On this page
This guide focuses on non–cystic fibrosis bronchiectasis in adults. If you’ve been diagnosed, your plan will blend bronchiectasis medication, airway clearance, nebulizer therapy, and daily habits to help prevent flare-ups.
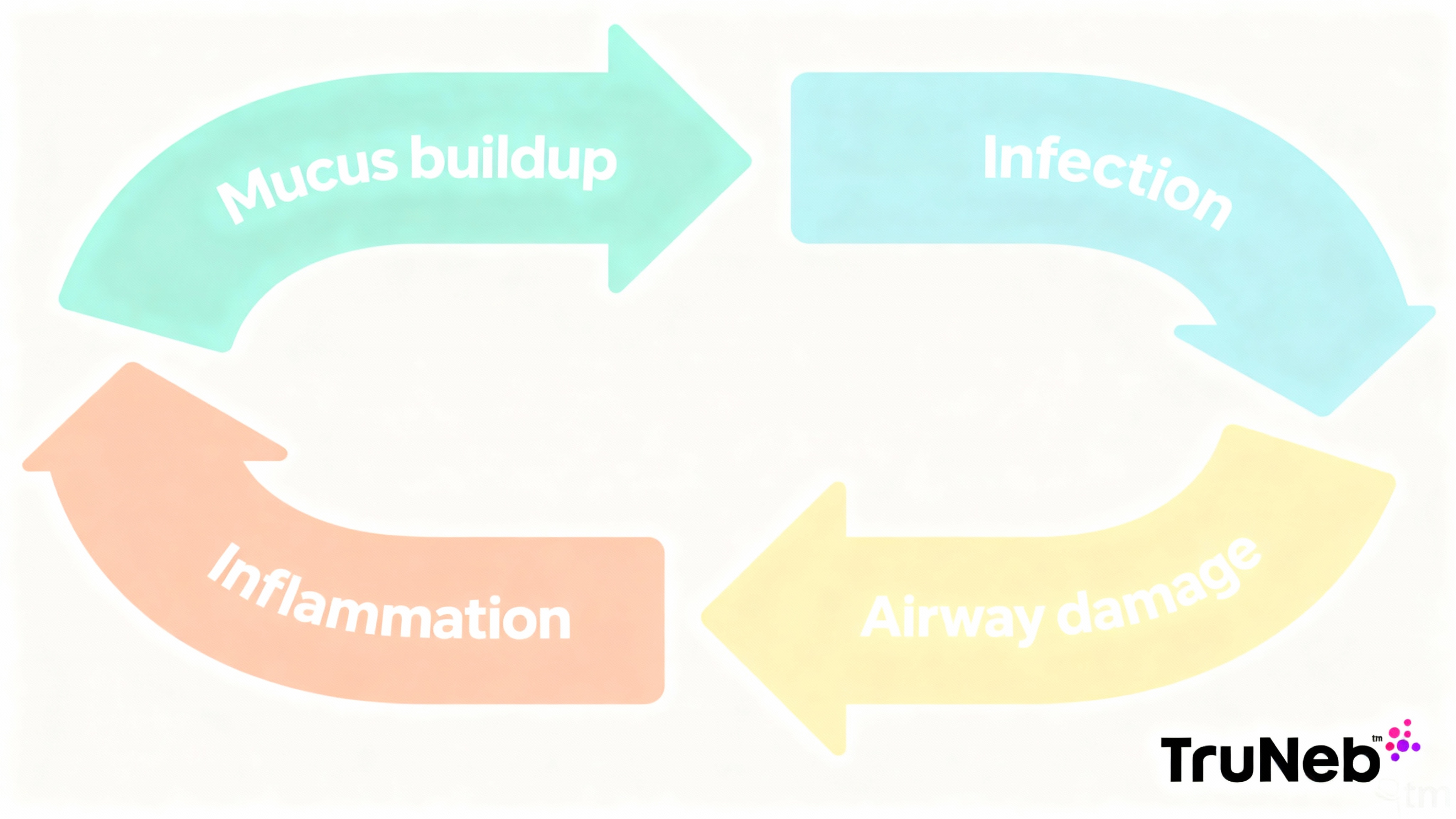
Treatment Goals: Break the Mucus–Infection Cycle
Bronchiectasis creates a loop: thick mucus sits in widened airways, germs grow, and inflammation makes even more mucus. Your care plan aims to break that loop.
- Fight and prevent infections with the right antibiotics and vaccines.
- Remove mucus every day using airway clearance and, sometimes, a nebulizer.
- Calm airway inflammation and protect lung tissue with targeted therapies and healthy habits.
Bottom line: small daily steps add up. A steady routine usually means fewer flare-ups and easier breathing.
Antibiotic Therapy: Treat Infections and Prevent Flare-Ups
Antibiotics for Flare-Ups
A flare-up (exacerbation) usually looks like more cough, thicker yellow or green sputum, fever, or breathlessness. Doctors usually treat bacterial flares with oral antibiotics for about 10–14 days. If your sputum culture shows a bug like Pseudomonas aeruginosa, your doctor might choose a specific antibiotic or use IV antibiotics if the infection is severe. Getting help early can shorten the illness and protect your lungs.
Your bronchiectasis medication plan depends on your sputum culture and symptoms.
Key tip: finishing the full antibiotic course helps prevent resistance and relapse.
Long-Term Macrolides to Prevent Flares
If you have frequent exacerbations, your doctor might suggest low-dose macrolide therapy (usually azithromycin a few times per week). This can reduce flare frequency and also calm airway inflammation. Before starting, most clinicians check your sputum for nontuberculous mycobacteria (NTM). Ongoing monitoring (like hearing, liver tests, and sometimes an ECG) helps keep this plan safe.
Inhaled Antibiotics for Chronic Infection
For people with chronic airway infection (especially Pseudomonas), inhaled antibiotics like tobramycin or colistin can be given in cycles via a nebulizer. They target bacteria directly in the lungs and can reduce flares. Some people notice chest tightness after doses; your doctor might recommend a bronchodilator first to reduce that. Your doctor will guide you on whether this is right for you.
One-liner: early, targeted antibiotics can help you recover faster and can prevent future lung damage.
Airway Clearance: Get Mucus Moving
Chest Physiotherapy and Huff Coughs
Chest physiotherapy (CPT) uses body positions and gentle clapping (percussion) to loosen mucus so you can cough it out. Huff coughing helps: take a deep breath in, then breathe out saying “huff” (like fogging a mirror). People commonly do CPT once or twice daily—morning and evening—and more often during flares.
Devices That Help
- Oscillating PEP devices (like Flutter or Acapella) create vibrations and back-pressure as you exhale, which helps shake mucus loose.
- High-frequency chest wall oscillation vests gently “shake” the chest to free mucus, useful if manual CPT is hard to do.
Daily Routine Tips
- Pick set times and pair with a daily habit (like morning news).
- Stay well hydrated to keep mucus thinner.
- Do clearance before meals or wait an hour after.
Airway clearance removes mucus from your lungs and is a daily cornerstone of bronchiectasis care.
Nebulizer Therapy: Thinning Mucus with Hypertonic Saline
What Hypertonic Saline Does
Hypertonic saline (commonly 7% or 3%) is a sterile saltwater mist you inhale. Hypertonic saline for bronchiectasis draws water into the airways, thins mucus, and triggers a productive cough so you can clear more. Studies suggest it helps mucus clearance and can improve symptoms, even if lung function numbers do not change much. In the U.S., hypertonic saline is typically prescribed and comes in ready-to-use vials.
How to Use a Nebulizer Safely
- Wash hands and sit upright. Add the prescribed saline to the cup.
- If advised, use a bronchodilator 10–15 minutes before to reduce tightness.
- Breathe the mist slowly through your mouth until the cup is empty.
- Do airway clearance right after to move out loosened mucus.
- Clean and dry the neb parts after each use to prevent germs.
Follow your device’s instructions, and your doctor’s guidance.
⚠️ You might see products labeled “steam inhaler” — these are NOT for breathing prescription medications.
Portable Mesh Nebulizers Help You Stay on Track
Portable mesh nebulizers are small, quiet, and battery-powered, so treatments are easier to fit into daily life. Using a nebulizer for bronchiectasis can make it easier to complete treatments consistently. A device like the TruNeb™ portable mesh nebulizer can deliver hypertonic saline or other inhaled medications efficiently at home or on the go, which can help you stick with your routine.
One-liner: neb saline first, then clearance—it’s a powerful combo for mucus management.
Safety note: if saline causes chest tightness or strong coughing, pause and talk to your doctor about bronchodilator pre-treatment or using a lower concentration.
In some regions, other mucus thinners like dry powder mannitol or oral agents (for example, carbocisteine or N‑acetylcysteine) are used. Ask your doctor what’s appropriate for you.
Inhalers: When Bronchodilators or Steroids Are Used
- Bronchodilators (like albuterol) can ease wheeze or chest tightness and are commonly used before exercise or saline treatments.
- Long-acting bronchodilators can be added if you also have COPD or fixed airflow limits.
- Inhaled steroids are not routinely recommended for bronchiectasis alone. They are usually reserved if you also have asthma, allergic disease, or COPD, based on your doctor’s advice.
Bottom line: inhalers support certain symptoms but are not core therapy for everyone with bronchiectasis.
Reducing Inflammation and Treating Underlying Causes
- Macrolides (like azithromycin) can lower flare-ups and also calm airway inflammation when used long-term in frequent exacerbators. Doctors usually check for NTM first and monitor for side effects over time.
- Root causes matter:
- Immune deficiencies can be treated with immunoglobulin replacement.
- ABPA (a fungal-related allergy) can require oral steroids and antifungals.
- NTM infections require multi-drug regimens guided by specialists.
- Emerging therapies: Research drugs like brensocatib (a DPP-1 inhibitor) aim to dial down harmful inflammation and, in trials, have been linked to longer time between flares.
Key idea: address infection, mucus, and inflammation together for best results.
Daily Habits That Help
- Vaccines: Stay current on flu and pneumococcal shots (and COVID-19 as advised). Fewer infections mean fewer flares.
- No smoking: Smoke and secondhand smoke slow your airway cilia and worsen mucus. Keep indoor air clean.
- Hydration and nutrition: Drink water through the day. Eat balanced meals to support strength and healing. There’s no proven “mucus” diet; focus on overall healthy eating.
- Exercise or pulmonary rehab: Gentle, regular movement helps mobilize mucus and builds stamina.
- Rest and support: Good sleep, stress management, and support groups can make daily care easier.
One-liner: healthy routines boost the impact of your medical treatments.
When to Call the Doctor
⚠️ If you cough up a lot of blood, have severe shortness of breath, or chest pain with high fever, seek emergency care immediately.
- Signs of a flare: more cough, thicker or green/yellow mucus, fever/chills, worse breathlessness, or chest pain.
- Act early: contact your doctor and ask about a sputum culture to guide antibiotics.
- Urgent signs: heavy blood in sputum, high fever with severe shortness of breath, or strong chest pain—seek emergency care.
- Check-ups: routine visits can include lung function tests and periodic sputum cultures. If you’re on long-term meds, you might need monitoring labs.
Tip: ask for a written flare plan so you know exactly what to do on day one of symptoms.
Act early when symptoms change—prompt treatment helps prevent complications.
Quick-Look: Treatment Summary
| Treatment | What it does | Examples/Notes |
|---|---|---|
| Antibiotics (flare) | Treats lung infection | Oral 10–14 days; IV if severe or resistant |
| Long-term macrolide | Lowers flares; anti-inflammatory | Azithromycin after NTM check†; monitoring needed |
| Inhaled antibiotics | Targets chronic bacteria | Tobramycin/colistin via nebulizer in cycles |
| Airway clearance | Loosens and removes mucus | CPT, huff coughs, PEP devices, chest vest |
| Nebulized saline | Thins mucus; boosts clearance | 3% or 7% saline; consider bronchodilator pre-treatment‡ |
| Bronchodilators | Eases wheeze/tightness | Albuterol before exercise or therapies if advised |
| Inhaled steroids | For coexisting asthma/COPD | Not routine for bronchiectasis alone |
† Long-term macrolides are usually considered for frequent exacerbations after checking for nontuberculous mycobacteria (NTM).
‡ A short-acting bronchodilator before hypertonic saline or inhaled antibiotics may reduce bronchospasm.
Safety reminder: Talk to your doctor before trying a new medication or changing how you use your inhaler or nebulizer. Long-term antibiotics, inhaled antibiotics, and hypertonic saline require medical guidance and monitoring.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Bronchiectasis is chronic. The goal is control: treat infections, clear mucus daily, and reduce inflammation so you have fewer flares and better breathing.
There isn’t one “best.” Most people do best with a mix: antibiotics for infections, daily airway clearance (usually with nebulized saline), plus vaccines, exercise, and no smoking.
Sometimes. Bronchodilators can ease wheeze or tightness. Inhaled steroids aren’t routine unless you also have asthma or COPD.
A nebulizer delivers medicine as a mist deep into your lungs. Hypertonic saline thins mucus, and inhaled antibiotics can target chronic bacteria.
Stick to daily clearance, take medicines exactly as prescribed, keep vaccines up to date, avoid smoke, and contact your doctor early when symptoms change.
Conclusion
Bronchiectasis care works best as a daily plan: treat infections promptly, clear mucus effectively, and calm airway inflammation, supported by healthy habits. Build a routine you can stick with, and check in with your doctor when symptoms shift so problems are handled early.
Disclaimer: This article is for informational purposes and isn’t a substitute for professional medical advice. Always talk to your doctor about your symptoms, diagnosis, and treatments.







