On this page
What Is Brown Phlegm?
Understanding Phlegm and Mucus
Phlegm and mucus get used interchangeably, but they aren’t exactly the same thing. Mucus is a sticky, protective substance your body produces in various places called mucous membranes. The respiratory and digestive tracts, for example, need mucus to trap bacteria, dust, and other particles. Phlegm is mucus from the lungs once it's coughed up. Now you know!
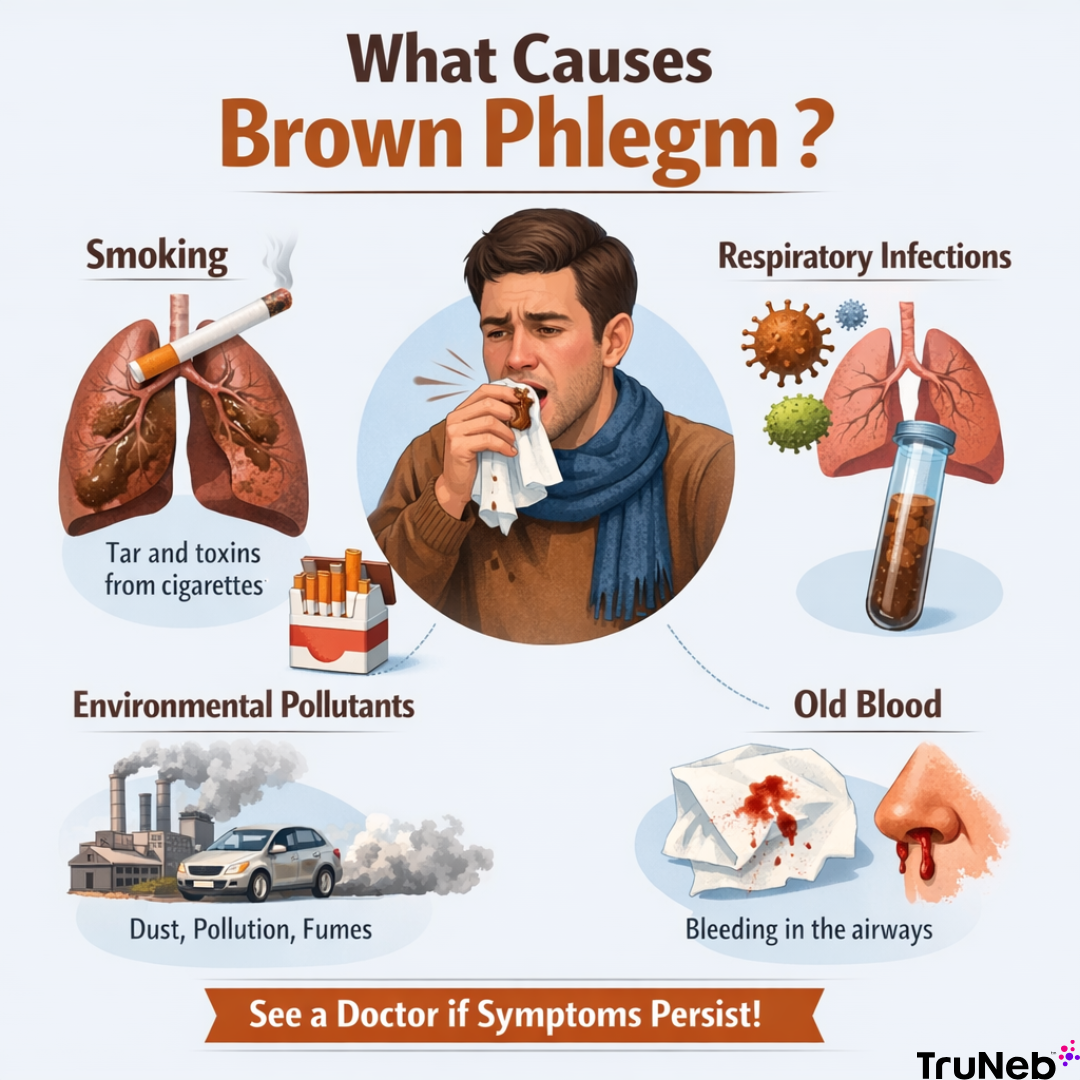
When phlegm changes color—especially to brown—it often means that something unusual is going on in your body. Brown phlegm usually points to old blood that’s been sitting in your lungs and has oxidized, which turns it that rusty brown shade. This can happen when your airways are inflamed, damaged, or irritated from smoking, environmental toxins, or chronic infections. Coughed up brown mucus is your body’s way of telling you something is off.
What Causes Brown Phlegm
Smoking and Brown Phlegm
Coughing up brown mucus from smoking isn't uncommon. The tar and toxins in cigarette smoke irritate your lungs, causing inflammation and excess mucus. Over time, your lungs try to clear out the gunk.
When you smoke, the tiny hair-like structures in your lungs, called cilia, get damaged. Normally, these cilia help sweep out mucus and debris, but smoking slows them down, making phlegm thicker and discolored.
Brown flecks in phlegm after quitting smoking is just your lungs expelling years of built-up tar. It's actually a positive sign of recovery!
Air Pollution and Environmental Irritants
If you’ve been around heavy dust, smoke, or smog (especially in places like construction zones or industrial areas), you might notice brown specks in your phlegm. That’s your lungs doing cleanup duty. When you breathe in dirty air, your body produces extra mucus to trap all those tiny irritants. Over time, all that gunk can tint your mucus brown. It might seem gross, but it’s a sign your body’s working to get rid of what doesn’t belong.
Respiratory Infections
Brown specks in phlegm (or just straight up brown phlegm) can show up when your lungs are fighting off an infection like bronchitis, pneumonia, or a lung abscess. These infections cause inflammation, and sometimes tiny blood vessels in your airways can break. When that blood sits in your lungs, it oxidizes and turns the mucus brown.
You might also see yellow or green mucus with these illnesses, but dark brown can point to something more serious or long-lasting. If it sticks around or comes with other symptoms, it’s a good idea to check in with a doctor.
Symptoms to watch for alongside dark mucus include:
- Fever
- Shortness of breath
- Chest pain
- Fatigue
Chronic Lung Conditions
Some long-term lung conditions, like COPD, bronchiectasis, or cystic fibrosis, can cause your body to produce thick, brown mucus. That’s because these illnesses keep your lungs irritated and prone to infections, which leads to constant mucus buildup and sometimes bleeding.
With COPD, your airways slowly get more inflamed and narrow over time. Breathing gets harder, and mucus starts to collect. That mucus can turn brown if there’s old blood or leftover tar from smoking. In bronchiectasis, the airways get stretched out and damaged, so mucus pools and infections keep coming back. People with cystic fibrosis deal with extra thick mucus that clogs the lungs. Over time, that irritation can lead to small bleeds, which show up as brown spots in phlegm.
What Does the Color and Texture of Brown Phlegm Mean?

Brown phlegm doesn’t always look the same. Sometimes it shows up as light brown flecks, and other times it’s thick and dark. Paying attention to those differences can give you clues about what’s happening in your body. It can also help you decide if it’s something you can manage at home or a sign you should talk to a doctor.
Brown Specks vs. Dark Brown Phlegm
- Brown Specks or Spots
If you’re seeing small brown flecks in otherwise clear or light-colored mucus, it might just be from minor irritation. This can happen when tiny blood vessels in your airways break—maybe from a hard cough or breathing in a lot of dust. If it only happens now and then and you feel fine otherwise, it’s probably nothing serious. But if the specks keep showing up or come with things like a fever or chest pain, it’s a good idea to check in with a professional. - Dark Brown Phlegm
Dark brown phlegm is thicker and harder to miss. It usually means there’s old blood in your lungs. That can happen when blood sits for a while and starts to break down, turning the mucus brown. This type of phlegm is more of a warning sign than a few brown specks. It can point to ongoing irritation, an infection, or even bleeding. If you’re seeing this regularly, set up an appointment as soon as possible.
Old Blood vs. New Bleeding in Phlegm
- Old Blood Turning Phlegm Brown
When blood has been sitting in your lungs or airways for a while, it oxidizes and turns brown. This can happen with conditions like lung abscesses, chronic bronchitis, or other long-standing infections. If you’ve got a condition like bronchiectasis, repeated infections can lead to small amounts of old blood in your mucus. - New Bleeding in Phlegm
Fresh bleeding in your lungs or airways will show up as red or pink phlegm, but as it mixes with other mucus, it can start to look brownish. Fresh bleeding is more concerning and can be caused by conditions like bronchitis, pneumonia, or severe irritation from smoking. If you see fresh blood turning your phlegm brown, don’t wait—seek medical help right away.
Home Remedies and Treatment Options for Brown Phlegm
Coughing up brown phlegm isn’t exactly pleasant, but there are some easy ways to help clear it up at home. Whether it’s showing up because of an infection or something like air pollution, these simple tricks can help loosen that sticky mucus and get it out of your system.
Hydration and Humidification
When you’ve got thick, dark brown phlegm stuck in your chest, staying hydrated is one of the best things you can do. Drinking lots of water helps thin the mucus, making it easier to cough up. It’s like watering down something that’s too thick so you can actually get it out. Aim for at least eight glasses of water a day—and more if you’re feeling dehydrated. If you have fluid restrictions, ask a doctor first!
Steam inhalation is another simple fix. Breathing in warm steam helps moisten your airways and loosens up that stubborn mucus. A hot shower is one way to accomplish this, or a device like a steam inhaler designed for this purpose.
- Tip: Try adding a few drops of eucalyptus or menthol to the water for an extra boost. It can help open up your airways and break up that dark brown phlegm even faster.
Saline Nasal Irrigation and Gargling
If you’re seeing brown specks in your phlegm, especially in the mornings after a night of coughing, a saline nasal rinse can help flush out the mucus and clear out your airways. Using a saline solution or neti pot will help rinse away the gunk that’s dripping down from your nose into your throat, making it easier to breathe and reducing irritation. Some people find nebulizing hypertonic saline majorly improves their ability to cough up phlegm.
Gargling with salt water is another super easy remedy that works wonders. It helps calm inflammation in your throat and loosens up the phlegm, making it easier to cough out those brown specks. Mix half a teaspoon of salt in warm water, gargle for 30 seconds, and spit it out. Do this a few times a day, especially in the mornings, when mucus tends to build up the most.
OTC Expectorants and Humidifiers
If your brown-colored phlegm feels like it just won’t budge, over-the-counter expectorants can really come in handy. These meds work by thinning the mucus, making it easier to cough up. Guaifenesin is the active ingredient you’ll want to look for—it basically turns that thick, sticky stuff into something easier to manage so you’re not constantly hacking away. And of course, always check with your doctor first before taking any medication.
Using a humidifier can also make a big difference, especially if you’re dealing with dry air at home. Dry air can thicken your mucus and make it harder to clear, but a humidifier keeps the air moist and helps your body manage the brown spots in phlegm more easily. In our 9 Amazing Gifts for Someone With COPD article, our top pick is the Carepod Humidifier.
- Tip: Keep a humidifier running while you sleep to stop your phlegm from thickening overnight. Just make sure to clean it regularly—nobody wants to deal with mold or bacteria making things worse.
Preventing Future Episodes of Brown Phlegm
If you’ve dealt with coughing up brown phlegm, you probably want to avoid it happening again. The good news is, there are some steps you can take to lower your chances of seeing brown-colored phlegm in the future. Let’s go over a few ways to protect your lungs and keep that phlegm at bay.
Quitting Smoking
One of the most important things you can do to prevent brown phlegm from coming back is to quit smoking. Smoking irritates your lungs, filling them with tar and toxins that cause inflammation and excess mucus production. Over time, this leads to the buildup of brown phlegm that can be hard to clear out. Quitting smoking helps your lungs heal, reduces the amount of mucus they produce, and lowers your risk of coughing up brown phlegm.
When you quit smoking, your lungs begin to clear out the tar and toxins that have built up over the years, which might lead to coughing up brown mucus for a short period. But don’t worry—it’s a sign your body is starting to recover. Stick with it, and you’ll breathe easier in the long run.
Avoid Pollution and Chemicals
Your lungs are sensitive, and the air you breathe makes a big difference. If you’re around dust, smoke, or strong chemicals, your body reacts by making more mucus to trap the junk and push it out. That’s how brown phlegm can start to show up. Try to limit your exposure when you can. Use an air purifier at home, wear a mask in dirty environments, and keep windows closed on high-smog days. A few small changes can help your lungs stay clearer and more comfortable.
- Tip: Consider using a high quality air purifier in your home to filter out allergens, dust, and other particles that could irritate your lungs. On days when air quality is poor, try to stay indoors, or if you have to be outside, wear an N-95 mask that’s designed to block out pollutants. It’s a simple step, but it can make a big difference for your respiratory health.
Managing Chronic Lung Conditions
If you live with something like COPD or another chronic lung issue, brown phlegm might be something you’ve seen before. These conditions cause inflammation and make your lungs work harder than they should. The key is staying consistent with your treatment. Use your inhalers, keep up with nebulizer treatments, and don’t skip your checkups. The more you stay on top of it, the less likely you are to deal with thick, discolored mucus getting in the way of your breathing.
- Tip: Stick to the medications prescribed by your doctor, such as inhalers, nebulizers, or other treatments. To make nebulizer treatments more quick and convenient, check out the TruNeb™ Portable Nebulizer.
Brown Phlegm: Listen to Your Body!
Brown phlegm is your body’s way of flagging that something might not be right. It could be leftover irritation from smoking, a sign of infection, or just your lungs reacting to the air around you. Whatever the cause, it’s worth paying attention to.
Taking small steps—like staying hydrated, keeping your air clean, or following your treatment plan—can make a real difference. If something feels off or the symptoms aren’t going away, trust your gut and reach out to a doctor. You know your body better than anyone. Keep listening to it.
*Article reviewed by a licensed Registered Respiratory Therapist
**Last updated 8/2/2025