On this page

Yes—stress and anxiety can trigger asthma attacks for some people. If you’ve wondered, “can stress and anxiety cause an asthma attack,” the short answer is yes: strong emotions and stress are recognized asthma triggers. This guide covers how it works, how to tell asthma from a panic attack, ways to cope, how to build an asthma action plan, tools like a portable nebulizer, and when to seek help.
How Stress and Anxiety Trigger Asthma Symptoms
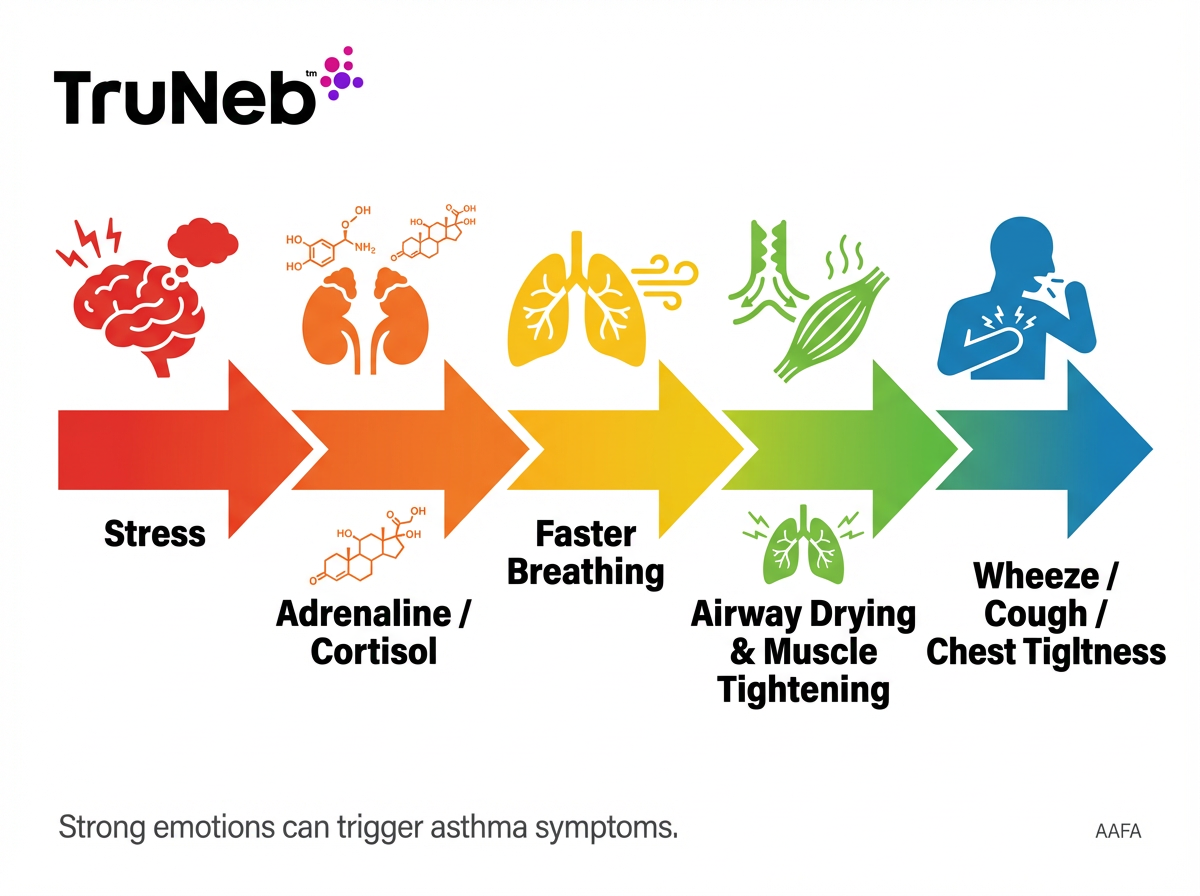
Stress and anxiety can set off real asthma symptoms. When your body goes into fight-or-flight, stress hormones like adrenaline and cortisol rise. Your breathing speeds up, chest muscles tense, and the tiny muscles around your airways can tighten. That mix can spark coughing, wheezing, and chest tightness.
Fast, shallow breathing (hyperventilation) can also dry and cool your airways. Dry, cool airways react by narrowing more, which can make you feel short of breath. On top of that, stress can nudge your immune system toward more inflammation. Inflamed airways are extra sensitive, so it takes less to trigger an episode.
Strong emotions can be triggers too. Anger, fear, excitement, crying, and big laughter change your breathing pattern and can start a stress-induced asthma attack if your airways are already sensitive. Anxiety can also trigger asthma symptoms in people with sensitive airways. This isn’t “all in your head.” Emotions kick off physical changes in your lungs.
Stress is one trigger among others like allergens, smoke, and respiratory infections—it doesn’t cause asthma by itself. People differ—not everyone with asthma reacts to stress the same way.
If your doctor has given you an asthma action plan, you can name the trigger, slow your breathing, and follow your plan early.
Bottom line: Stress and anxiety can trigger asthma by speeding your breathing and tightening the muscles around your airways.
Asthma Attack or Anxiety Attack? Knowing the Difference
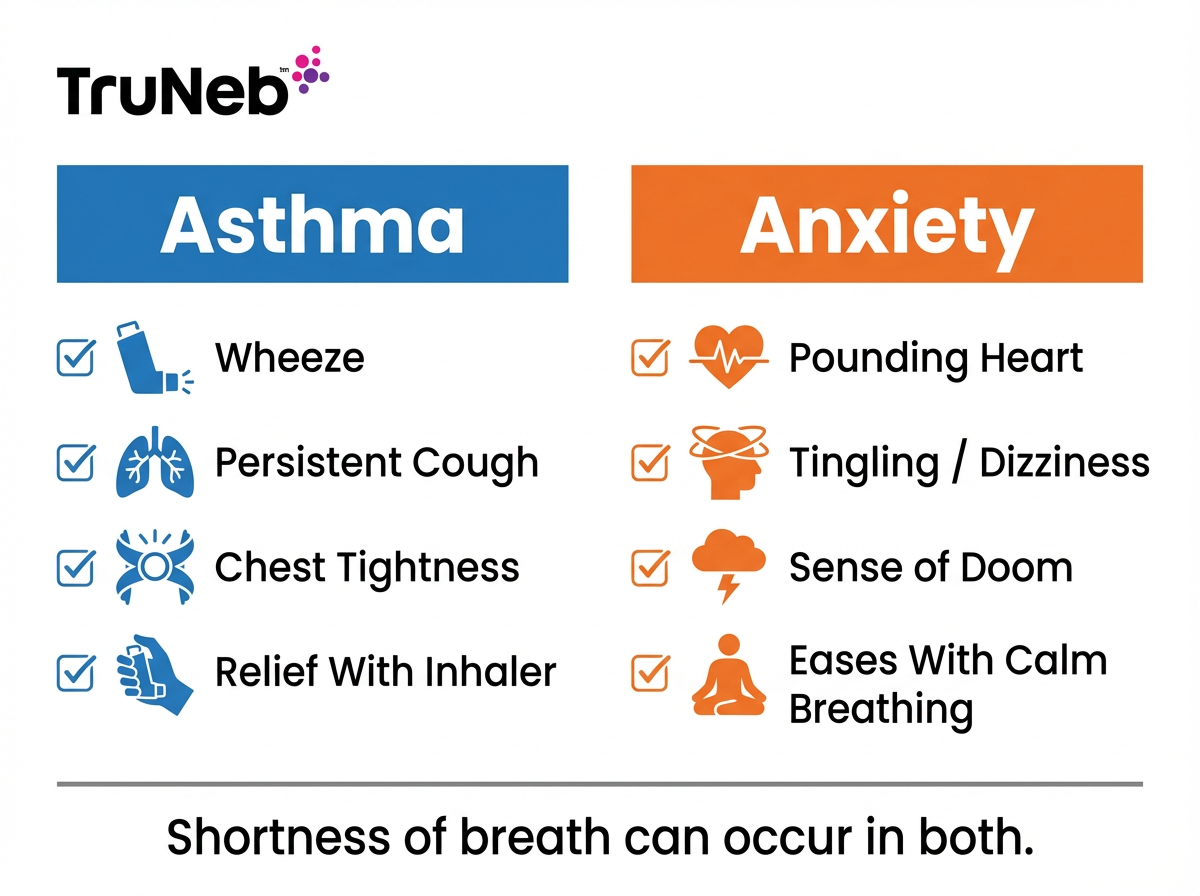
Asthma tends to include:
- Wheezing you can hear, a cough that won’t stop, and a tight chest.
- Trouble exhaling and a feeling of trapped air.
- A clear trigger like allergens, smoke, exercise, or strong emotions.
- Relief after using a quick-relief inhaler as prescribed.
Anxiety or panic tends to include:
- Pounding heart, shaking, tingling hands, dizziness, or nausea.
- A wave of fear or a sense of danger.
- Shortness of breath without wheeze; lungs often sound clear.
- Peaks within minutes and eases with calm breathing and grounding.
Shared signs:
- Shortness of breath and chest tightness. That overlap makes it confusing.
Simple self-check: If you have asthma and you’re wheezing or coughing, treat it like asthma and follow your action plan. If it’s mostly fear, tingling, and dizziness without wheeze, focus on slow breathing and grounding. They can happen together, so handle the breathing first, then calm the anxiety after.
This quick check doesn’t replace a medical evaluation—if you’re unsure or symptoms feel severe, seek urgent care. If you already have an asthma diagnosis, using your prescribed inhaler as directed is safe while you get help.
One-liner: Wheezing and cough point to asthma; tingling, dizziness, and intense fear lean toward a panic attack.
The Vicious Cycle – Stress, Anxiety, and Asthma
Stress can make asthma worse, and difficult breathing can raise your stress. That back-and-forth is a loop.
When stress runs high, you can breathe faster, your chest tenses, and your airways can narrow. You might also skip routines that protect your lungs, like taking your controller inhaler or other daily asthma medicine on schedule or getting solid sleep. Over time, extra inflammation can make asthma harder to control. Research shows that chronic stress and ongoing anxiety are linked with poorer asthma control—more frequent flares and more missed activities.
When asthma flares, the feeling of not getting enough air can be scary. That fear adds more stress, which can tighten your chest again. The key is to notice the loop and put simple tools in place to break it: slow breathing, a short reset, and a clear action plan.
If you’re finding it hard to break the cycle, ask your doctor or a mental health professional for help. Support and simple stress skills can make a real difference.
One-liner: Stress and asthma feed each other, but early breathing resets and a plan can break the loop.
Effective Coping Strategies for Asthma and Anxiety
Use these exercises alongside, not instead of, your prescribed asthma treatment.
Calm breathing:
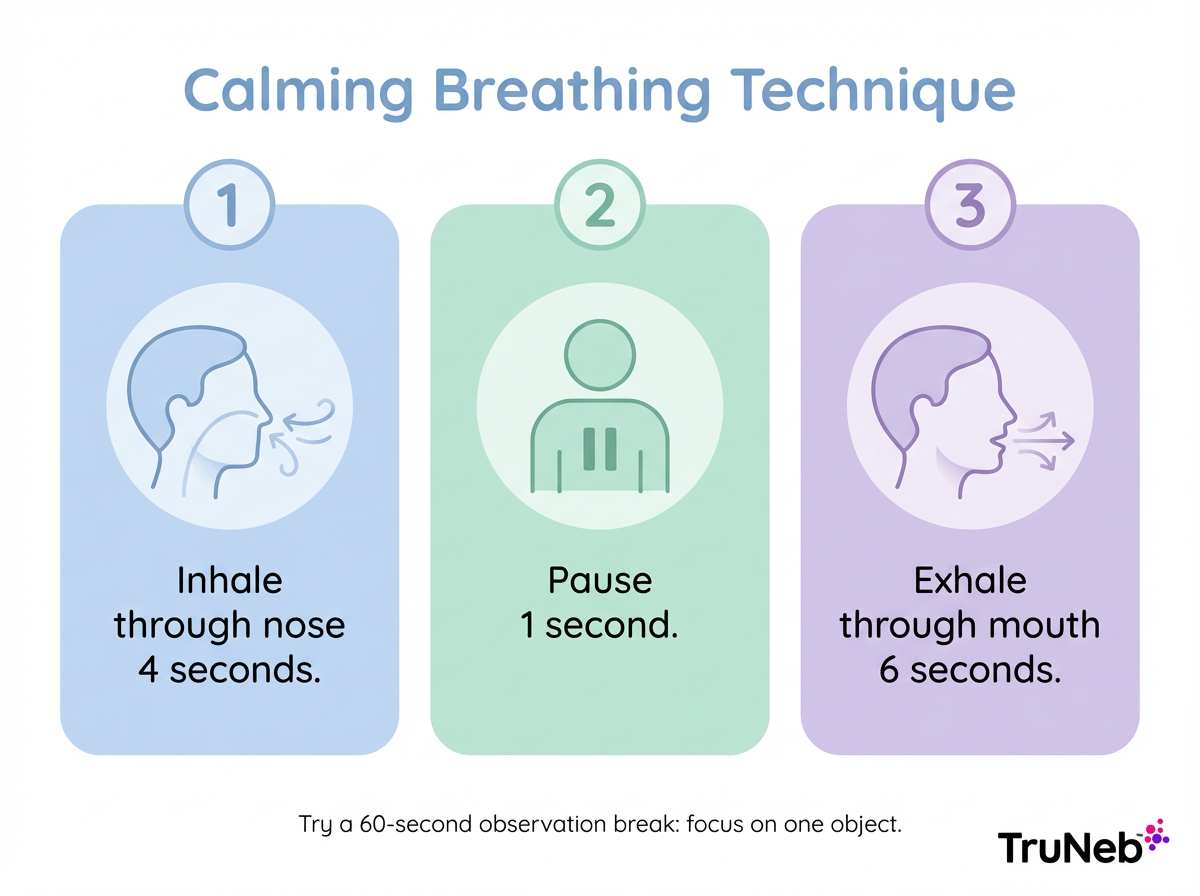
- Some people find this pattern helpful: inhale through your nose for 4 seconds, pause 1, exhale through your mouth for 6. Repeat 1–2 minutes. Keep your shoulders relaxed. Start at the first sign of stress.
- If your mind races, try a 60-second “observation” break: pick one object and notice its color, shape, and texture.
Relaxation and mindfulness:
- Gentle practices like progressive muscle relaxation or a short guided meditation can release chest and neck tension.
Move and sleep:
- Regular walks, light cycling, or yoga can lower overall anxiety and support lung health. A steady sleep routine helps your body cope better.
- If your asthma isn’t well controlled, check exercise choices with your doctor.
Limit stimulants and triggers:
- If caffeine makes you jittery, cut back on high-stress days. Avoid smoke and other known triggers when you’re run-down.
Support and counseling:
- A support community or a therapist can teach skills to handle anxiety that also make asthma easier to manage. Cognitive behavioral therapy (CBT) is commonly helpful.
Medication check-in:
- Well-controlled asthma flares less under stress. If tension regularly sets off symptoms, ask your doctor if your action plan needs an update. Never change medicines on your own.
Practice these skills when you’re calm, so they’re ready when you need them.
One-liner: Practice calm breathing early and pair it with a quick grounding trick before symptoms build.
Prepare an Asthma Action Plan for Stress Triggers
Work with your doctor to update your written asthma action plan so it includes stress triggers.
Write stress into your asthma action plan so you know exactly what to do when tension rises.
What to include:
- Early signs: Note what stress feels like in your body (tight shoulders, racing thoughts) and any breathing changes.
- First steps: Move to a quieter spot, start calm breathing for 1–2 minutes, and use your quick-relief inhaler as prescribed if breathing stays tight.
- Tools: Keep rescue meds where you need them most. If your doctor has prescribed nebulizer treatments for bad episodes, plan when and how to use them.
- On the go: A TruNeb™ portable mesh nebulizer can help you take prescribed treatments when coordinating a deep breath is hard. It’s small and quiet, which can lower stress in public places. Add it only with your doctor’s guidance.
- Early warnings: Some plans include a peak flow meter to catch early drops in lung function during stressful periods. Ask your doctor if this tool fits your plan.
- Track and share: Keep a simple log of stress levels and symptoms. Bring it to your next visit so your doctor can personalize your plan.
Keep a copy in your phone and another at home.
One-liner: Add stress steps to your plan so you can act early and breathe easier.
Tools for Relief – Nebulizers and Hypertonic Saline
A nebulizer turns liquid medicine into a fine mist you breathe in. This can help when you’re too tense to coordinate an inhaler breath. A compact, quiet mesh device, fits in a bag and can be used at work, school, or travel when prescribed.
Doctors sometimes recommend nebulized hypertonic saline to thin mucus and make coughs more productive. Common concentrations are 3% and 7% hypertonic saline. TruNeb offers these options for people whose care plans include saline. Hypertonic saline isn’t right for everyone with asthma—your doctor will decide if it fits your plan.
Key takeaway: Mesh nebulizers are portable and quiet for doctor-prescribed asthma medicines; steam inhalers aren’t for asthma meds.
| Device | Portable | Noise | Works with asthma meds | Typical use | Cleaning |
|---|---|---|---|---|---|
| Mesh nebulizer | Yes (pocket-sized) | Quiet | Yes (doctor-prescribed liquids, incl. hypertonic saline when indicated) | On-the-go relief when coordination is tough | Rinse/disinfect parts per manual |
| Jet (compressor) nebulizer | Home or portable with compressor | Louder | Yes | Home treatments | Clean cup/tubing as directed |
| Steam inhaler | Yes | Quiet to moderate | No | Comfort moisture only | Clean per device instructions |
Steam inhalers produce warm mist for comfort; they don’t deliver asthma medications.
⚠️ If you see boxes labeled “steam inhaler,” don’t use them for asthma medications—steam inhalers are different devices and aren’t made for asthma medicines.
Safety note: Talk to your doctor before trying a new medication or nebulized saline. Use only what’s on your written plan, and clean your device as instructed.
One-liner: A portable mesh nebulizer can deliver doctor-prescribed treatment when stress makes inhaler use tough.
When to Seek Help (Don’t Ignore Severe Signs)
Call emergency services if breathing is getting worse fast. Red flags include: struggling to speak full sentences, lips or fingernails turning blue, ribs pulling in with each breath, severe chest tightness, or no relief after using your rescue inhaler as prescribed.
If you can’t tell if it’s asthma or panic, treat it like asthma first and follow your action plan. If you already have an asthma diagnosis, using your prescribed rescue inhaler as directed is safe while you get help. If you’re not improving or you feel faint, call 911. Medical teams can support your breathing and also help calm the anxiety response.
If you’re not sure whether to go to the ER, call your doctor’s office or an urgent care line for advice.
Make a non-emergency appointment if stress often triggers symptoms, your rescue inhaler use is rising, or you’ve started avoiding activities out of fear. Your doctor can adjust your asthma plan and connect you with support for anxiety. If anxiety about asthma is constant or affecting daily life, a mental health professional can help.
As always, don’t start, stop, or change prescriptions without talking to your doctor.
Stress and anxiety can trigger real asthma symptoms, but planning and support help. Work with your doctor, practice calm breathing, keep your written action plan handy, and ask whether tools like a portable mesh nebulizer fit your plan.
One-liner: If you can’t speak in full sentences, your meds aren’t helping, or you’re turning blue, call 911.
FAQs – Stress, Anxiety, and Asthma
Tap or click a question below to see the answer:
Yes. Intense emotions like stress, fear, anger, or excitement can change your breathing and tighten the muscles around your airways, which can trigger asthma symptoms if your airways are sensitive.
Wheezing and a stubborn cough point to asthma. Tingling, dizziness, and a surge of fear lean toward panic. If you have asthma, follow your action plan first. Calm-breathing techniques help both.
Use your quick-relief inhaler as prescribed, then slow your breathing: in through your nose for 4 seconds, out through your mouth for 6. Relax your shoulders and focus on one object to ground yourself. If you don’t improve, seek emergency care.
It can. Ongoing stress can increase airway inflammation and make your lungs more reactive. It can also disrupt routines, like regular meds and sleep, that keep asthma controlled.
Treating anxiety with skills like CBT or other therapies can reduce stress-triggered flares. Anxiety care supports, but doesn’t replace, your asthma treatment. Coordinate with your doctor.
Some quick-relief medicines can cause jitters or a fast heartbeat. Knowing this side effect can help you stay calm. If it bothers you, ask your doctor about options.
One-liner: Strong emotions and anxiety can affect both your breathing and your asthma control, so work with your doctor on both your lungs and your stress.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, asthma plan, and any changes to your medications or mental health care.







