On this page
How COPD and Heart Failure Are Different (Lungs vs. Heart)
COPD and heart failure aren’t the same.
- COPD (chronic obstructive pulmonary disease) is a lung disease. Damaged airways make it hard to move air out, causing chronic cough, mucus, wheezing, and shortness of breath. COPD includes chronic bronchitis and emphysema.
- Heart failure (also called congestive heart failure or CHF) is a heart problem. The heart can’t pump enough blood, which leads to fluid buildup, swelling (edema), and breathlessness, especially when lying flat.
COPD is a lung disease, not a type of heart disease, even though it can increase your heart risk over time. That’s why the same shortness of breath can feel confusing when you’re living with one or both conditions.
Left-sided vs right-sided heart failure:
- Left-sided heart failure can back fluid into the lungs, which triggers coughing and shortness of breath.
- Right-sided heart failure causes swelling in the legs and ankles. Advanced COPD can strain the right heart over time.
Causes differ:
- COPD is most commonly linked to smoking and long-term lung irritants.
- Heart failure is usually tied to heart disease, high blood pressure, or a past heart attack.
Bottom line: COPD starts in the lungs; heart failure starts in the heart. Both can make breathing hard for different reasons.
Why COPD and Heart Failure Often Occur Together
They share a lot of the same risks.
- Smoking harms lungs and blood vessels.
- Age and inactivity add strain over time.
- Inflammation from COPD can affect the whole body, including the heart.
COPD can strain the right side of the heart.
- Long-term low oxygen and high pressure in lung arteries (pulmonary hypertension) make the right ventricle work harder.
- Over time, that stress can lead to right-sided heart failure called cor pulmonale.
It also goes the other way.
- Left-sided heart failure pushes fluid into the lungs. That can make COPD symptoms feel worse.
These clues are helpful but not a diagnosis—only your doctor and tests can sort out the exact cause.
Bottom line: COPD and heart failure often occur together because they share risks like smoking and age, and severe COPD can strain the right side of the heart.
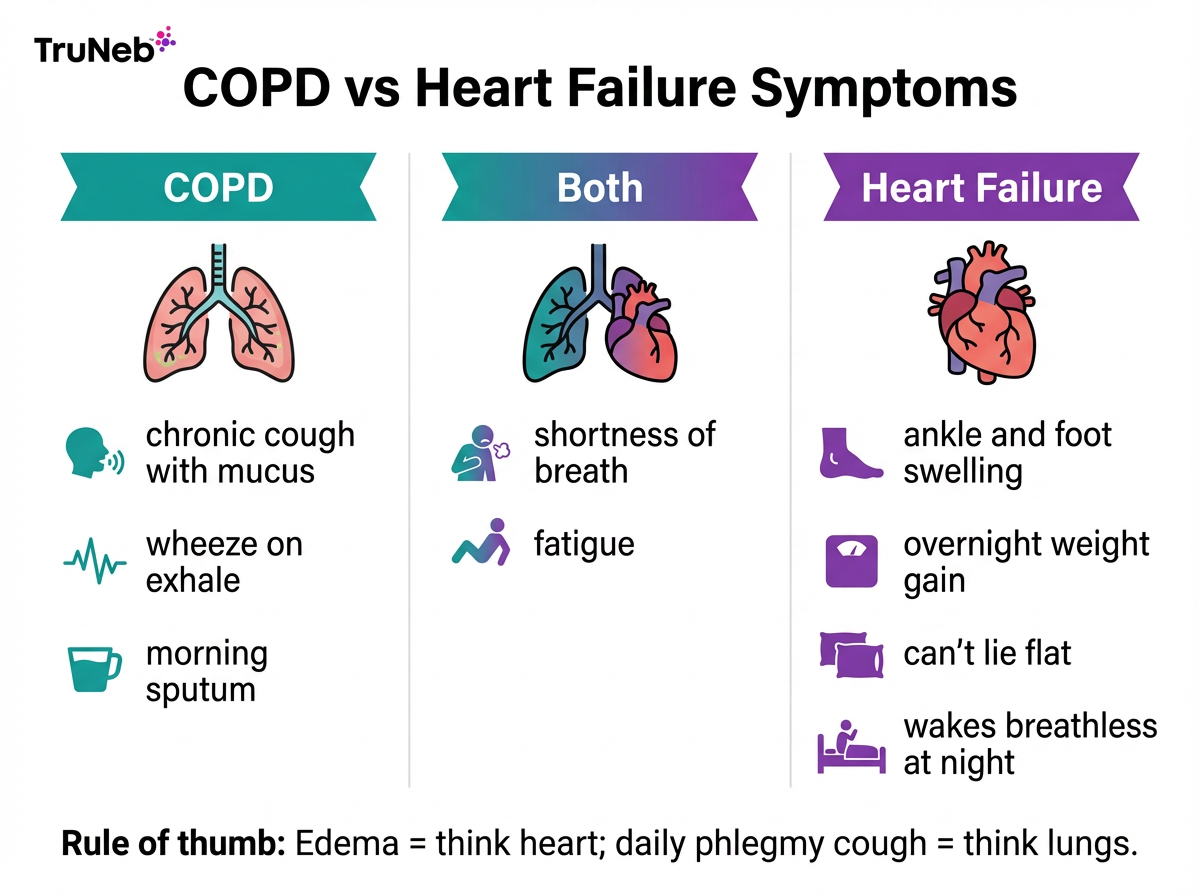
COPD or Heart Failure? Symptom Clues to Tell the Difference
Symptoms that point to COPD:
- Chronic cough (usually with thick mucus)
- Wheezing, especially on exhale
- Long history of smoking or lung irritants
Symptoms that point to heart failure:
- Swelling in feet or ankles (edema)
- Sudden weight gain from fluid
- Trouble breathing when lying flat (orthopnea) or waking up breathless at night (paroxysmal nocturnal dyspnea)
- Needing extra pillows to sleep
Shared symptoms (either condition):
- Shortness of breath with activity
- Fatigue and exercise intolerance
- Occasional chest tightness or wheeze
The biggest difference between COPD and heart failure symptoms is a chronic cough with mucus versus fluid swelling in the legs and sudden night-time breathlessness.
Bottom line: a daily, phlegmy cough suggests COPD; new leg swelling and night-time breathlessness suggest heart failure.
⚠️ If you suddenly can’t catch your breath, have new chest pain, or feel like you’re going to pass out, call 911 or seek emergency care right away.
Tests That Tell Lung Problems from Heart Problems
Doctors usually check both systems.
- Physical exam: leg swelling and neck vein bulging point to heart failure; wheeze suggests airway narrowing.
- Chest X-ray: enlarged heart or lung fluid suggests heart failure; over-inflated lungs suggest COPD.
- BNP blood test: high B-type natriuretic peptide can point to heart failure.
- Echocardiogram: ultrasound that shows how well the heart pumps.
- Spirometry (PFTs): confirms airflow blockage typical of COPD.
- ECG: looks for past heart damage or rhythm issues.
Bottom line: high BNP and an abnormal echocardiogram can point to heart failure; obstructed spirometry points to COPD.
Treating COPD and Heart Failure Together
Treat both the lungs and the heart.
For COPD:
- Doctors use bronchodilators (inhalers) to open airways.
- Your doctor may add an inhaled corticosteroid if you have frequent flare-ups.
- Pulmonary rehab helps build stamina and teaches breathing techniques.
- Oxygen therapy can help when your oxygen is low.
- Nebulizer treatments are an option when inhalers are hard to use.
For heart failure:
- Doctors use medicines that support the heart and reduce fluid (for example, ACE inhibitors/ARBs, cardio-selective beta-blockers, diuretics).
- Your plan typically includes low-sodium eating and daily weight checks to limit fluid buildup.
Safety notes:
- Cardio-selective beta-blockers are generally considered safe in COPD when a cardiologist prescribes them for heart disease.
- Some bronchodilators can raise heart rate, so your doctors balance doses and choices.
Team approach: if it’s unclear which condition is flaring, doctors sometimes treat both at once and adjust as tests come back.
Using Nebulizer Therapy Safely with Heart Failure
A nebulizer turns liquid medicine into a fine mist you breathe in. A portable mesh nebulizer like the TruNeb™ portable nebulizer can help deliver prescribed bronchodilators or saline, especially if you’re short of breath or have trouble with inhalers.
Hypertonic saline is a salty nebulized solution some doctors use to help thin mucus for certain lung conditions. It should only be used under medical guidance, particularly if you have heart failure or fluid limits. It’s available in strengths like 3% or 7%, but your doctor will decide what’s right for you.
Bottom line: treating COPD and heart failure together means supporting both your lungs and your heart with the right mix of medicines, lifestyle changes, and close follow-up.
Talk to your doctor before starting or changing any treatment. See the full disclaimer at the end.
Living with Both COPD and Heart Failure: Day-to-Day Tips
Managing COPD with heart failure takes a combined daily plan for your lungs and your heart.
Stick to your plan:
- Take your heart and lung medicines on the schedule your doctor recommends.
- Use your inhaler or nebulizer as prescribed.
- Do your home exercises from pulmonary or cardiac rehab.
Track changes:
- If your heart doctor has asked you to track your weight, weigh yourself every morning and call them if you see sudden fluid weight gain.
- Watch for more swelling, more night-time breathlessness, or a big change in cough or mucus color. If you notice any of these changes, contact your doctor promptly.
Move safely:
- Walk most days if you can, and pause when winded, as your doctor or rehab team recommends.
- Practice pursed‑lip and diaphragmatic breathing during activity.
Eat and hydrate smart:
- Lower sodium to reduce fluid buildup (follow your heart failure plan).
- Stay hydrated enough to keep mucus thin unless your doctor limits fluids.
Protect your lungs:
- Don’t smoke, and avoid secondhand smoke.
- Keep up with vaccines your doctor recommends (like flu and pneumonia).
Bottom line: low-salt eating, steady movement, and daily symptom checks help you stay ahead of both conditions.
Your Care Team: Pulmonologist + Cardiologist
When COPD and heart failure overlap, teamwork matters.
- A pulmonologist tunes your COPD plan (inhalers, rehab, oxygen).
- A cardiologist adjusts heart medicines and fluid goals.
- Your primary care doctor helps connect the dots.
You’re the most important member of your care team.
Your role:
- Bring a full medication list to every visit
- Share new symptoms right away
- Ask your doctors to message each other
Good coordination can reduce hospital visits when you have both COPD and heart failure.
Bottom line: a coordinated team of doctors can reduce setbacks and help you feel better day to day.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. COPD and congestive heart failure can look similar at first—both can cause breathlessness and fatigue. Tests like a chest X‑ray, BNP blood test, echocardiogram, and spirometry help tell them apart. Many people have both, which is why doctors check for each.
Yes, severe COPD can lead to a type of right-sided heart failure called cor pulmonale, but it doesn’t cause every kind of heart failure.
No. Heart failure doesn’t damage airways the way COPD does. But fluid in the lungs from heart failure can make breathing feel like a lung problem.
No. COPD is a lung disease. But COPD can raise heart risks over time because of shared factors like smoking and inflammation.
Having both conditions is serious and can mean more symptoms and a higher risk of flare-ups. The good news: coordinated treatment and rehab can improve daily breathing and reduce hospital visits.
Key Takeaways: COPD and Heart Failure
- COPD and heart failure are different problems that often overlap.
- New swelling, fast fluid weight gain, or needing extra pillows point to heart failure.
- A daily cough with thick mucus points to COPD.
- Tests (BNP, echocardiogram, spirometry, chest X‑ray) sort out what’s driving symptoms.
- Treating both systems together usually works best, and make sure your doctors coordinate.
- Safety note: Talk to your doctor before trying a new medication or hypertonic saline; see the full disclaimer below.
A portable mesh nebulizer like TruNeb can support your lung routine as part of a doctor-approved plan.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, test results, and any treatments, including nebulizer therapies or hypertonic saline.