On this page

Nebulizers can help bronchitis symptoms when your airways are tight or inflamed, but they are not needed for every case. A nebulizer turns liquid medicine into a fine mist you breathe in, which can open swollen airways and make coughing less intense. Most mild acute bronchitis clears with rest and fluids. In chronic bronchitis (a form of COPD), inhaled treatments are commonly part of daily care.
If you’re wondering 'should I use my nebulizer if I have bronchitis,' the short answer is: use it when you’re wheezing or short of breath—only as directed by your doctor.
What Bronchitis Does to Your Lungs
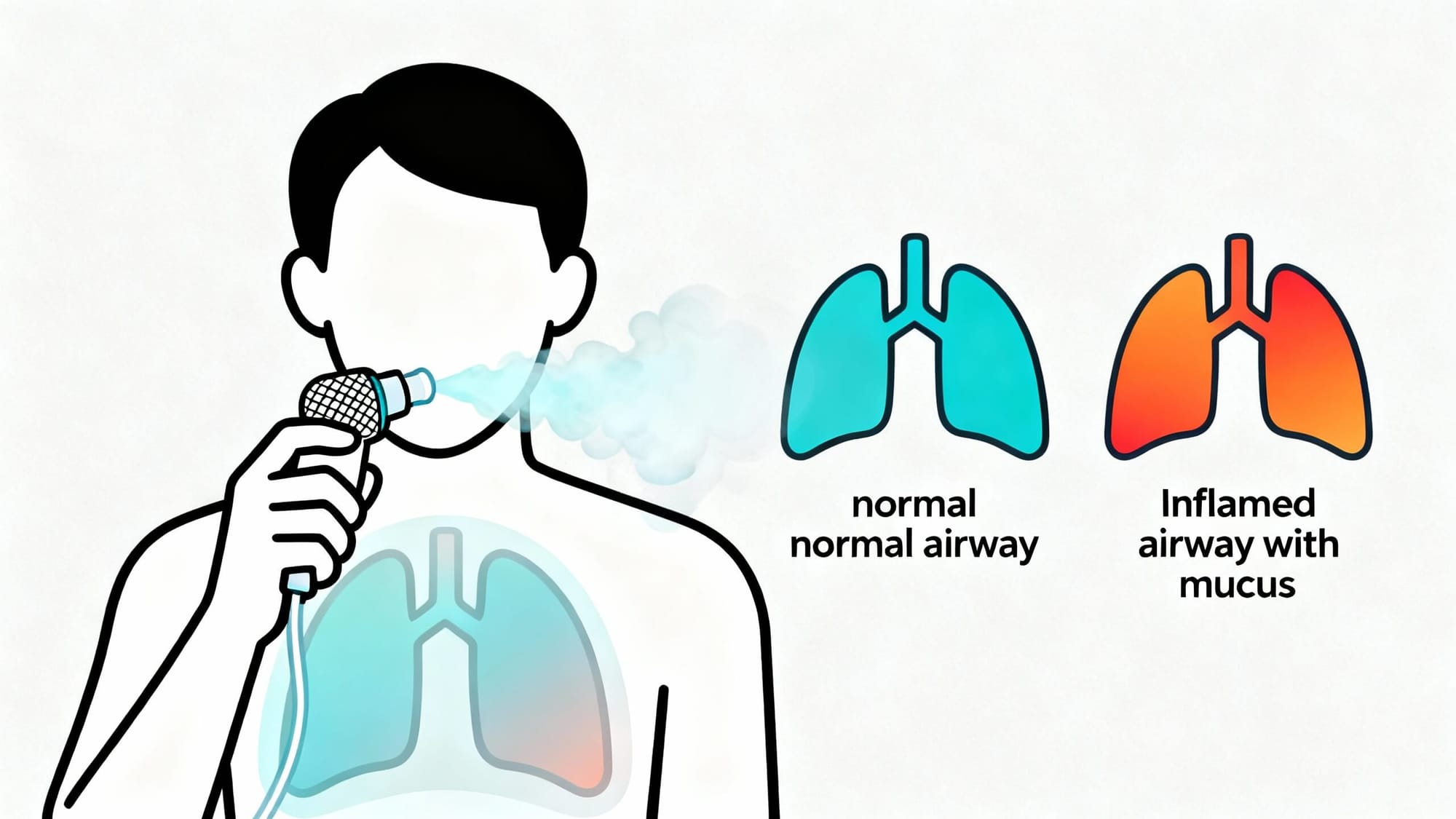
Bronchitis is swelling of the bronchial tubes, the airways that carry air into your lungs. When these tubes get irritated, they make extra mucus. That leads to cough, chest congestion, and sometimes wheezing and shortness of breath.
- Acute bronchitis: usually caused by a virus and lasts a couple of weeks. It usually follows a cold. Most people get better with time and home care.
- Chronic bronchitis: a type of COPD. It causes a long-term, mucus-heavy cough and breathing trouble. Inhaled meds (inhalers or nebulizers) are commonly used to improve airflow.
Why breathing feels hard: swollen airways get narrow, and thick mucus clogs the tubes. Opening those airways can make a big difference.
Narrowed, mucus-filled airways are the main reason bronchitis makes you cough and wheeze.
How a Nebulizer Helps During Bronchitis
A nebulizer turns liquid medicine into a mist you breathe through a mouthpiece or mask. The mist goes straight into your lungs.
- Bronchodilators (like albuterol) relax the muscles around your airways so they open up. This can ease wheezing, chest tightness, and a persistent cough. Albuterol can help bronchitis symptoms if your airways are tight or you’re wheezing.
- Inhaled corticosteroids (like budesonide) can calm airway swelling in chronic or severe flare-ups.
- Saline (sterile salt water) can thin mucus so it’s easier to cough up.
Acute bronchitis: doctors sometimes prescribe a nebulizer if you are wheezing or very short of breath. Evidence shows bronchodilators have little benefit for routine acute bronchitis without wheeze.
Chronic bronchitis/COPD: inhaled treatments are common. A nebulizer can help you get medicine into your lungs, especially if an inhaler is hard to use.
Nebulizers deliver medicine straight to swollen airways, which can quickly ease wheeze and tight breathing.
When to Use a Nebulizer for Bronchitis
Use a nebulizer for bronchitis only when it fits your symptoms and plan from your doctor.
Use it if:
- You have wheezing or can’t catch your breath. A bronchodilator treatment can open airways.
- You have asthma or COPD and got bronchitis. Your action plan may include nebulized meds during flares.
- A doctor recommends it for a severe episode. Short-term use can help you breathe easier.
Probably not needed if:
- Your cough is mild and breathing is fine.
- You aren’t wheezing and symptoms are improving with rest and fluids.
How long to use a nebulizer for bronchitis: Treatments are typically short-term for acute episodes. Most home treatments run until the cup is empty—your doctor will set your schedule.
Save nebulizer treatments for wheeze or hard breathing, not for a simple chest cold.
Nebulizer vs. Inhaler vs. Steam: What’s Best?
Here’s how these options compare in real use.
| Option | What it does | Pros | Cons | Best for |
|---|---|---|---|---|
| Nebulizer (medicated or saline) | Delivers medicine or saline mist to the lungs | Easy to breathe normally; helpful for wheeze; useful if inhaler technique is difficult | 5–10 minutes per treatment; needs device and power | Severe acute symptoms with wheeze; COPD/chronic bronchitis flare-ups |
| Inhaler (with spacer) | Quick puffs of bronchodilator or steroid | Fast; portable; as effective as a nebulizer when used correctly[1] | Requires proper technique and timing | Mild to moderate cases; maintenance therapy |
| Steam/humidifier | Adds moisture to airways | May soothe and loosen mucus | Does not treat inflammation; limited evidence[2]; hot steam can burn[3] | Comfort care alongside medical treatment |
[1] Inhalers with spacers can be as effective as nebulizers when used properly. [2] Evidence for steam benefits in bronchitis is limited. [3] Hot steam can cause burns—use caution. Never nebulize oils; consumer “steam inhalers” are not for medications.
An inhaler with a spacer can work as well as a nebulizer when used correctly. You might see devices labeled “steam inhaler”—these are not for breathing medications.
How to Use a Nebulizer the Right Way
- Wash your hands and prep the dose. Open the medicine vial (or saline) and pour it into the nebulizer cup.
- Set up the device. Attach the tubing and mouthpiece or mask. Make sure the compressor is charged or plugged in.
- Breathe the mist. Sit upright. Place the mouthpiece in your mouth (or mask over nose and mouth). Turn it on and breathe normally until the cup is empty. Take a slow deep breath now and then to help medicine settle.
- Rinse if you used a steroid. Swish and spit water to lower the chance of mouth irritation or thrush.
- Clean the parts. Wash cup and mouthpiece/mask with warm soapy water, rinse, and air-dry after each use. Disinfect regularly as your manual says.
Note: A portable mesh nebulizer like TruNeb™ can make treatments easier to do away from home.
Right setup, slow breathing, and clean parts make each treatment safer and more effective.
Side Effects and Safety Notes
- Common side effects: Bronchodilators like albuterol can cause shakiness, a fast heartbeat, or nervous feelings that fade after a short time. Inhaled steroids can cause hoarseness or mouth thrush if you don’t rinse.
- Keep it clean: Not cleaning parts can grow germs and raise infection risk.
- Use only approved solutions: Do not nebulize oils or non-nebulizer liquids. Steam inhalers are not for medications.
Know the common side effects and keep equipment clean—using the right solutions and good hygiene keeps treatments safer.
⚠️ Stop and contact your doctor if you feel worse after a treatment (racing heart, chest pain, severe shakiness), or if your breathing doesn’t improve.
Talk to your doctor before trying a new medication or changing your treatment.
When to See a Doctor
⚠️ If you have severe shortness of breath, bluish lips/face, confusion, or trouble speaking in full sentences, call emergency services.
- High fever or fever that lasts more than a few days.
- Breathing gets worse or wheeze does not ease after treatment.
- Chest pain or coughing up blood.
- Cough lasts over 2–3 weeks or symptoms keep getting worse.
If you’re short of breath or not improving, it’s time to call your doctor.
Summary
Nebulizers can help with bronchitis when you have wheezing or trouble breathing by delivering medicine straight to your lungs. Many mild cases don’t need nebulizer therapy and improve with rest, fluids, and time. In chronic bronchitis, inhaled treatments are commonly part of daily care.
Use a nebulizer for bronchitis symptoms that affect your breathing, under your doctor’s guidance.
Frequently Asked Questions
Tap or click a question below to see the answer:
Not always. Inhalers with a spacer can work as well and are faster. Nebulizers help if you’re very short of breath or can’t use an inhaler well.
Yes, if your cough is tied to airway tightness or lots of mucus. The mist and medicine can open airways and make coughing fits ease.
Follow your doctor’s plan. For acute bronchitis, treatments are typically short-term; your doctor will set the schedule that’s right for you.
Yes. Saline can loosen mucus and soothe airways, though it doesn’t reduce inflammation like prescribed medicines do.







