On this page

Do Nebulizers Help with Croup?
Yes, nebulizers can help croup, but only with the right medicine and usually in a medical setting. In the ER, doctors sometimes use a nebulizer to deliver epinephrine, which can quickly shrink swelling in the voice box and ease noisy breathing. The effect is short-lived, so children are watched for a few hours afterward. For most kids, the gold-standard treatment is a single dose of dexamethasone that reduces airway swelling over a few hours. A nebulizer is just the delivery tool; the medication inside is what matters for croup.
What Is Croup and Why Breathing Gets Hard
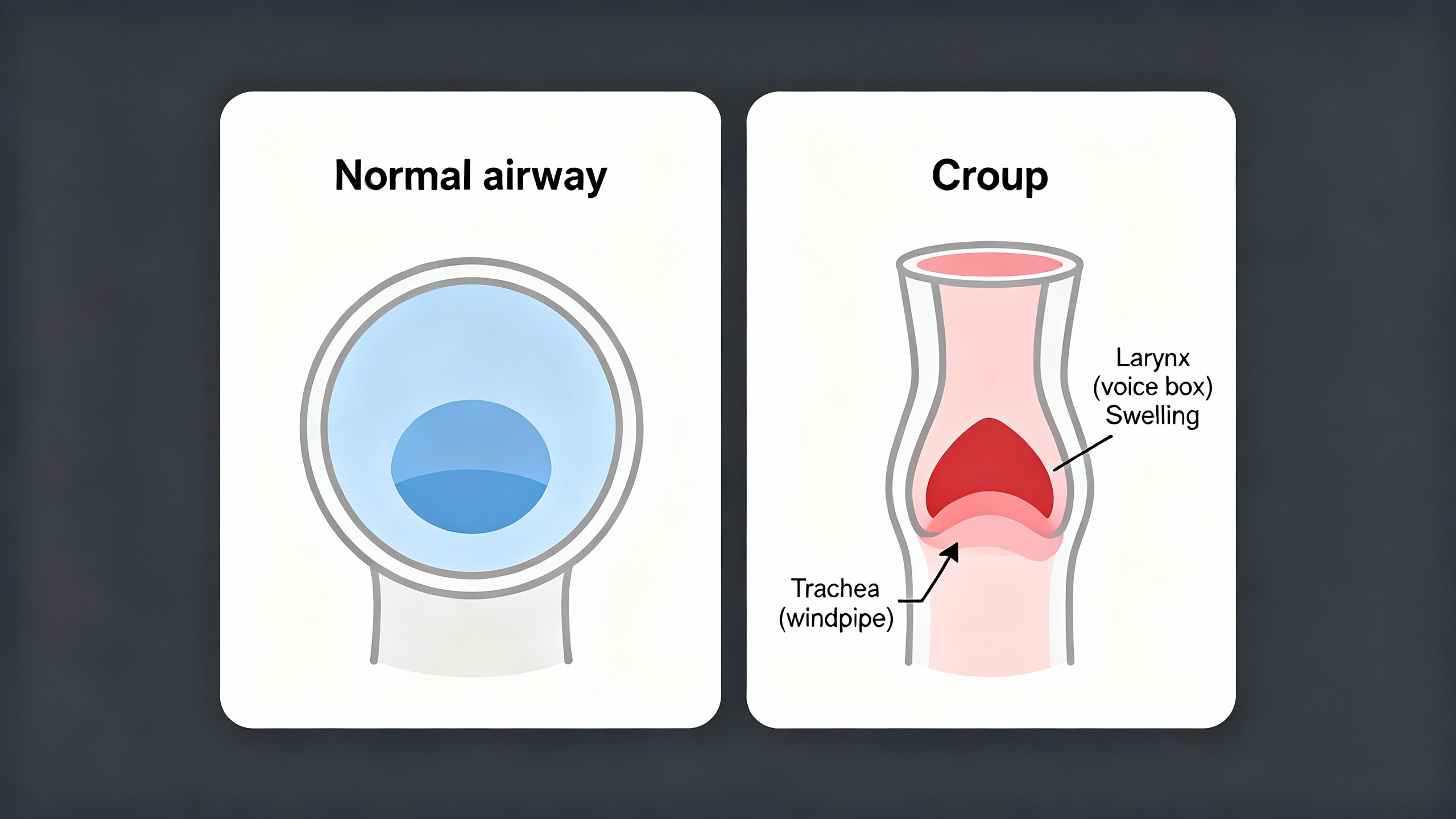
Croup is a viral infection (usually parainfluenza) that causes swelling in the upper airway—the larynx (voice box) and trachea (windpipe). That swelling leads to the classic barking cough, hoarse voice, and a harsh, high-pitched sound when breathing in called stridor. Symptoms usually get worse at night and improve over 3–5 days. Croup is most common in toddlers and preschoolers.
When the airway narrows, it’s like trying to breathe through a smaller straw. Treatments that reduce swelling make it easier for air to pass. Croup is a viral infection that swells the voice box and windpipe, causing a barky cough and stridor.
Fast Facts: 📌
- Croup is upper-airway swelling (larynx and trachea) with barking cough and inspiratory stridor (BMJ Clinical Evidence).
- A single dose of dexamethasone helps at all severities and starts working in about 2–3 hours (American Family Physician).
- Cool or humidified air may soothe, but trials show no clear outcome benefit (American Family Physician).
- Most cases improve within 3–5 days and are most common in toddlers (BMJ Clinical Evidence).
Home Treatment for Mild Croup
- Keep your child calm. Crying can make stridor louder. Hold them, speak softly, and distract with a quiet story or song.
- Try cool or humidified air. Use a cool-mist humidifier in the room, sit in a steamy bathroom for 10 minutes, or step outside into cool night air for a few minutes. Studies show mixed results, but a lot of parents find these options soothing.
- Avoid steam inhalers for meds. You might see boxes labeled "steam inhaler" — these are NOT for breathing medications.
- Offer fluids regularly. Small, frequent sips of water, breast milk, or formula can help comfort and prevent dehydration.
- Help them rest upright. Sitting up can make breathing feel easier; some parents sleep nearby to keep an eye on symptoms.
- Treat fever or discomfort if needed. Ask your doctor about fever reducers and the right dosing for your child.
What not to do: Over-the-counter cough and cold medicines do not help croup in young children.
Bottom line: Calm plus cool or moist air usually brings mild croup relief within 20–30 minutes while you wait for prescribed medicine to work.
The Gold-Standard Treatment: Dexamethasone
Doctors commonly give a single dose of dexamethasone for croup. It reduces swelling in the upper airway and can lower the chance of returning for care. It works for mild, moderate, and severe cases.
- What it does: Lowers inflammation in the voice box and windpipe.
- How it’s given: Usually an oral liquid; sometimes an injection if the child is vomiting or very distressed.
- When it helps: Most children improve within 2–3 hours, and the effect can last 24–72 hours.
A one-time dose of dexamethasone reduces airway swelling within a few hours and is the gold-standard treatment for croup.
Nebulizers and Croup: What Actually Helps
A nebulizer is just the delivery tool; the medication determines whether it helps croup.
Nebulized Epinephrine (ER/Clinic Use)
Nebulized epinephrine (commonly racemic epinephrine) can quickly ease severe croup by shrinking swollen airway tissue. Relief can start within minutes and typically wears off in about 2 hours. That’s why children are observed for a few hours after treatment and might need a repeat dose. Side effects can include a brief fast heartbeat or jitteriness, and medical staff monitor closely.
Epinephrine by nebulizer doesn’t cure the virus. It buys time while the steroid (dexamethasone) kicks in.
What About Albuterol?
Albuterol is a bronchodilator used for asthma because it relaxes the lower airways in the lungs. Croup is an upper-airway problem at the voice box. Because of that, albuterol usually doesn’t help croup’s barky cough or stridor. Using it without a doctor’s guidance can cause side effects (like jitteriness) without benefit.
Note on home devices: A portable nebulizer like TruNeb™ can deliver doctor-prescribed medications. For croup, the effective nebulized medicine in severe cases is epinephrine, which is generally given in the ER with monitoring. If your child has other conditions (like asthma), your pediatrician might prescribe medications for home use in a device like TruNeb.
Optional alternative: Nebulized budesonide (a steroid) can help when a child cannot take medicine by mouth, but studies show oral dexamethasone works just as well and is less distressing for children.
Bottom line: For croup, epinephrine via nebulizer is an emergency tool; albuterol generally isn’t helpful.
Treatment options at a glance
| Treatment | Main purpose | Onset | Where used | Notes |
|---|---|---|---|---|
| Dexamethasone (steroid) | Reduce airway swelling | 2–3 hours; lasts 24–72 hours | Clinic/ER; sometimes at home (prescribed) | Gold standard for all severities |
| Nebulized epinephrine | Shrink swollen tissue quickly | Minutes; wears off ~2 hours | ER/clinic with monitoring | Observe after dose; may repeat |
| Albuterol (bronchodilator) | Relax lower lung airways | Not effective for croup | Not recommended for croup | Consider only if wheeze from lower airways |
| Nebulized budesonide | Reduce airway swelling | Similar to dexamethasone | Clinic/ER if oral meds not possible | Oral dexamethasone is equally effective |
| Cool/humidified air | Comfort measure | May soothe within minutes | Home | Evidence mixed; safe to try |
Note: Albuterol targets the lower airways (asthma); croup is swelling of the upper airway, so albuterol typically doesn’t help.
Hospital Care for Severe Croup: What to Expect
In the ER, the team will keep your child calm, give dexamethasone if not already given, and use nebulized epinephrine if breathing is hard or stridor happens at rest. Because the epinephrine effect is temporary, the team will observe your child for a few hours and give another treatment if symptoms return.
Support care can include oxygen if oxygen levels are low and IV fluids if drinking is hard. Rarely, very severe cases might need heliox or even intubation to protect the airway, but that’s uncommon.
In the ER, kids usually receive dexamethasone and nebulized epinephrine with a short observation period, and most go home the same day.
When to Go to the ER
⚠️ If your child has stridor at rest, blue or gray lips, drooling, or is working hard to breathe, seek emergency care now.
- Stridor at rest (noisy breathing even when calm or sleeping)
- Working hard to breathe (fast breathing, chest/neck retractions, can’t speak or cry normally)
- Blue or gray lips or fingertips
- Drooling or trouble swallowing (possible other serious airway problem)
- Very sleepy, hard to wake, or unusually agitated
- Symptoms getting worse or not improving after a few hours or after prescribed medicine
- Age under 6 months or underlying health issues
Go to the ER if your child has stridor at rest, is working hard to breathe, or shows blue lips or drooling. If you’re unsure but worried about your child’s breathing, it’s safest to go to the ER. Talk to your doctor before trying a new medication.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes—when they deliver epinephrine in a medical setting. It reduces airway swelling within minutes but usually wears off in about 2 hours, so children are observed. For most cases, a single dose of dexamethasone is the main treatment.
Usually no. Albuterol opens the lower lung airways (asthma); croup is swelling of the upper airway (voice box). It may be used only if a clinician suspects co‑existing wheeze.
Keep your child calm, try cool or humidified air, sit them upright, and offer small sips of fluids—while the prescribed steroid (often dexamethasone) begins to work.
Most cases improve within 3–5 days. The first 1–2 nights are usually the worst.
Go now for stridor at rest, visible chest/neck retractions or fast breathing, blue or gray lips, drooling or trouble swallowing, extreme sleepiness or agitation, or if symptoms are worsening.
Yes. Recurrences are common in toddlers and usually lessen as the airway grows. Frequent or severe episodes should be discussed with your pediatrician.
No. Croup is usually viral, so antibiotics do not help.