease, but quitting helps at all stages.
The good news: most of these factors can be managed. Avoid irritants, prevent infections, and follow your care plan to keep progression as slow as possible.
Key takeaway: Past damage, aging, exposures, and flares can still nudge COPD forward after you quit.
How to Keep COPD from Getting Worse After Quitting
Quitting is step one. Daily habits and smart care help you keep your lungs as steady as possible.
Here are some key steps:
- Take your prescribed medications the right way.
- Clear mucus so it doesn’t clog or get infected.
- Stay active with gentle, regular exercise.
- Prevent infections and triggers in your environment.
Build or review a COPD action plan with your doctor so you know what to do if symptoms change.
Key takeaway: Quitting is step one; daily habits and care keep COPD as steady as possible.
Adhere to Your Medications and Treatment Plan
Keep taking your COPD medications as prescribed. Maintenance inhalers help keep airways open and calm. A lot of people find they use their rescue inhaler less frequently once they’ve been smoke-free for a while, which is a good sign—but always keep it nearby. Quitting can also make inhalers and other COPD medicines work better because the airways are less irritated by smoke.
Use the right technique. A spacer can help inhaled medicine reach your lungs. If you struggle with inhalers, a nebulizer can turn medicine into a fine mist you breathe in at a relaxed pace. Portable mesh nebulizers like the TruNeb™ portable mesh nebulizer are small, quiet, and battery-powered, so it’s easy to take treatments at home or on the go.
If you’re unsure how to use an inhaler or nebulizer, ask your doctor or pharmacist to review your technique.
If your doctor has prescribed oxygen, keep using it as directed. Quitting makes oxygen use safer and more effective.
Key takeaway: The right meds work better after quitting, but only if you take them correctly.
Keep Your Airways Clear
Thick mucus can block airflow and lead to infections. Clearing it helps you breathe easier.
Key steps:
- Staying well-hydrated can help thin mucus.
- Controlled coughing techniques can help bring mucus up, especially in the morning.
- Ask your doctor about airway clearance tools (like flutter or OPEP devices) if you have a lot of phlegm.
Some doctors recommend inhaling hypertonic saline with a nebulizer to draw water into the airways and loosen mucus. For example, 3% or 7% saline via a portable nebulizer can help you cough out stubborn secretions once your clinician says it’s right for you. Hypertonic saline isn’t right for everyone (it can trigger bronchospasm in some people), so it must be prescribed and monitored by your doctor.
Safety note: Only use hypertonic saline or new therapies under your doctor’s guidance. Frequent or worsening mucus build-up is a reason to revisit your treatment plan with your doctor.
Key takeaway: Thinner, moving mucus means fewer blocks, fewer infections, easier breaths.
Stay Active with Pulmonary Rehab and Exercise
Pulmonary rehab teaches safe exercise, breathing skills, and daily strategies. It can boost your stamina and quality of life.
Aim for regular, gentle activity. Start with short walks and build up. Use pursed-lip breathing: breathe in through your nose, then exhale slowly through puckered lips for twice as long. This helps keep airways open. Light strength work for arms and legs also helps.
Moderate exercise is generally considered safe for people with stable COPD and can lessen symptoms. Ask your doctor how to start if you haven’t been active, and avoid extreme heat, cold, or poor air quality days.
Key takeaway: Regular, gentle exercise trains your body to breathe easier with COPD.
Prevent Infections and Flare-Ups
Respiratory infections can trigger COPD flare-ups and speed decline. Protect yourself.
Key steps:
- Stay up to date on recommended vaccines (like flu and pneumonia) as recommended by your doctor.
- Wash your hands regularly and avoid close contact with people who are sick.
- Keep your home smoke-free, and limit dust, fumes, and harsh chemicals.
- Check air quality; on bad days, stay indoors or wear a well-fitted mask.
- Have a COPD action plan so you know what to do if symptoms suddenly worsen.
⚠️ If you have severe trouble breathing at rest, chest pain, blue lips or face, or confusion, call emergency services or go to the ER right away.
Contact your doctor promptly if your shortness of breath gets worse quickly, your mucus increases or changes color, or you develop fever or chills.
Catching problems early and avoiding triggers helps you stay stable.
Key takeaway: Fewer infections mean fewer setbacks and a slower COPD decline.
FAQs About COPD Progression After Quitting
Note: This information is educational and not a substitute for medical care. Talk to your doctor before changing any treatment.
Tap or click a question below to see the answer:
No. COPD damage is permanent, so quitting can’t regrow healthy lung tissue. But quitting prevents ongoing smoke irritation and can improve cough and shortness of breath.
It’s never too late. Stopping at any stage slows the disease’s progression and can help you feel and function better.
A lot of people notice easier breathing within weeks because inflammation drops and airways work better. You may not gain back lost capacity, but you can slow future decline and tend to feel more stamina.
Yes. Studies show people who quit after a COPD diagnosis have a lower risk of death than those who keep smoking; quitting can improve your life expectancy compared with continuing to smoke.
Continuing to smoke leads to faster lung function decline, more flare-ups and hospitalizations, and a higher risk of death compared with quitting. Stopping smoking shifts you to a slower decline and fewer setbacks.
Take your medications as prescribed, stay active (pulmonary rehabilitation helps), clear mucus, and prevent infections and triggers like smoke and poor air. Work with your doctor on a COPD action plan.
Key takeaway: Quitting slows COPD; smart daily care helps keep it steady.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options.