On this page
COPD Breathing Devices Explained
COPD (chronic obstructive pulmonary disease) makes breathing hard. The right device can open airways, clear mucus, or keep oxygen levels safe.
Here is what most people use:
- Inhalers: Small handheld devices that send medicine straight to your lungs.
- Nebulizers: Machines that turn liquid medicine into a mist you breathe in normally.
- Oxygen therapy: Tanks or portable concentrators for low oxygen levels.
- Airway clearance tools: Positive expiratory pressure (PEP) devices and huff cough to move sticky mucus.
- Noninvasive ventilation: BiPAP devices to support breathing, usually at night.
Consumer warning: Steam inhalers are not nebulizers and should not be used for prescription COPD medicines.
Each tool has a job. Some help in a flare-up. Some help every day. Your doctor can help decide which mix of these tools fits your COPD plan.
Safety note: Talk to your doctor before trying a new medication or device.
Takeaway: COPD devices do three jobs—open airways, move mucus, and support oxygen.
Inhaler vs Nebulizer for COPD
Both deliver medicine to your lungs. When used the right way, they can work equally well. The big difference is how you take them.
- Inhaler: A small handheld device that delivers a quick puff of medicine. It’s very fast and pocket sized, but you must time your breath and press at the right moment (a spacer can help).
- Nebulizer: A machine that turns liquid medicine into a mist you breathe normally for several minutes. No timing needed. Helpful during flare-ups or when your chest feels tight.
Mesh nebulizers are quiet, fast, and easy to carry. A portable mesh nebulizer lets you take a treatment without tubing or a loud motor.
Doctors may favor a nebulizer during severe flare-ups, very low lung function, or when arthritis, tremor, vision, or memory make inhaler technique hard. If your technique is solid and you need speed, an inhaler can be the simplest choice.
Common medicines used by both include bronchodilators, inhaled steroids, and, when a doctor recommends it, saline to thin mucus.
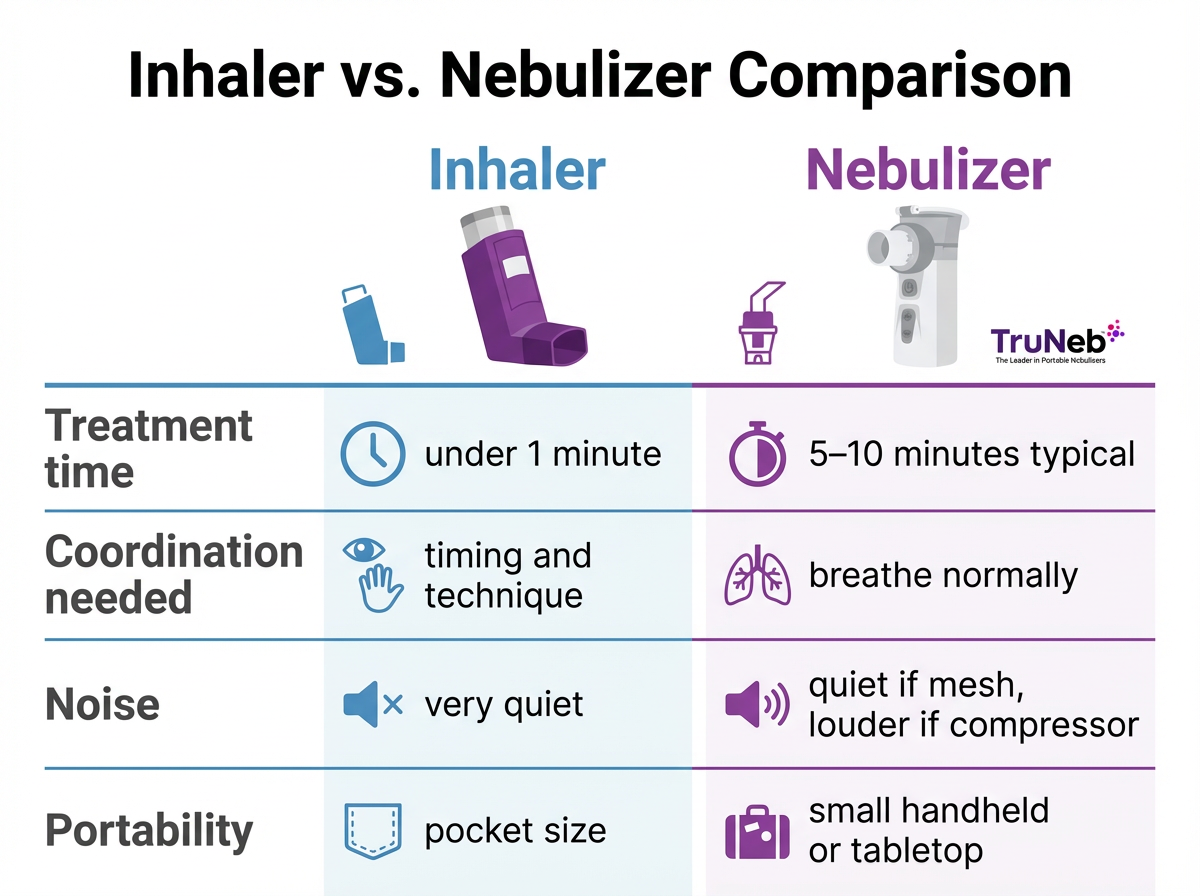
Inhaler vs nebulizer: quick comparison
| Feature | Inhaler | Nebulizer |
|---|---|---|
| Treatment time | Under 1 minute | 5–10 minutes typical |
| Breathing coordination | Needs timing and technique (spacer helps) | Breathe normally; no timing |
| Noise | Very quiet | Quiet if mesh; louder if compressor |
| Portability | Pocket size | Small handheld or tabletop |
| Typical use-case | Fast relief when technique is reliable | Flares, tight chest, or low lung function |
| Medication compatibility | Common bronchodilators and some steroids | Bronchodilators, steroids, doctor-directed saline |
| Cleaning | Minimal | Cup and mouthpiece need regular cleaning |
Key takeaway: Inhalers trade speed for required technique, while nebulizers trade time for easier breathing.
Safety note: Talk to your doctor before trying a new medication or changing devices.
Takeaway: Nebulizers are easier during flare-ups; inhalers are faster but need technique.
Oxygen Therapy Options for COPD
If tests show your oxygen runs low, your doctor may prescribe oxygen therapy. The goal is to keep your oxygen in a safe range so your heart and brain get what they need.
Main options:
- Oxygen tanks: Compressed gas or liquid oxygen. Heavier, need refills. Good for higher continuous flow.
- Portable oxygen concentrator (POC): Pulls oxygen from the air. Lighter, runs on batteries, usually pulse flow. Great for getting out of the house.
Plan your power and refills. Keep spare batteries charged for portable concentrators, and work with your supplier for travel. Use oxygen only as prescribed.
Safety note: Do not change your flow rate on your own. Keep oxygen away from flames and heat sources, and don’t smoke or let anyone smoke near oxygen. Store tanks upright in a well‑ventilated area.
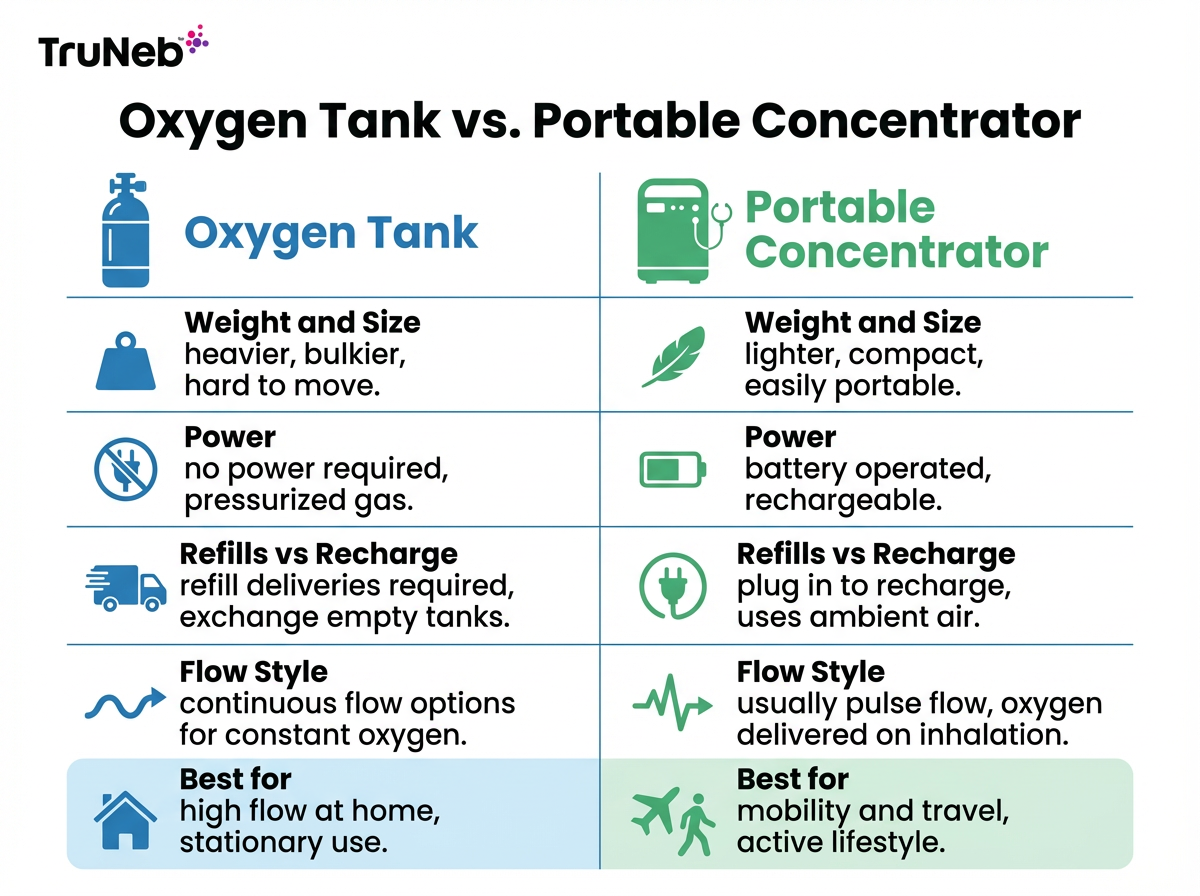
Oxygen tanks vs portable oxygen concentrators: quick comparison
| Feature | Oxygen tank | Portable oxygen concentrator |
|---|---|---|
| Weight & size | Heavier; larger | Lighter; compact |
| Power | No power needed | Battery powered; needs recharging |
| Refills vs recharge | Delivery/refill swaps | Plug in to recharge batteries |
| Flow style | Continuous flow options | Usually pulse flow |
| Best for | Higher continuous flow at home | Mobility, errands, and travel |
| Travel notes | Plan deliveries | Plan batteries and power access |
Key takeaway: Tanks excel for higher continuous flow at home, while portable concentrators favor mobility with battery planning.
Note: Some portable concentrators support low-rate continuous flow—check your model and prescription.
Takeaway: Oxygen tanks work best for higher continuous flow at home, while portable oxygen concentrators are better for mobility and fewer refills.
Airway Clearance Tools That Help Move Mucus
Thick mucus can trap air and make you cough all day. Two helpers:
- Positive expiratory pressure (PEP) devices: You exhale against gentle resistance. This back pressure keeps airways open and moves mucus. A small study of 23 people reported less breathlessness using a pocket PEP device.
- Huff cough: A quick series of strong exhales to bring mucus up without long strain.
Not everyone with COPD needs airway clearance tools—they’re usually used when thick mucus is a problem.
Your doctor may recommend nebulized hypertonic saline, such as 3% or 7%, to thin mucus.
Safety note: Talk to your doctor before adding PEP or saline. Ask for coaching on huff cough so it works without tiring you out.
Takeaway: When taught by your doctor, daily PEP plus huff cough can loosen and clear mucus.
Noninvasive Ventilation at Home
People with more advanced COPD sometimes use bilevel positive airway pressure (BiPAP) at night. BiPAP gives one pressure when you breathe in and a lower pressure when you breathe out. It can help when your lungs and breathing muscles need support, or if you have sleep apnea too.
Continuous positive airway pressure (CPAP) is mostly for sleep apnea. BiPAP is more common in COPD when extra support is needed.
Doctors may consider BiPAP for chronic high carbon dioxide (hypercapnia), repeated hospitalizations for breathing failure, or overlapping sleep apnea.
These devices are prescription only. You need a sleep or lung specialist to set the pressure and fit the mask.
Safety note: Do not change your settings on your own. Report skin sores or leaks to your doctor. If you have severe trouble breathing, chest pain, confusion, or bluish lips or face, seek emergency care right away.
Takeaway: BiPAP is a prescription support tool for select COPD cases, often at night.
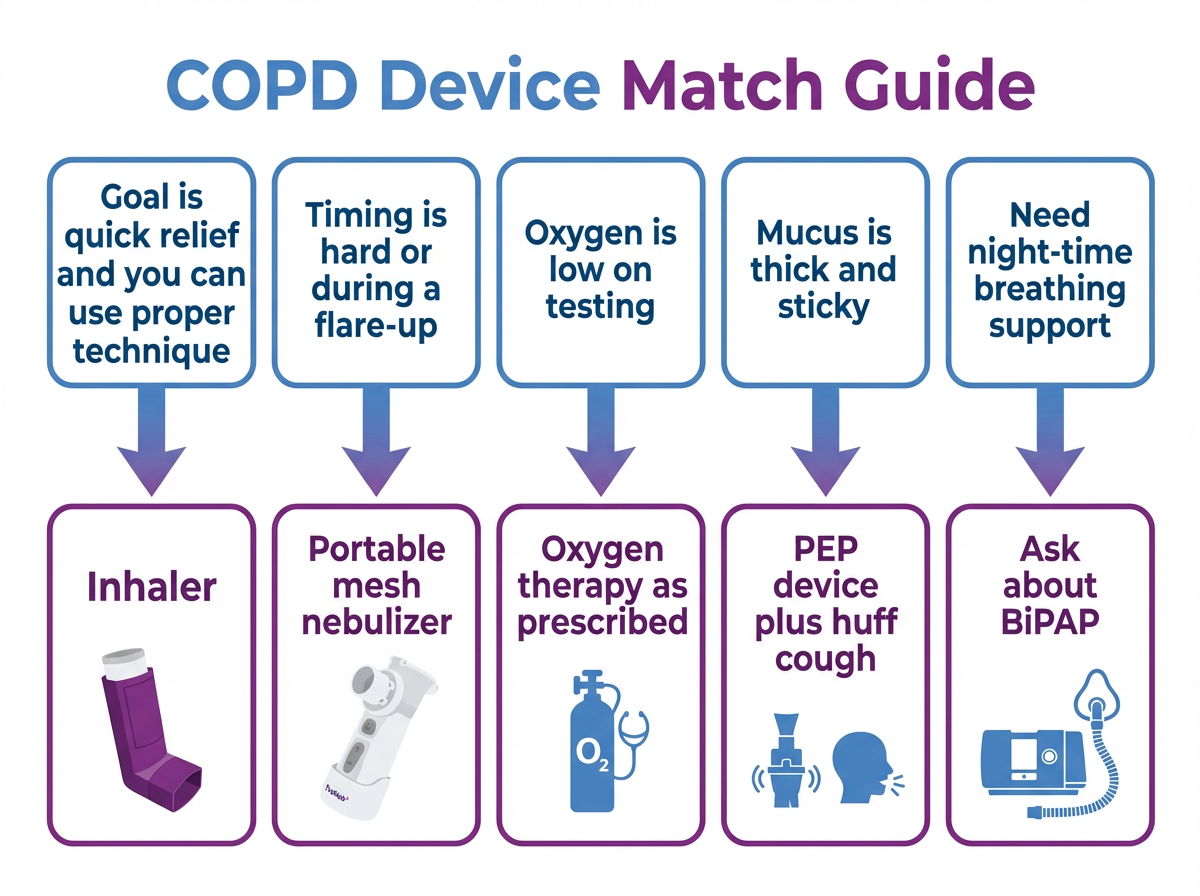
How to Choose Your COPD Device
COPD Device Readiness Checklist:
- Goal: Quick relief, daily control, mucus clearance, or oxygen support?
- Setting: Home only or out and about?
- Medication fit: Will your medicine work in the device you want?
- Ability to operate the device: Hand strength, vision, memory, and comfort with cleaning.
- Insurance and budget: What will insurance cover versus out-of-pocket costs?
- Noise: Do you need a quiet setup for night or travel?
- Power: Plug-in, rechargeable battery, or both?
- Cleaning: Fewer parts are easier to clean and keep safe.
- Support: Warranty, spare parts, and customer help.
Safety note: Your doctor should make the final call for prescription therapies.
Coming soon: Try our quick "Find Your COPD Device" quiz to see options to discuss with your doctor.
Takeaway: Pick the device that matches your goal, setting, and medication.
Frequently Asked Questions
Tap or click a question below to see the answer:
They can work equally well when used correctly. Inhalers are fast and pocket sized but require timing and technique (a spacer can help). Nebulizers deliver a steady mist you breathe normally and can be easier during a flare or when your chest feels tight. Ask your doctor which fits your plan.
You typically don’t need a prescription to buy a nebulizer device out of pocket. If you’re going through insurance, your plan will usually require a prescription and documentation of need. Nebulized medicines always require a prescription.
No. Steam inhalers heat water to make warm vapor and aren’t designed for prescription medicines. COPD medications must be used in devices approved for them, set up by your doctor or respiratory therapist.
Doctors typically consider BiPAP for people with chronic high carbon dioxide, repeated hospitalizations for breathing failure, or COPD that overlaps with sleep apnea. It’s usually used at night. BiPAP is prescription-only and requires a specialist to set pressures and fit the mask.
It can help thin mucus for some people when a doctor recommends it. It isn’t right for everyone and can cause more coughing or throat irritation. Use only the concentration and schedule your doctor prescribes.
Yes. Keep your nebulizer, charger, and a backup inhaler in your carry-on. For oxygen, check airline rules early, bring flight-approved batteries, and plan power for layovers. Your oxygen provider can help with paperwork and logistics.
The Philips InnoSpire Go is discontinued. One alternative is a compact mesh nebulizer such as the TruNeb portable mesh nebulizer. Choose a device that fits your medication, cleaning needs, and travel plans.
Yes. The FDA approved ensifentrine for maintenance treatment in adults with COPD. Ask your doctor if it fits your plan.
Follow your device manual first. As a general example, some brands suggest replacing the mesh or nozzle every 1–2 months with daily use. Replace sooner if you notice longer treatment times or weaker mist.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, devices, and medications.
Takeaway: Work with your doctor to choose a mix of COPD devices that fits your symptoms, lifestyle, and budget.