On this page
What Is Pulmozyme and Why Do CF Patients Use It?
Pulmozyme (dornase alfa) is a mucus-thinning medication used in cystic fibrosis (CF). You breathe it in with a nebulizer. It works like tiny scissors that cut up extra DNA in thick mucus, so the mucus gets thinner and easier to cough out.
It’s prescribed as part of a daily airway routine. It doesn’t replace airway clearance, it helps make airway clearance work better. Pulmozyme is FDA‑indicated for CF.
One-liner: Pulmozyme is a nebulized enzyme that thins CF mucus so airway clearance can remove it more easily.
The HFCWO Vest - How Chest Physiotherapy Helps Clear Mucus
The vest (high-frequency chest wall oscillation, or HFCWO) gently squeezes and releases your chest many times per second. Those vibrations loosen mucus from the airway walls so you can cough it up.
A typical vest session lasts about 20 to 30 minutes. People commonly do it once or twice a day, and more during flare-ups. The vest is one type of airway clearance technique (ACT). Others include manual percussion and devices you blow into. Timing matters because medicines that thin mucus can make the vest session more effective.
One-liner: A chest physiotherapy vest vibrates your chest to loosen mucus so you can cough it out.
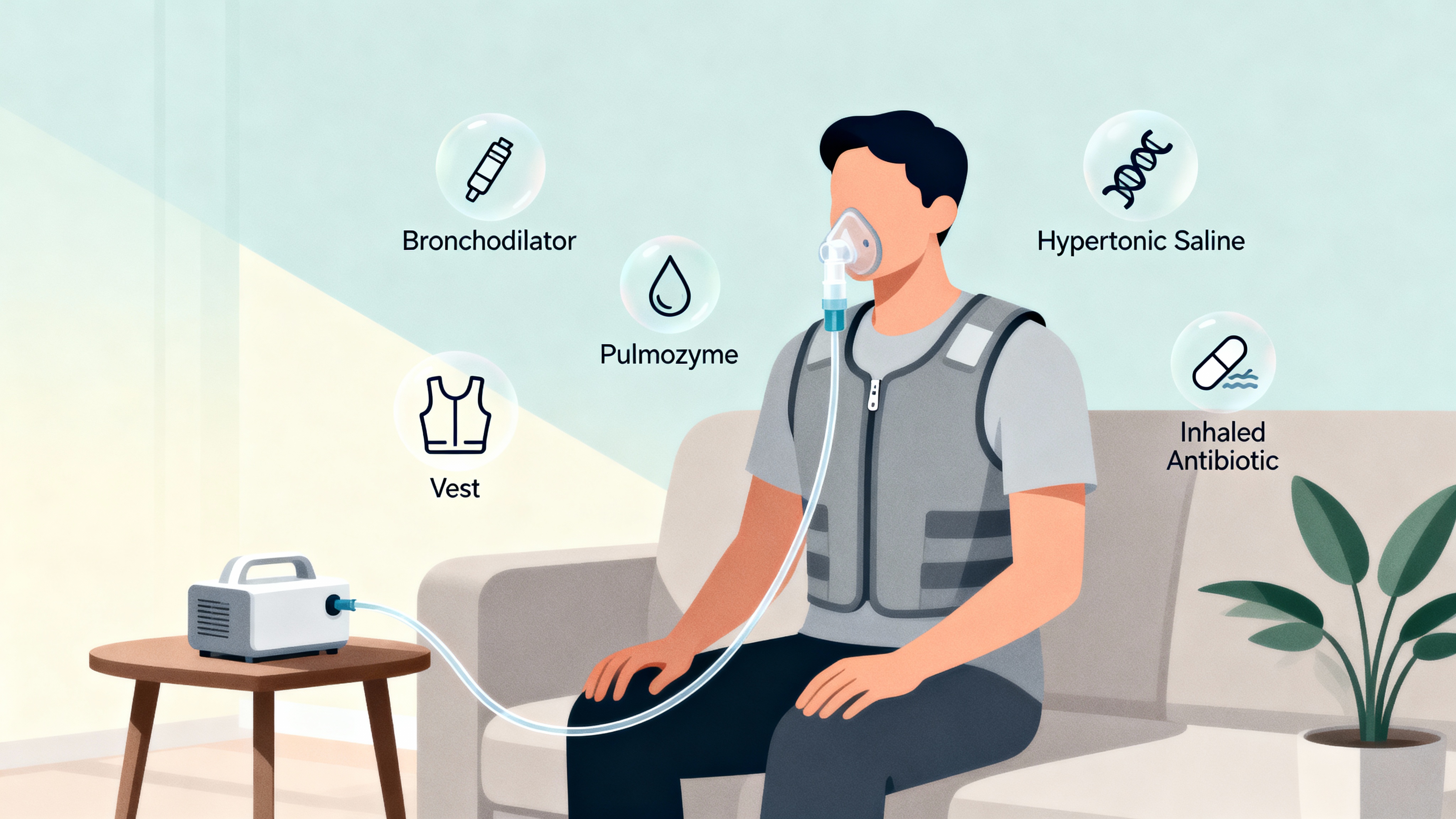
Standard CF Respiratory Treatment Order (Where Does Pulmozyme Fit?)
Here’s the common order CF teams teach. It helps open the airways, thin mucus, clear it out, and then let antibiotics reach deeper.
- Bronchodilator first (like albuterol) to open airways.
- Hypertonic saline to hydrate and loosen mucus.
- Pulmozyme to thin sticky mucus.
- Airway clearance (vest or other ACT) to move mucus out.
- Inhaled antibiotic last (like tobramycin or aztreonam) so it stays in the lungs longer.
Some clinics allow hypertonic saline and Pulmozyme during vest time to save time. Others prefer Pulmozyme a little before airway clearance. Your CF team can tailor this to you.
One-liner: Open airways, thin mucus, clear it, then inhale antibiotics last.
| Step | Therapy | Purpose | Vest at same time? |
|---|---|---|---|
| 1 | Bronchodilator (e.g., albuterol) | Open airways | Yes* |
| 2 | Hypertonic saline | Loosen/hydrate mucus | Yes* |
| 3 | Pulmozyme (dornase alfa) | Thin sticky mucus | Yes† (ideal: 20–30 min before ACT) |
| 4 | Airway clearance (vest or other ACT) | Move mucus out | — |
| 5 | Inhaled antibiotic | Treat airway bacteria | No — do after clearance |
* If your CF team approves, many clinics allow combining vest with bronchodilator and hypertonic saline to save time. † For maximal thinning, some teams suggest inhaling Pulmozyme 20–30 minutes before airway clearance. Always follow your clinic’s guidance.
Pulmozyme Before or After Vest? Finding the Optimal Timing
Most CF teams recommend taking Pulmozyme before airway clearance, then giving it a bit of time to thin mucus so your vest can clear more.
What the guidance suggests: A short wait between the neb and the vest (about 20–30 minutes) is typically suggested when it fits your schedule. Some reports suggest doing Pulmozyme before airway clearance can improve airflow measures compared with after; your team can help you decide what matters for you.
Real-world practice: If your schedule is tight, using the vest during your Pulmozyme neb can still help. Staying consistent each day matters more than a perfect gap every time. If you’re unsure which method helps you cough out more mucus, ask your clinic to help you test both approaches.
One-liner: Best case, Pulmozyme before vest with a short wait; practical case, vesting during your Pulmozyme neb is generally acceptable.
Benefits and Drawbacks of Vesting During Your Pulmozyme Nebulizer
Pros
- Saves time: Doing both together can shave about 10–15 minutes off a session.
- Supports consistency: Shorter sessions can make it easier to stick with daily care.
- Convenience: One setup, one seating, fewer transitions.
Cons
- Slight trade-off in timing: Pulmozyme can thin mucus more if given a short head start before clearance.
- Comfort and coordination: The vest’s vibration can make holding the neb or pacing breaths a bit harder; you may need brief pauses to cough.
- Preference matters: Some people simply feel better doing steps one at a time.
Tip: Some people find a middle ground, like finishing the Pulmozyme neb and starting the vest right away.
One-liner: Combining Pulmozyme and vest saves time and can boost adherence, with a small timing trade-off for some.
How to Use Pulmozyme with Your Nebulizer
Follow your care team’s directions. Here’s a simple step-by-step you can adapt:
- Wash hands and set up your nebulizer kit.
- Use one Pulmozyme ampule as prescribed when you’re ready to treat. Don’t mix Pulmozyme with other medicines in the cup.
- If prescribed, use your bronchodilator first to open airways.
- Use an approved jet nebulizer/compressor system listed in the Pulmozyme instructions. Pour the Pulmozyme into the nebulizer cup and start the compressor. Breathe slow, deep breaths through the mouthpiece until the mist stops.
- If you’re vesting during the neb, use a comfortable setting and pause to cough as needed.
- If you didn’t use the vest during the neb, start your airway clearance right after.
- Clean the neb parts right away per your equipment’s instructions, and let them air dry.
- Store unopened Pulmozyme ampules as directed in the medication instructions.
Device notes
- Pulmozyme should be used with approved jet nebulizer/compressor systems listed in the medication instructions. Check device compatibility with your clinic.
- Steam inhalers are not nebulizers and aren’t for breathing medications.
- For other inhaled medicines, a portable mesh nebulizer can be convenient for travel and quiet use.
One-liner: Keep it simple—set up, neb Pulmozyme, clear mucus, then clean your gear every time.
Safety Note
Talk to your doctor before trying a new medication, changing your treatment order, or combining therapies in a new way. Your CF team can tailor timing to your lungs, your schedule, and your other meds.
If you have severe shortness of breath, chest pain, wheezing that doesn’t settle, signs of an allergic reaction (rash, swelling, trouble breathing), or you cough up blood, seek emergency care. If your symptoms don’t improve, or you’re thinking about changing the timing or order of your treatments, talk to your CF team.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes—most teams allow vesting during Pulmozyme to save time; if possible, inhaling Pulmozyme before airway clearance with a short wait can help it thin mucus first.
About 20–30 minutes is typically suggested so the enzyme can thin mucus before clearance.
Both thin and loosen mucus. Most plans put bronchodilator first, then hypertonic saline, then Pulmozyme, then airway clearance. Your team can adjust this based on how you respond.
Most clinics say yes. It can save time and still help move mucus.
No. Inhaled antibiotics usually go last, after airway clearance, so the medicine can stay in your lungs.
Wrap-Up: Make a Plan You Can Stick With
You can vest with Pulmozyme. For best effect, some teams suggest giving Pulmozyme a little time before airway clearance. If combining helps you finish daily care, that can be a smart choice too. The most important thing is a routine you can keep. Ask your CF team to help you fine-tune your timing.
One-liner: Pick the sequence you can stick with and confirm the plan with your CF team.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice. Always talk with your doctor about your health and treatments.