On this page
Obesity and Asthma: Understanding the Connection
Obesity doesn't cause asthma in everyone, but it raises your risk and can make asthma harder to control.
Doctors generally define obesity as a body mass index (BMI) of 30 or higher.
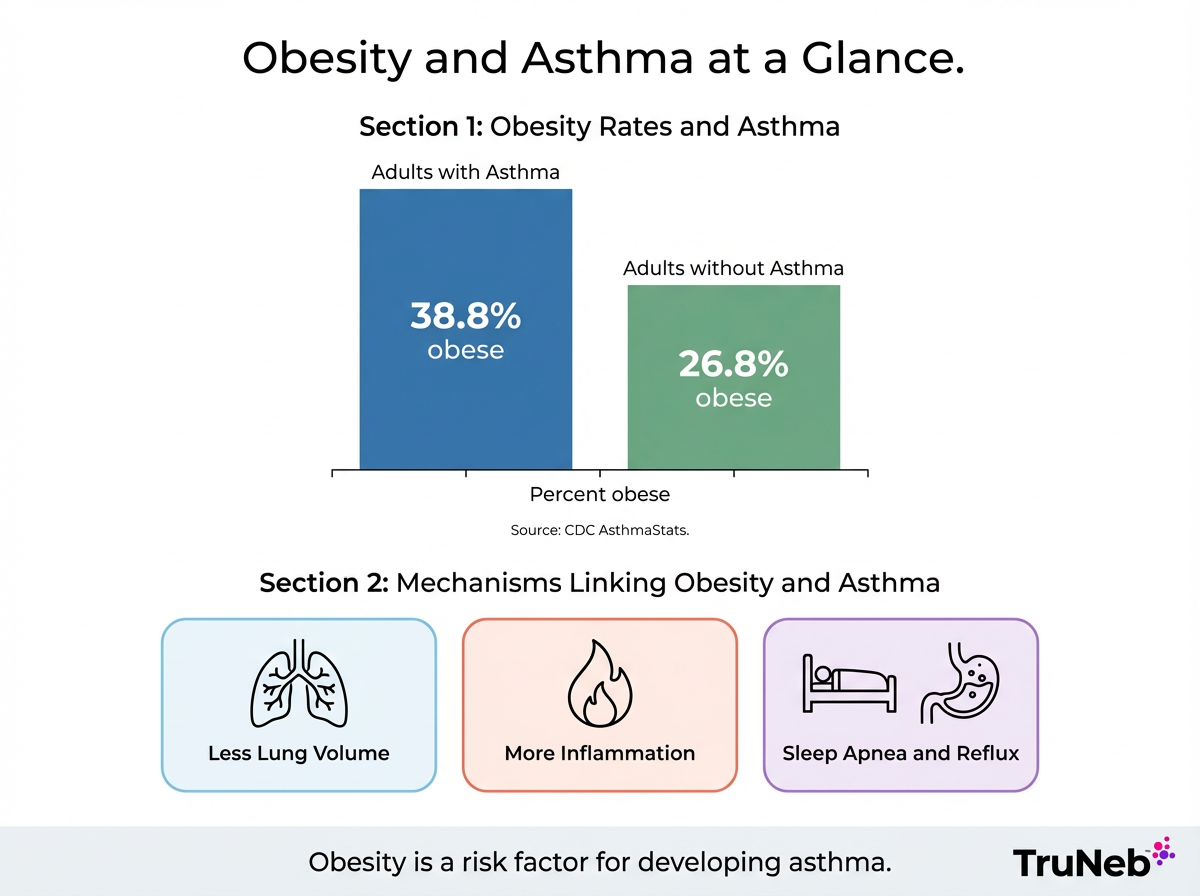
The CDC lists obesity as a risk factor for developing asthma. In national data, 38.8% of adults with asthma were obese, compared to 26.8% of adults without asthma.
Why this happens: extra weight can squeeze your lungs and add body-wide inflammation. That makes airways more sensitive and more likely to tighten.
In short, obesity raises both your chances of developing asthma and your chances of having more stubborn symptoms if you already have it.
How Excess Weight Affects Breathing and the Lungs
Extra weight, especially belly fat, presses up on your diaphragm and chest wall. That leaves less room for your lungs to expand. It can feel like wearing a heavy vest on your chest.
This extra pressure means your lungs can't fully expand, so breathing feels harder even with small efforts.
Common signs include:
- Shortness of breath with small efforts like climbing stairs.
- Tightness when lying flat because the diaphragm is pushed upward.
- Shallow breathing that lets small airways close more easily.
Lower lung volumes make the airways easier to irritate and easier to narrow. This can mimic asthma or make diagnosed asthma flare more readily, especially at night.
Inflammation and Immune Changes in Obesity-Related Asthma
Fat tissue is active. It releases inflammatory signals into your bloodstream. These signals, including leptin and other cytokines, can make your airways more irritable and swollen.
In simple terms: extra fat can put your body in a more inflamed state. Inflamed airways are the core of asthma, so this background inflammation adds fuel to symptoms and flare-ups. Research shows obesity-related asthma sometimes doesn't respond as well to standard inhalers.
Newer science points to more clues. Harvard researchers identified a gut hormone called CCK that seems to play a role in airway narrowing in obesity-related asthma. Researchers are still studying this, and it isn't part of everyday asthma care yet.
Together with the mechanical squeeze on your lungs, this background inflammation makes your airways more likely to tighten and stay irritated.
Why Asthma Is Often Harder to Control in People with Obesity
People with obesity and asthma tend to have more symptoms, more flare-ups, and more limits on daily life. Health records show higher medication use and more hospital visits.
Two big reasons:
- Airway inflammation and reduced lung volume make small triggers feel big.
- Some studies find common asthma medicines don't work as well at higher BMIs.
What you might see day to day:
- Using a rescue inhaler several times a week.
- Nighttime coughing or wheezing.
- Slower recovery after colds.
Mood issues like depression are more common with obesity and can make asthma management feel harder.
If your asthma feels stubborn, you're not imagining it—targeted steps can help.
Sleep Apnea and Acid Reflux Can Worsen Night Symptoms
Obstructive sleep apnea and acid reflux both common with obesity can trigger or worsen asthma symptoms at night.
Two common conditions in people with obesity can fire up nighttime asthma symptoms like coughing or wheezing and make asthma harder to control while you sleep:
- Obstructive sleep apnea: airway collapse during sleep can trigger coughing and wheezing. People can wake up breathless and feel tired during the day.
- Acid reflux: acid that moves upward can irritate your airways, leading to chest tightness and cough when you lie down.
When these conditions are treated, asthma control can improve. Your doctor might recommend a sleep study if you snore, gasp at night, or wake unrefreshed. Simple steps like eating earlier, raising the head of your bed, and using medicines your doctor prescribes can help limit reflux. Managing these hidden culprits can reduce nighttime wheeze and cough.
| Condition | How it worsens asthma at night | Common clues | How doctors evaluate | What can help |
|---|---|---|---|---|
| Obstructive sleep apnea | Airway collapses during sleep, causing drops in oxygen and airway irritation that can trigger cough and wheeze. | Loud snoring, gasping or pauses in breathing, morning headaches, daytime sleepiness. | Sleep study (home or lab) to measure breathing, oxygen, and sleep quality. | Treatments like CPAP, weight loss, side-sleeping; follow your doctor's plan. |
| Acid reflux | Stomach acid moves upward and irritates the throat and airways, especially when lying down. | Heartburn, sour taste, cough that worsens at night or after meals. | Clinical history; sometimes pH monitoring or endoscopy if symptoms persist. | Meal timing changes, raising the head of the bed, medicines your doctor prescribes. |
Note: This table is for general information. Talk with your doctor for diagnosis and treatment.
Can Losing Weight Improve or Even Cure Asthma?
Losing weight can improve asthma control. People breathe easier, need less rescue medicine, and have fewer attacks as pounds come off. Even a 5 to 10 percent loss can make a clear difference.
Is it a cure? Not always. If your asthma is driven by allergies or genetics, you can still have it. Even if symptoms go into remission, asthma can return, so you'll still need to keep an eye on your breathing and follow your plan.
Bonus: weight loss also reduces reflux and lowers the risk of sleep apnea, which further calms night symptoms.
Extra weight makes asthma worse, so you feel too breathless to move much. Moving less makes it easier to gain more weight, which then worsens asthma again. Breaking this cycle—even with small, steady changes—can make breathing and daily life feel easier.
Managing Asthma When You Carry Extra Weight
Managing asthma when you carry extra weight means fine-tuning your medicines, treating hidden issues like reflux or sleep apnea, and making steady lifestyle changes. Work with your doctor to create a personalized Asthma Action Plan. Tell your doctor about night symptoms, heartburn, or snoring so you can treat those too.
Make your medicines work harder:
- Check your inhaler technique; a spacer can help medicine reach deeper into your lungs.
- If inhalers are hard to use during flares, a nebulizer can make treatment easier by turning medicine into a gentle mist you breathe in slowly.
A portable mesh nebulizer like TruNeb is designed to be small, quiet, and easy to carry, so you can take treatments with you. Use a portable nebulizer only as your doctor prescribes. Some doctors also use nebulized saline in certain lung conditions or for people with thick mucus. Talk to your doctor about what's right for you.
⚠️ Steam inhalers are not the same as nebulizers. They're not designed to deliver asthma medications into your lungs. Only use medication in a nebulizer if your doctor prescribes it.
Tackle hidden culprits and lifestyle:
- Adjust meal timing, raise the head of your bed, and use medicines your doctor prescribes to help limit reflux.
- If sleep apnea is suspected, your doctor can arrange a sleep study, and treatments like CPAP can improve both sleep and breathing.
- Aim for steady, realistic weight loss with a plan you can keep. Short, low impact activities like walking or swimming are a strong start.
Safety note: Talk to your doctor before trying any new medication or saline treatment, or before making big changes to your asthma plan.
⚠️ Seek emergency medical care right away (call 911 or your local emergency number) if you have severe shortness of breath, trouble speaking in full sentences, chest pain, blue lips or face, or if your rescue inhaler isn't helping.

Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. Two common causes are obstructive sleep apnea and acid reflux. Both are more common with obesity and can trigger nighttime coughing and wheezing. Treatments like CPAP for sleep apnea and reflux strategies such as diet changes or medicine your doctor prescribes can reduce night symptoms and improve overall control.
Not always, but it can make a big difference. People can see fewer symptoms, less need for rescue inhalers, and better lung function after losing weight. If allergies or genetics drive your asthma, you can still have it, but it can become much milder and easier to manage. Even if symptoms go into remission, asthma can return, so keep following your plan.
Asthma itself can make weight loss harder when symptoms limit activity, and short courses of oral steroids for flare-ups can increase appetite. Daily inhaled steroids usually have minimal whole-body effects. Good control helps you stay active with a plan that fits your breathing.
You'll use the same core treatments, but your plan is usually tailored. Doctors also treat reflux and sleep apnea alongside asthma because those fixes help control. Some medicines are adjusted over time. A nebulizer is sometimes used when inhalers are hard to use during flares. Talk to your doctor before changing any medicine.
Yes. The link exists in both children and adults. Obesity raises asthma risk and can worsen symptoms in kids and adults. In children, asthma can also reduce activity and lead to weight gain over time. Keeping a healthy weight in childhood usually improves control and lowers problems later.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options.