On this page

Asthma Is a Lifelong Condition – But Remission Is Possible
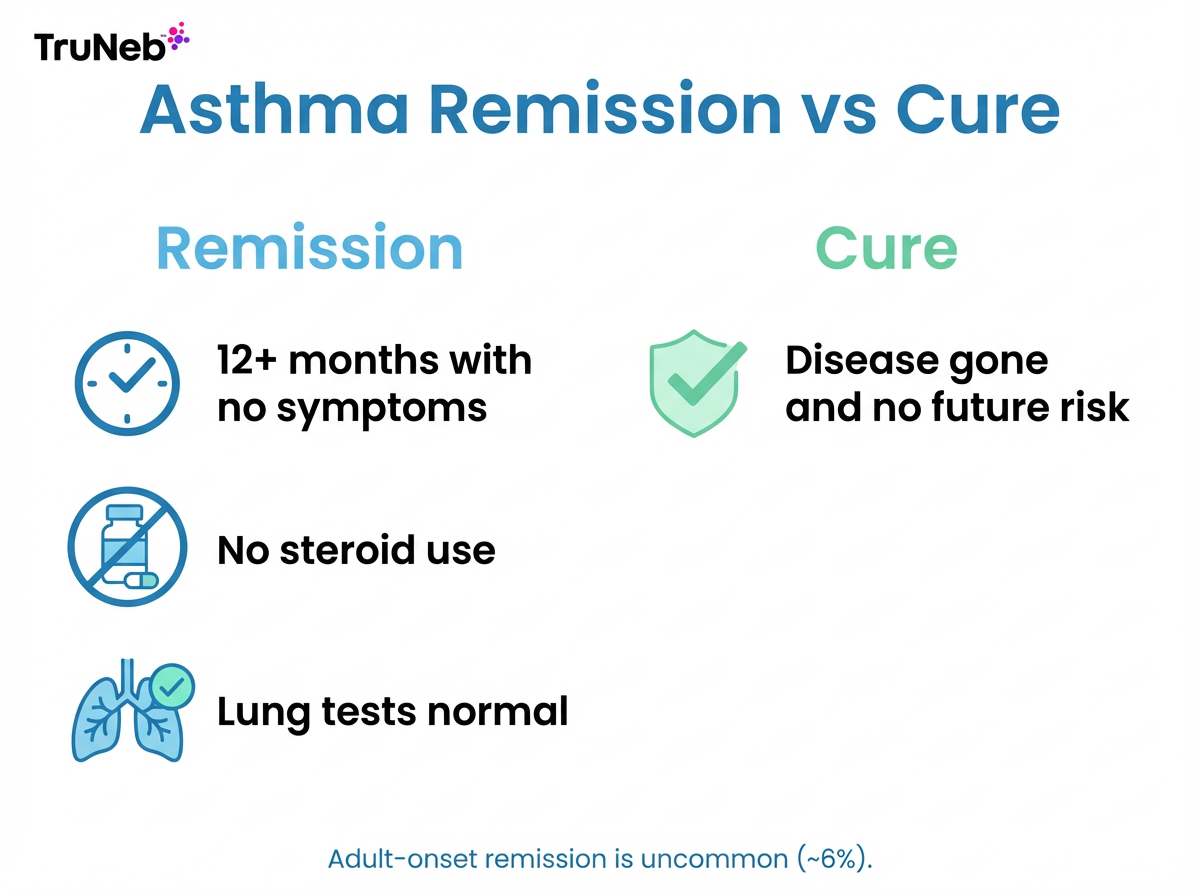
Asthma usually doesn’t go away on its own. It’s a long-term disease of the airways in your lungs, where those airways stay prone to inflammation. It mainly affects the bronchial tubes that carry air in and out of your lungs. Doctors sometimes talk about asthma remission vs cure to make this distinction clear.
In remission, you have no symptoms and you aren’t using steroids for 12 months or more, and your breathing tests look normal. That’s called remission, not a cure — the airway inflammation tendency is still there even when you feel normal. Groups like the American College of Allergy, Asthma & Immunology note that there’s no permanent cure for asthma.
Bottom line: asthma can go quiet for a long time, but it isn’t considered cured — it’s better to think of those quiet years as remission.
Outgrowing Childhood Asthma
Many kids see asthma fade in the teen years, especially if symptoms were mild. As kids grow, their airways get larger, their lungs mature, and their immune systems change. For some, that means less airway narrowing and fewer asthma symptoms.
What makes remission more likely:
- Mild, infrequent symptoms.
- Few or no other allergies like eczema or hay fever.
- Good lung function and less airway inflammation.
- Boys often improve during adolescence as airways grow.
- Wheezing only with colds that fades as the immune system matures.
Why some kids don’t outgrow it: children with moderate or severe asthma, multiple allergies, or a strong family history are more likely to have asthma into adulthood, and outgrowing it isn’t guaranteed even with mild disease. Studies suggest that a good share of kids with mild asthma become symptom-free as adults, while only a small minority of people whose asthma starts in adulthood reach remission (around 6% in some studies).
Even if symptoms stop, keep asthma in your medical history and stay prepared. Remission can last for years, and that’s great, but it isn’t guaranteed forever.
Takeaway: childhood asthma that eases is remission, not a cure.
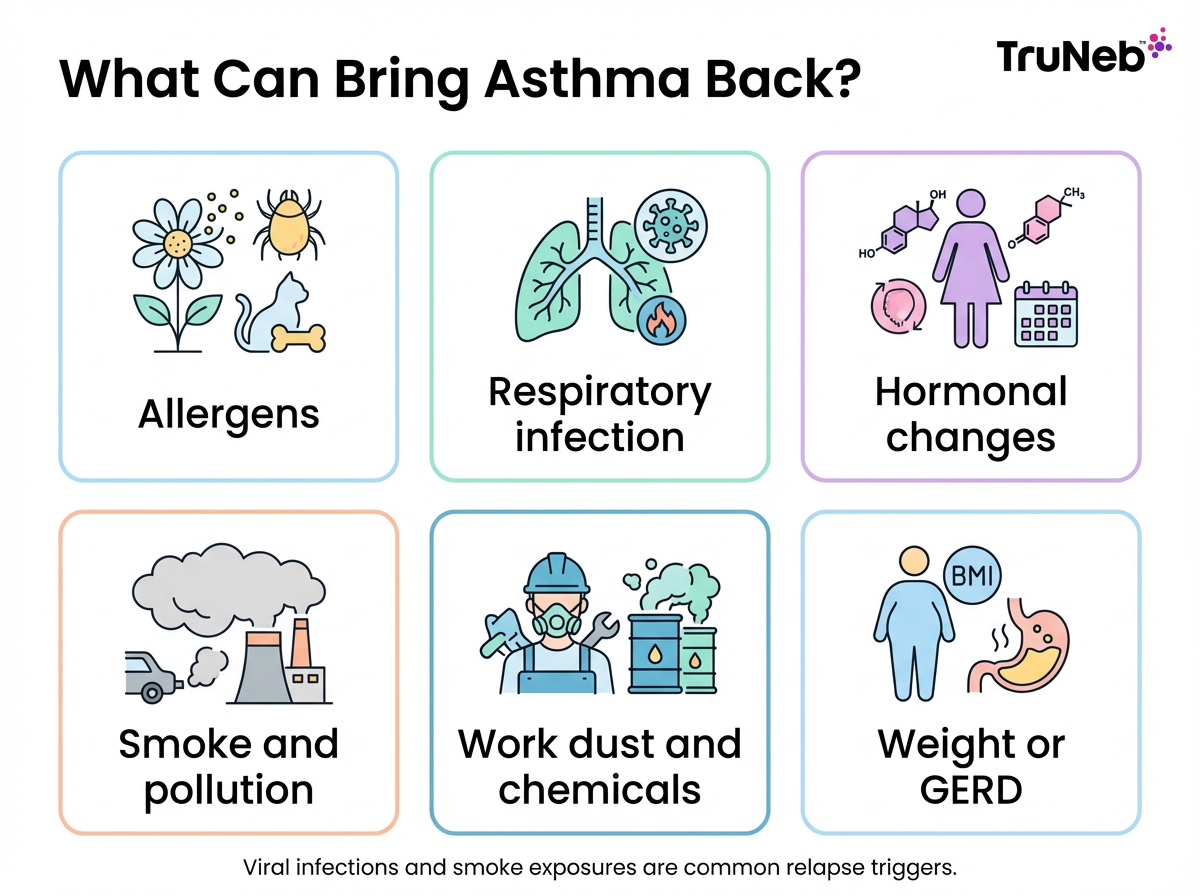
When Asthma Symptoms Return in Adulthood
Even after years of quiet, asthma can come back. Research shows that a noticeable share of people whose childhood asthma seemed to disappear get symptoms again in their 20s — doctors sometimes call this a relapse.
Common triggers:
- New allergen exposure: dust mites, pet dander, pollen, mold.
- Respiratory infections like a bad cold or flu.
- Hormonal changes and aging.
- Smoke and air pollution, including secondhand smoke.
- Job exposures to dust or chemicals.
- Weight gain or reflux that irritates airways.
Early signs include night cough, wheeze with exercise, or needing your rescue inhaler again. If you notice these, see your doctor and update your plan.
⚠️ If you have severe trouble breathing, chest pain, blue lips or fingernails, or can’t speak in full sentences, seek emergency medical care right away.
Key point: asthma that was quiet for years can flare again when a new trigger shows up — whether doctors call it a relapse of childhood asthma or new adult-onset asthma, it still needs attention.
How to Stay in Control Even If You Feel Better
Keep your plan steady even when you feel great. It protects those quiet months.
Staying on your plan can help protect your lungs over time, not just prevent day-to-day symptoms.
Continue your medication and monitoring
- Talk with your doctor before changing or stopping any controller medicine.
- Try to keep regular checkups, including spirometry, when your doctor recommends them.
- Use a written Asthma Action Plan from your doctor and watch for early symptoms or drops in your peak flow.
Avoid triggers and keep a healthy routine
- Taking steps to reduce dust and pollen at home can cut down on flare-ups.
- If you smoke, ask your doctor about support to quit, and try to avoid secondhand smoke.
- Staying active and keeping a healthy weight can make breathing easier over time.
- If allergies drive your asthma, ask about immunotherapy (allergy shots).
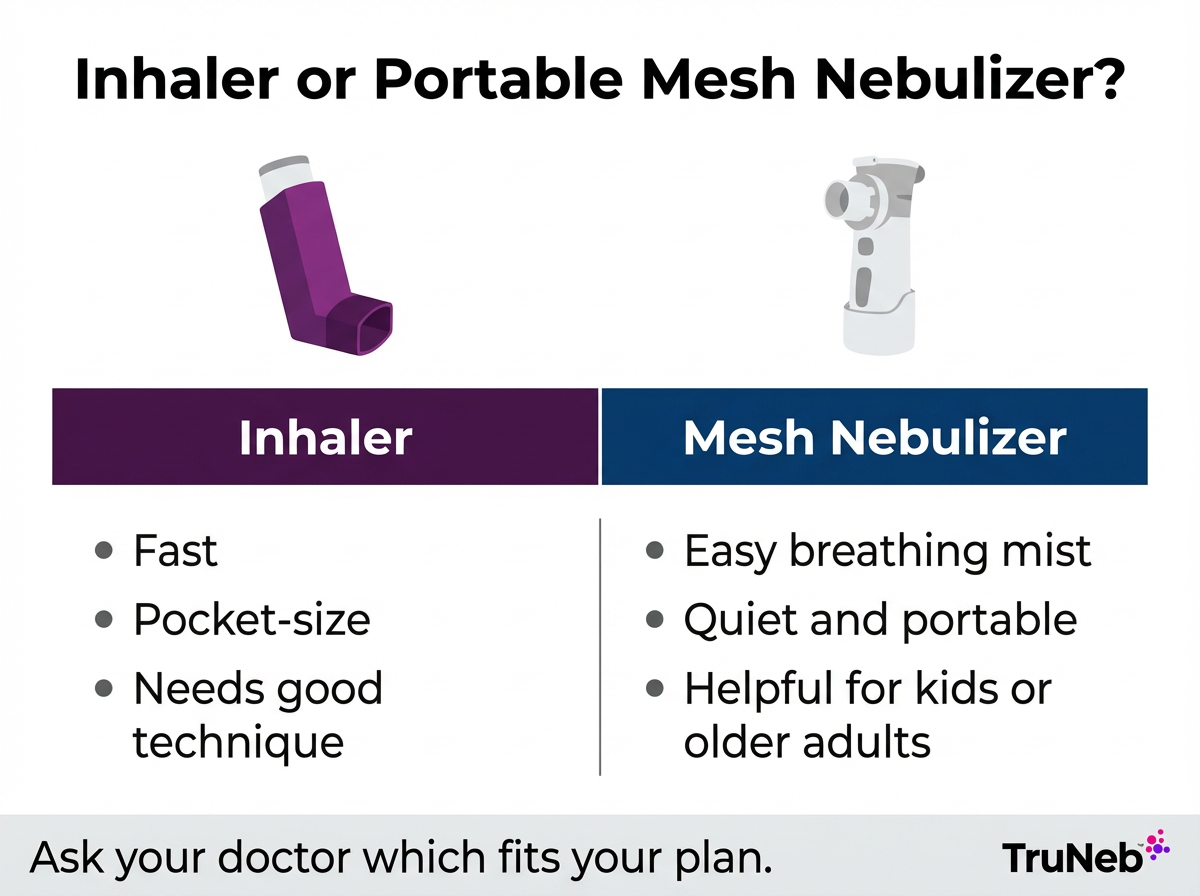
Have quick relief ready
- Most doctors recommend keeping a rescue inhaler with you and checking the expiration date from time to time.
- A nebulizer can be helpful if you struggle with inhalers or your doctor prescribes nebulized treatments during flares. A portable mesh device like the TruNeb™ Portable Mesh Nebulizer is quiet and travel-friendly, so it’s easier to take a breathing treatment at home or on the go when your clinician recommends one.
- Quick note on solutions: hypertonic saline is usually for mucus-heavy lung diseases and isn’t routine for asthma unless your doctor specifically advises it.
- ⚠️ If you see products labeled "steam inhaler," know these are not the same as nebulizers and shouldn’t be used to deliver prescription asthma medications.
Safety note: Talk to your doctor before trying a new medication or changing doses.
Takeaway: stay steady on your plan, avoid triggers, and keep fast relief close by.
Frequently Asked Questions
Tap or click a question below to see the answer:
Very unlikely. Untreated asthma often continues and can worsen. Some children see symptoms fade as they grow, but that’s not the same as being cured. It’s important to stay in touch with a doctor about your asthma, even when you feel well.
Asthma has no permanent cure. Good treatment can keep symptoms quiet for long stretches, but the tendency for airway inflammation remains.
Estimates vary by age and severity. Some studies suggest that over half of children with mild asthma have few or no symptoms as adults, while adult-onset remission is uncommon, around 6%. Remission isn’t a guarantee and isn’t a cure.
Yes. New allergens, a bad respiratory infection, smoke, or life changes can light up sensitive airways again. If symptoms return, see your doctor to review your diagnosis and update your plan.
Doctors usually recommend that people with a history of asthma keep a rescue inhaler handy and check the expiration date. Asthma can flare suddenly, even after a long quiet stretch.
You’re likely in remission. You may feel normal, but the tendency for airway inflammation can still be there. Keep avoiding triggers and follow your doctor’s advice.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, treatment options, and any changes to your asthma plan.