On this page
Nebulizer vs Oxygen Therapy: What’s the Difference
A nebulizer turns liquid medication (like albuterol) into a fine mist you breathe in. It helps open your airways so air can move more easily.
Oxygen therapy adds extra oxygen gas (from a concentrator or tank) to your breathing when your blood oxygen is low.
These are not the same and can’t replace each other. Think of oxygen as the air your body needs, and a nebulizer as the way you take lung medicine. Lots of people use both, but for different reasons.
You might see 'steam inhaler' on shelves—those are not nebulizers and don’t deliver prescription medications.
A nebulizer delivers medicine to your lungs; oxygen therapy adds oxygen to your breath—these aren’t interchangeable.
Nebulizers deliver prescription medication as a mist to the lungs; they do not supply oxygen.Oxygen therapy provides supplemental oxygen gas for low blood oxygen; it does not deliver medication.The two therapies are complementary, not interchangeable. Typical jet-nebulizer treatments last about 5–10 minutes.
| Device | What it delivers | Purpose | Common use |
|---|---|---|---|
| Nebulizer | Medication mist | Opens airways | Asthma/COPD flare, daily meds |
| Oxygen concentrator/tank | Oxygen gas | Raises blood oxygen | Low O₂ (hypoxemia), COPD oxygen support |
Can You Nebulize While on Oxygen? The Short Answer
Yes, you generally can use a nebulizer while on oxygen. Plenty of people keep their nasal cannula on during a breathing treatment, or they use their oxygen source to power the nebulizer.
There are two common ways to combine them:
- Keep your oxygen on through a nasal cannula while using a nebulizer mouthpiece or mask.
- Some patients use oxygen as the driving gas for the nebulizer when their doctor recommends it.
There are a few exceptions for certain COPD cases (more below). Your doctor can tell you what’s best for you.
You can use oxygen and a nebulizer at the same time if you follow the setup your doctor recommends.
How to Use a Nebulizer with Your Oxygen Supply
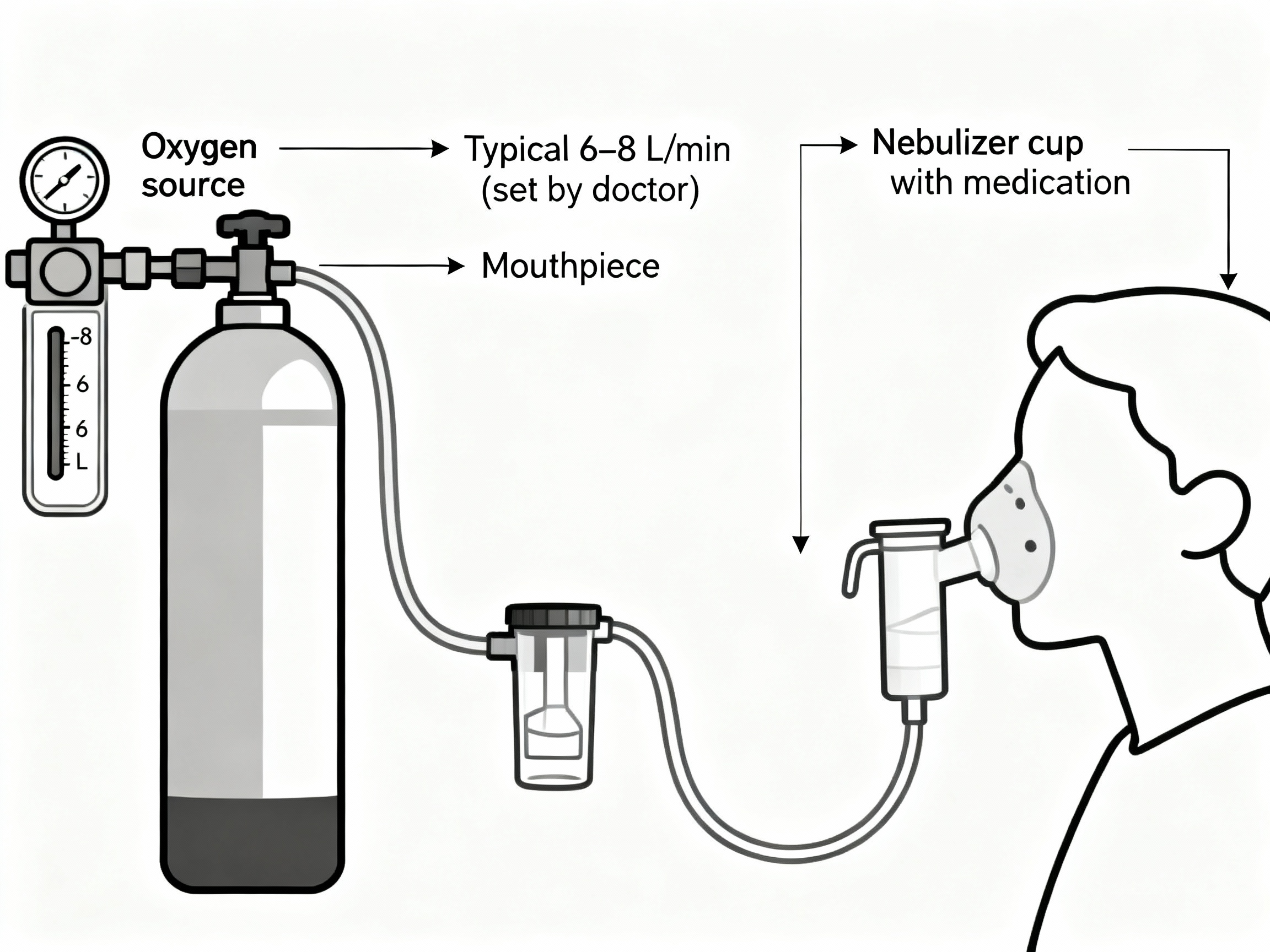
- If your doctor says it’s okay to power your nebulizer with oxygen, here’s a simple setup:
- If your doctor has you use oxygen to power the nebulizer, the flow is typically set around 6–8 L/min to create a steady mist. Don’t change your oxygen setting unless your doctor told you to.
- Connect the oxygen tubing from your oxygen source (oxygen concentrator or oxygen tank with regulator) to the nebulizer cup’s inlet (instead of the compressor hose).
- Add your prescribed medication, put on the mouthpiece or mask, and breathe as usual until the cup sputters (about 5–10 minutes).
- When you’re done, return to your usual oxygen routine and reconnect your nasal cannula if you took it off.
Tip: If you normally need oxygen continuously, keep your switch-back steps ready so you don’t stay at a higher flow by accident.
Most nebulizer cups need about 6–8 L/min when oxygen is used as the driving gas to aerosolize medication well.
Caption: How to connect oxygen to a nebulizer cup (flow typically set by your doctor).
Using a Nebulizer While Wearing a Nasal Cannula
If you use a standard nebulizer machine (which runs on room air), you can usually keep your nasal cannula on and use a mouthpiece at the same time. If you need a nebulizer mask, some people tuck the cannula inside the mask so a little oxygen still flows to the nose during the treatment. Ask your doctor what they prefer for you if you use a nebulizer mask.
If you remove your cannula for a mask treatment, put it back on right away when you’re done.
Mesh nebulizers can help you take medication anywhere. If you’re on prescribed oxygen, keep using your oxygen as directed during treatments.
Keep your oxygen routine steady and add the nebulizer on top of it.
Talk to your doctor before changing how you use oxygen or medications.
Oxygen vs Air: Which Should Drive Your Nebulizer?
For most people, either option can work. If you already need oxygen, using it to power your nebulizer can cover both needs at once. If you don’t need oxygen, the usual setup is a compressor that uses room air.
In some severe COPD cases, too much oxygen can reduce breathing drive, letting CO₂ build up. Important exception: Some people with severe COPD who retain carbon dioxide (CO₂) can get a rise in CO₂ when breathing high oxygen during nebulization. In one study, CO₂ rose by about 7.7 mmHg when 100% oxygen was used to drive the neb in CO₂-retaining patients. Doctors commonly prefer an air-driven nebulizer (and give oxygen separately if needed) for these patients.
If you have CO₂ retention or you’re not sure, ask your doctor which gas you should use to drive your nebulizer.
If you retain CO₂ with COPD, an air-driven nebulizer is usually preferred; if you need oxygen, your doctor might approve oxygen-driven treatments.
Safety first: Oxygen is a prescription. Don’t change your oxygen flow or medication routine without your doctor’s guidance. Talk to your doctor before trying a new medication or changing how you nebulize on oxygen.
Step-by-Step Safety Tips for Nebulizing on Oxygen
- Use the right flow. Use the oxygen flow your doctor recommended for nebulizing (commonly higher than your usual oxygen setting).
- Don’t exceed your plan. Only increase oxygen flow for nebulization if your doctor told you to, and set it back right after.
- Sit upright. Stay seated and relaxed during the treatment so tubing doesn’t pull and you can breathe deep, slow breaths.
- Switch back right away. As soon as the neb is done, reconnect your cannula and return to your normal oxygen setting.
- Keep it safe. No smoking or open flames around oxygen. Keep tanks stable and tubing out of walkways.
- Keep it clean. Clean and dry your nebulizer parts as directed to reduce infection risk.
- Watch how you feel. If you get very drowsy, confused, or more short of breath, stop and contact your doctor.
- Know when to get urgent help. If you have severe shortness of breath, blue lips or face, chest pain, confusion, or can’t speak in full sentences, call 911 or seek emergency care right away.
Using the right flow, clean equipment, and switching back to your normal oxygen setting right away keeps this combination safe.
Frequently Asked Questions
Tap or click a question below to see the answer:
Usually no. If you’re on continuous oxygen, keep it going—use a mouthpiece with your cannula in place, or if you use a mask, put the cannula back on right after the treatment.
Most standard neb cups need about 6–8 L/min to produce a good mist when using oxygen as the driving gas. Check with your doctor for your exact setting. If your device can’t reach that, use your regular compressor.
Not by itself. If your oxygen improves after a treatment, it’s usually because medicine opened your airways. A nebulizer cannot replace an oxygen tank or concentrator for low oxygen.
No. Oxygen adds needed O₂ to your breath; a nebulizer does not. Claims that a nebulizer can replace an oxygen cylinder are baseless.
No. A nebulizer delivers medication as a mist, while oxygen therapy delivers oxygen gas to raise blood oxygen. They’re different but often used together.
No. Steam inhalers warm and humidify air. Nebulizers turn prescribed liquid medication into a fine mist for your lungs—don’t use a steam inhaler for prescription breathing medications.
Medical Disclaimer
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, oxygen settings, and medications.