On this page

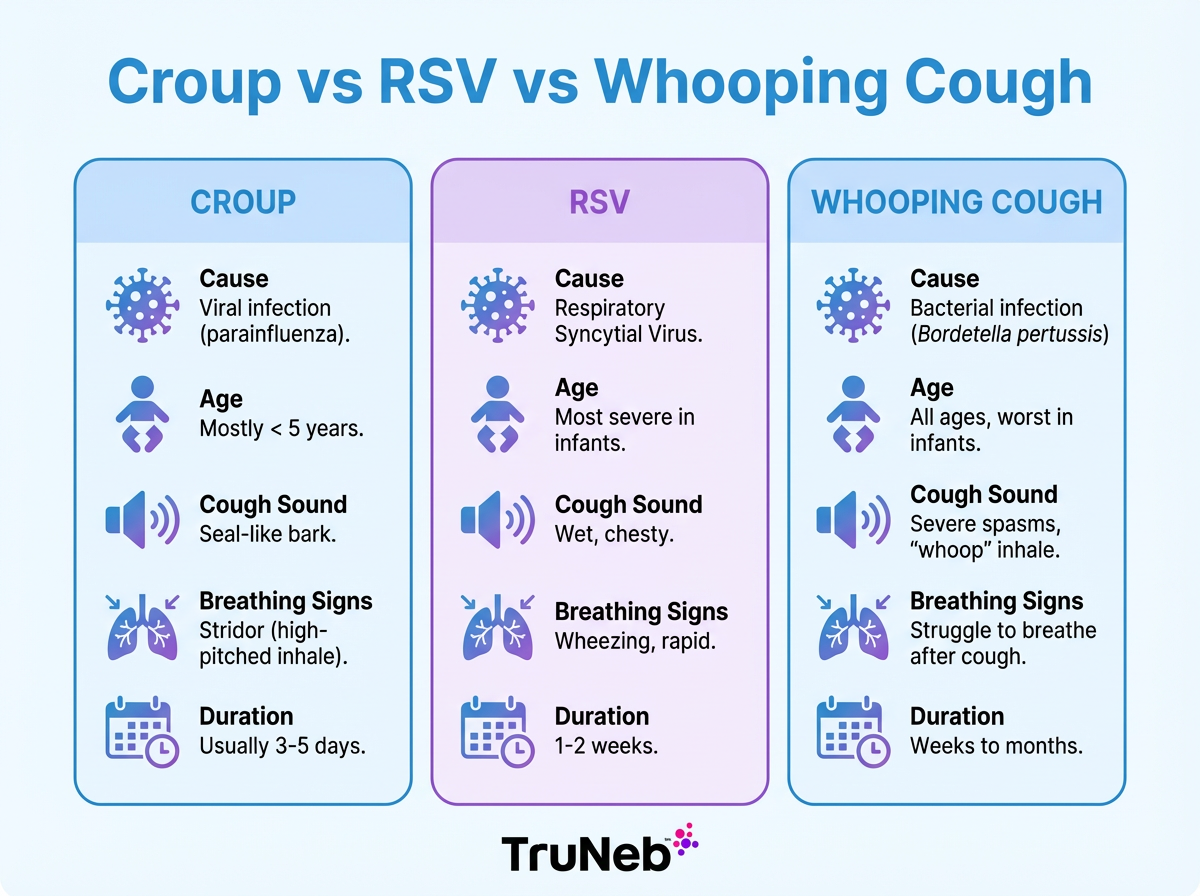
Quick Comparison: Croup vs. RSV vs. Whooping Cough
Here is a fast way to tell them apart. Start with the cough sound, then watch your child’s work of breathing.
In short: croup causes a barky cough from swelling high in the airway, RSV causes a wet cough and wheeze from the lungs, and whooping cough causes long coughing fits with a sharp whoop on the next breath.
Key point: Listen for the signature sound: bark, wheeze, or whoop.
Quick comparison chart: Key differences between croup, RSV, and whooping cough
| Feature | Croup | RSV | Whooping Cough |
|---|---|---|---|
| Cause | Viral (commonly parainfluenza) | Viral (respiratory syncytial virus) | Bacterial (Bordetella pertussis) |
| Typical Age | 6 months–3 years most common | Under 2 common; all ages can get it | All ages; most severe in young infants |
| Signature Cough | Barking, hoarse | Wet, congested cough with wheeze | Repeated coughing fits with a whoop |
| Breathing Signs | Stridor on inhale, noisy throat | Fast breathing, retractions, crackles | Gasping after fits; can vomit |
| Fever Pattern | Low-grade or none | Low to moderate early | Usually low or none after early phase |
| Contagiousness | Spreads like a cold while sick | Very contagious during season | Highly contagious for weeks if untreated |
| Primary Treatment | Calm child; single-dose steroid if needed | Supportive care; oxygen in severe cases | Antibiotics plus supportive care |
| Testing | Clinical diagnosis | Nasal swab can confirm RSV | PCR swab can confirm pertussis |
| Prevention | Hand hygiene; no croup vaccine | Hygiene; maternal RSV vaccination during pregnancy and long‑acting monoclonal antibodies for some infants; ask your child’s doctor | Vaccination with DTaP/Tdap |
| Duration / Course | Peaks over 1–2 nights; clears in ~3–5 days | Builds over several days; improves in 1–2 weeks | Cough lasts 6–10 weeks (the “100‑day cough”) |
Croup: Causes, Symptoms, and How It Differs
Croup is a viral illness, commonly caused by parainfluenza viruses, that inflames the upper airway, mainly the voice box and windpipe. The swollen airway narrows, so moving air makes a barky, seal-like cough. You might hear a harsh, high-pitched sound on inhale called stridor. Symptoms usually begin like a simple cold, then get louder at night in toddlers.
Most cases are mild. Kids can have a hoarse voice, a runny nose, and a low fever. Keeping your child calm helps the noise ease. Doctors sometimes give a single dose of an oral steroid, such as dexamethasone, to shrink swelling. In severe cases, hospital teams sometimes use a nebulized epinephrine treatment and observe.
Croup spreads like other colds and is usually most contagious in the first few days of illness.
How it differs: croup noise lives in the throat. RSV usually causes chest wheeze and a wet cough. Whooping cough causes long coughing fits with a whoop, not a bark.
In short: croup is an upper-airway problem that peaks over a night or two and fades in a few days.
RSV: Causes, Symptoms, and How to Recognize It
RSV is a common virus that targets the lower airways. It’s a leading cause of bronchiolitis and pneumonia in infants, and nearly all children encounter RSV by age two. It spreads easily in fall and winter. Preterm infants and children with heart or chronic lung disease are at higher risk for severe illness.
RSV usually starts like a cold. Then the cough turns wet and congested. Wheezing, fast or hard breathing, and feeding trouble in babies are common. You might see skin pull in between the ribs, called retractions. Fever can be mild or absent. Most cases improve with fluids, gentle nasal saline and suction, fever control, and rest. Severe cases sometimes need oxygen or IV fluids in the hospital.
Most RSV infections improve over 1–2 weeks, though the cough can linger a bit longer. Newer options, like maternal RSV vaccination during pregnancy and long‑acting monoclonal antibodies for some infants, can lower the risk of severe RSV. Ask your child’s doctor what’s recommended where you live.
How it differs: RSV sounds like the lungs are tight, with wheeze and crackles. Croup sounds like a bark in the throat. Whooping cough brings bursts of cough with a whoop and can lead to vomiting after spells.
In short: RSV is a lower-airway virus with a wet cough and wheeze, especially in babies.
Whooping Cough (Pertussis): Causes, Symptoms, and Course
Whooping cough is a highly contagious bacterial infection caused by Bordetella pertussis. After a week or two of cold-like symptoms, the cough turns into exhausting paroxysms—many coughs in a row—followed by a sharp, high-pitched whoop as your child tries to breathe in again. Older kids can vomit after a fit. Babies don’t always whoop; they can pause breathing (apnea) or turn dusky during spells.
Pertussis unfolds in three phases. In the catarrhal phase, it looks like a simple cold. The paroxysmal phase brings severe coughing fits for two to six weeks or more. The convalescent phase is a slow recovery where the cough gradually fades. This long timeline earns the nickname 100-day cough.
Antibiotics are used to clear the bacteria and shorten how long a person is contagious. They don’t stop the cough right away because the airways need time to heal. Supportive care includes humidified air, small frequent feeds, and close monitoring. Whooping cough is most dangerous for young infants, especially those too young to be fully vaccinated. Infants sometimes need hospital care for breathing and hydration. Vaccination with DTaP for children and Tdap boosters for older kids, adults, and during pregnancy is key prevention.
Key point: pertussis is a long-haul cough in fits. Antibiotics help stop the spread, but the cough can linger as airways heal.
When To Seek Medical Care: Red Flags for Breathing Troubles
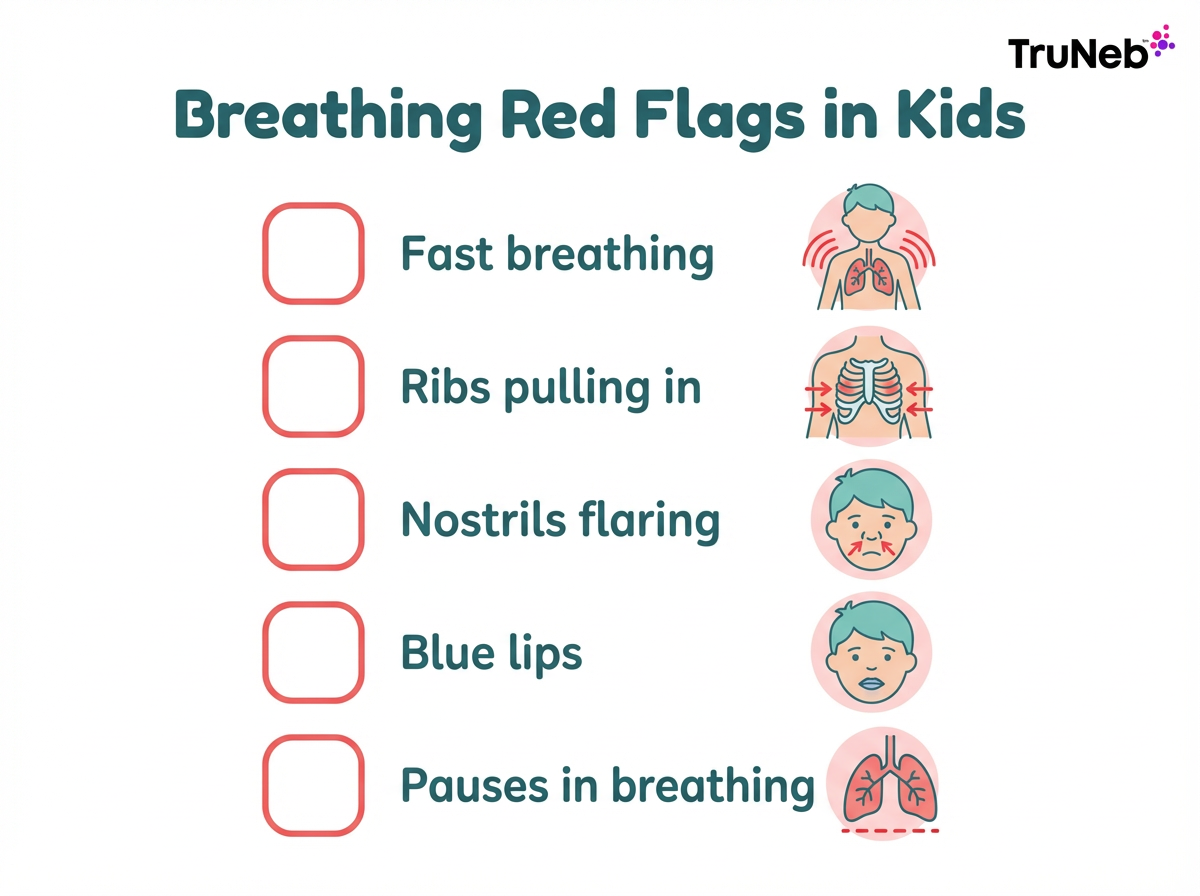
No matter which illness it is, some signs mean your child needs medical help.
- Working hard to breathe (fast breaths, ribs pulling in, nostrils flaring)
- Stridor or wheeze at rest, or can’t catch breath between coughs
- Blue or gray lips or face (cyanosis)
- Any pause in breathing, limpness, or very weak cry in an infant
- Signs of dehydration (very dry mouth, few or no wet diapers, not drinking)
- Unable to keep fluids down or feed because of cough
- High fever with a very ill appearance, or getting worse instead of better
⚠️ Call 911 for severe breathing trouble, blue coloring, or pauses in breathing. For milder but worrisome signs, contact your pediatrician or go to urgent care. When in doubt, have your child’s doctor check your child’s breathing. Breathing trouble in babies, especially under 3 months, should always be checked quickly by a doctor.
One-line takeaway: If you’re worried about your child’s breathing or see any of these red-flag signs, it’s safest to have a doctor check them right away.
Home Care Tips for Croup, RSV, and Mild Cases
Keep your child calm and close. Crying can make a croupy cough louder. Comfort helps breathing stay steady.
Keep fluids going. Offer breast milk or formula for infants and water or oral rehydration for older kids. Hydration helps thin mucus and prevents dehydration.
Moist air can soothe the airway. A cool-mist humidifier in the room or brief time in steamy air can help. Cool night air can also ease croup symptoms for some children.
Clear the nose with saline drops and gentle suction before feeds and sleep. Babies breathe through the nose, so this step matters.
Your child’s doctor might recommend acetaminophen, or ibuprofen for children 6 months and older, to ease fever or discomfort. Always check dosing with your child’s doctor or follow the package instructions.
Over-the-counter cough and cold medicines aren’t recommended for young children; ask your doctor before giving anything besides fever reducers.
If your child’s doctor prescribes it, use a nebulizer for medicines or saline. A quiet, portable mesh nebulizer, such as the TruNeb™ portable mesh nebulizer, can make treatments easier for kids who don’t tolerate loud machines. Some providers also recommend 3% or 7% hypertonic saline to help thin mucus in certain lower‑airway conditions, usually under close monitoring. This isn’t needed for every child with croup or RSV and should only be used if your child’s doctor specifically prescribes it.
You might see boxes labeled “steam inhaler” next to nebulizers. These aren’t the same as nebulizers and shouldn’t be used to give prescription breathing medications.
Safety note: Talk to your doctor before trying a new medication. Never start, stop, or change prescribed treatments without medical guidance.
In short: gentle home care focuses on comfort, fluids, moist air, and doctor‑recommended treatments like nebulizers.
Frequently Asked Questions
This FAQ answers common questions about how croup, RSV, and whooping cough differ, when they can overlap, and when to worry. Tap or click a question below to see the answer:
No. Croup is usually a viral swelling of the upper airway with a barky cough. RSV is a virus that inflames the lungs and bronchioles, causing a wet cough and wheeze. Whooping cough, also called pertussis, is a bacterial infection that causes severe coughing fits with a whoop. They need different care; antibiotics treat pertussis but not croup or RSV.
Yes. RSV can sometimes trigger croup-like symptoms in young children. A child can have a barky cough from upper-airway swelling along with RSV signs like wheeze and heavy congestion. Treatment stays supportive, and your child’s doctor might add a steroid for the croup component.
It depends on age and severity. Whooping cough is most dangerous for young infants and can be life-threatening. RSV can be serious in babies and in children with heart or lung conditions. Croup can sound scary but is usually mild; severe cases with stridor at rest need urgent care.
Doctors use the history and exam — cough sound, age, timing, and breathing signs. Tests can confirm RSV with a nasal swab and can confirm pertussis with PCR from a nose or throat sample. There isn’t a specific lab test for croup; the diagnosis is clinical, and imaging is rarely needed.
Vaccines protect against pertussis with DTaP and Tdap. RSV prevention options are available for some groups, including pregnant people, some older adults, and certain high-risk infants; ask your child’s doctor what’s recommended where you live. There isn’t a vaccine for croup itself.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about any questions or concerns regarding your child’s health.