On this page

Best Sleeping Positions for Shortness of Breath at Night
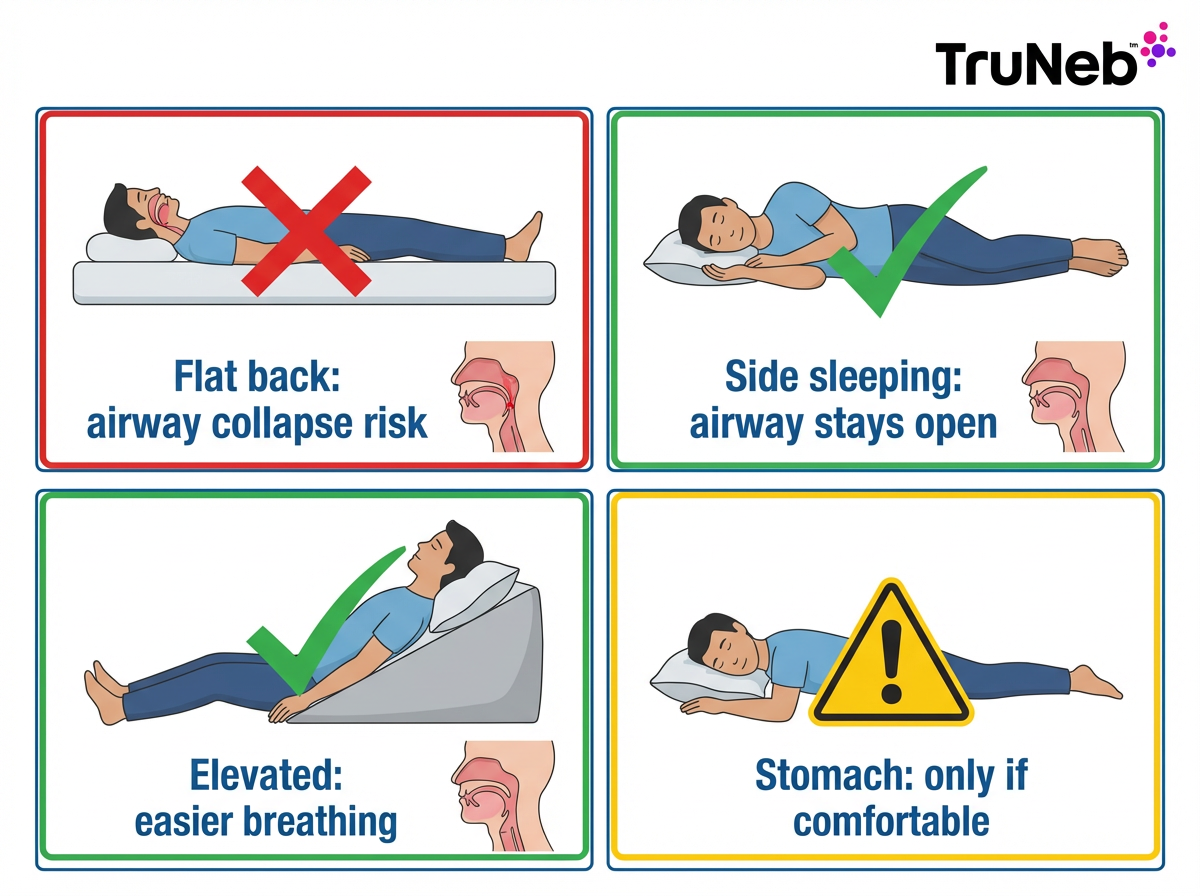
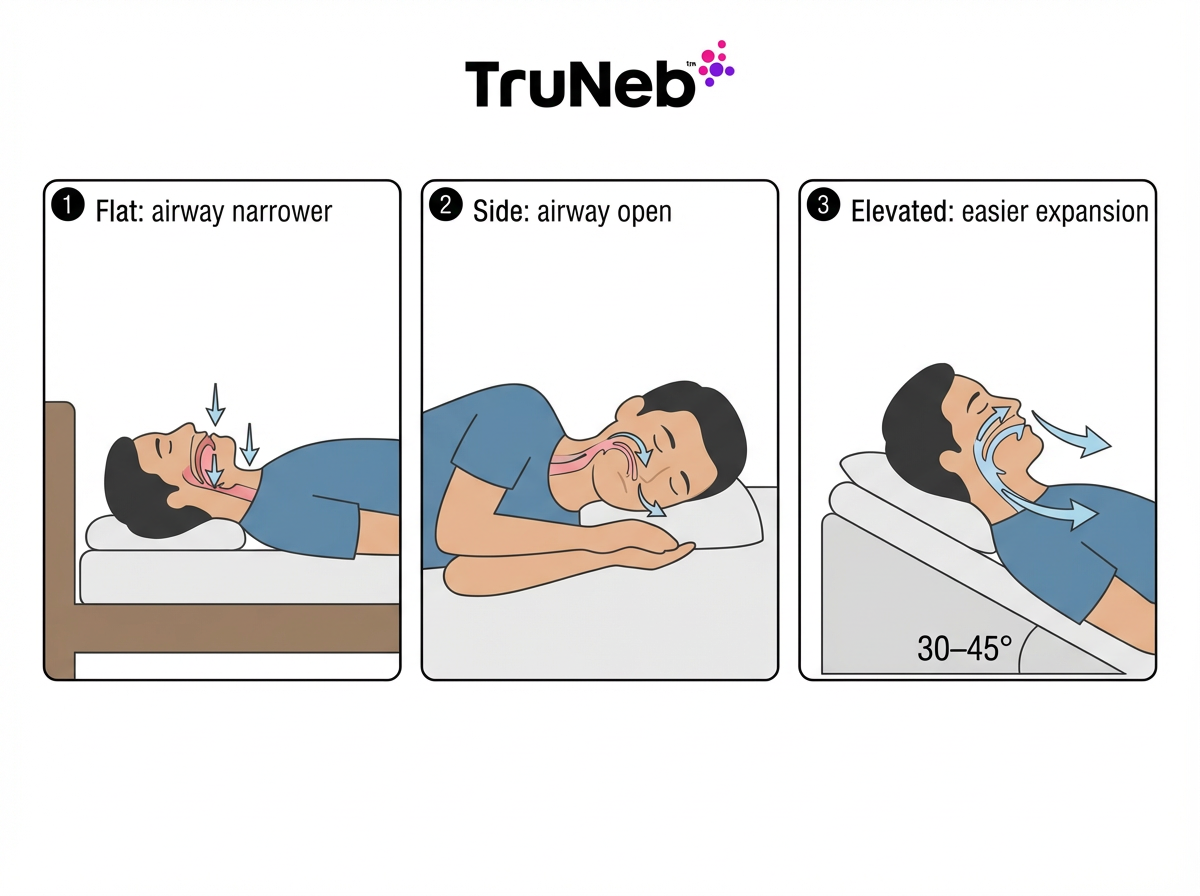
Here’s the short answer: sleep on your side or with your upper body raised. These positions keep your airway open, help your lungs expand, and can ease that tight, breathless feeling. If you get shortness of breath when lying down at night, these positions can make breathing easier.
Side sleeping
- Lying on your side helps keep your tongue and soft tissue from falling back into your throat. Breathing stays smoother and quieter.
- The left side usually feels best if you have acid reflux, which can trigger cough or asthma at night. A pillow between your knees helps your back stay aligned so you can hold the position longer.
- Some people with sleep apnea feel better on the right side, based on how their airway behaves. If the left side isn’t comfortable, choose the side you can maintain.
Elevate your head and chest
- Raise your upper body 30–45 degrees with a wedge pillow, an adjustable bed, or a recliner. Gravity helps keep pressure and fluid off your lungs and eases post-nasal drip and sinus congestion.
- No wedge? Use a firm pillow or two under your upper back and head. Keep your neck neutral (not bent forward).
Try stomach-down only if it feels good
- Stomach sleeping can reduce airway collapse for some, but it’s not for everyone. If you try it, use a thin pillow (or none) under your head and a small pillow under your hips to protect your low back. This isn’t usually the first recommendation, so only use it if it’s comfortable and helps you breathe.
Avoid lying flat on your back
- Flat-back sleeping usually makes breathing worse. Your tongue can fall backward, and chest weight or fluid can press on your lungs. If you feel breathless flat, switch to your side or prop yourself up.
Side or elevated positions usually open your airway; lying flat can make breathing harder.Compare sleeping positions for breathing comfort
| Position | Breathing comfort | Helps with | Caution |
|---|---|---|---|
| Side (left/right) | Usually best | Snoring/OSA, reflux (left side), airway openness | Use a pillow between knees; switch sides if a shoulder hurts |
| Elevated (30–45°) | Usually better | Post-nasal drip, sinus congestion, fluid-related pressure | Keep neck neutral; use a wedge or adjustable bed |
| Stomach (prone) | Mixed | Can reduce airway collapse in some people | Not a first choice; thin pillow for head, small pillow under hips |
| Back (flat) | Typically worst | — | Airway narrows; reflux and snoring can get worse |
Key takeaway: If you get shortness of breath when lying down at night, side-sleeping or raising your upper body usually helps; lying flat tends to make it worse.
Position Strategies by Underlying Condition
The best position can change based on what’s driving your shortness of breath. Match your setup to your situation.
Asthma or COPD
- What helps: Side sleeping, especially on the left side, plus a slight upright angle. Asthma can flare at night (nocturnal asthma), and COPD symptoms usually feel worse when you lie flat. COPD breathing at night can feel worse when you’re flat. A wedge pillow reduces strain on the lungs.
- Night routine: Take your prescribed inhalers or nebulizer sessions as directed by your doctor so your airways are open when you lie down. A quiet portable mesh nebulizer like the TruNeb™ portable mesh nebulizer can deliver medication or doctor-recommended saline quietly, as prescribed by your doctor. In some cases, hypertonic saline 3% (or 7% if prescribed by your doctor) thins mucus earlier in the evening so it doesn’t build up once you lie down. Cut allergens in bed (wash bedding hot, dust-mite covers, keep pets out).
- Safety note: Talk to your doctor before trying a new medication or nebulized saline.
Heart failure or cardiac issues
- What helps: Sleeping propped up quite a bit. A lot of people with congestive heart failure need 2–3 pillows, a foam wedge, or even a recliner to breathe comfortably. Avoid being flat. If you wake up gasping (paroxysmal nocturnal dyspnea), call your cardiologist and seek urgent care if you still can’t catch your breath after sitting up. Needing several pillows to breathe comfortably is called orthopnea.
- Side choice: Pick the side that feels best; comfort matters more than left vs right when the main issue is fluid in the lungs. Long term, consider raising the head of your bed on blocks or using an adjustable base.
Obesity or deconditioning
- What helps: Side sleeping plus a small incline. Extra body weight on the chest and belly can press on the lungs when flat. A 30° incline frees your diaphragm. Use pillows between the knees and under the top arm for support. A lot of people with obesity also have sleep apnea, so avoid back-sleeping. If you’re deconditioned after illness, lying flat can make breathing harder; the same small incline helps.
Anxiety or panic
- What helps: A slightly reclined position (propped up in bed) can calm the “air hunger” sensation. Practice pursed-lip breathing and slow belly breaths as you settle in. A simple wind-down (quiet music, gentle stretching) tells your body it’s safe to relax. If your doctor has ruled out heart and lung problems, anxiety can still make breathing feel harder at night.
Key takeaway: For nighttime shortness of breath, keep your airway open with side-lying or head elevation, then add tweaks based on your specific condition.
Other Tips to Help You Breathe Easier at Night
Position is step one. These simple habits can make nights even smoother.
- Clear your airways before bed
- You can use a saline nasal spray or a nasal strip if congestion is common, and ask your doctor if these are right for you. If your lungs make mucus, follow your doctor’s plan for airway clearance or prescribed inhaler/nebulizer sessions. For some people, doing them in the late afternoon or evening helps them feel clearer at bedtime.
- Optimize your bedroom
- Keep the room cool but not cold. Dry air can trigger cough, and a clean humidifier can help. Lower allergens with dust-mite covers and regular hot-water washes for bedding. A gentle head-of-bed incline also helps sinus drainage.
- Mind meals and alcohol
- Avoid large meals 2–3 hours before bed. Big meals and alcohol can worsen reflux and relax throat muscles, which can make breathing tougher. If you take water pills (diuretics), ask your doctor if timing them earlier could reduce nighttime trips and fluid shifts.
- Calm your breathing
- Spend 10–15 minutes on slow, relaxed breaths. Try pursed-lip breathing: inhale through your nose, exhale slowly through puckered lips. Some people sleep better with a fan on for airflow and white noise.
- Use devices if prescribed
- If your doctor prescribed CPAP for sleep apnea, try to use it every night. If your doctor prescribed oxygen therapy, use it as directed. Arrange pillows around tubing for comfort.
Note: Talk to your doctor before changing medications or adding new treatments.
Key takeaway: Pair a side or elevated position with a calm routine, light evening meals, and prescribed devices for easier breathing.

When to See a Doctor and When It’s an Emergency
⚠️ Call 911 or go to emergency care now if:
- You have severe trouble breathing that doesn’t improve when you sit up or use your inhaler/oxygen.
- Shortness of breath comes with chest pain or pressure, confusion, fainting, or a bluish color to lips or fingers.
Make a prompt doctor’s appointment if:
- Your shortness of breath when lying down at night is new or getting worse, or you need more pillows (or a recliner) to sleep.
- You suspect sleep apnea (loud snoring, witnessed pauses, daytime sleepiness).
Mention at your next check-up if:
- Position changes help only a little, or you’re using your rescue meds more at night. Tell your doctor exactly how many pillows you need to sleep; in heart failure, orthopnea (breathlessness when flat) is an important warning sign.
Key takeaway: Emergency symptoms need immediate care; new or worsening shortness of breath at night should be evaluated by a doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before changing any medications, treatments, or devices.
Frequently Asked Questions
Tap or click a question below to see the answer:
Side sleeping or a slight incline works best for most people. These positions keep your airway open and help your lungs expand. Try a wedge pillow or an adjustable bed, and avoid lying flat on your back.
Gravity isn’t helping your lungs when you’re flat. Soft tissues can fall back and narrow your airway, and pressure or fluid in your chest can increase. That’s why you may feel breathless when flat (orthopnea).
It usually is. Back-sleeping raises the risk of airway blockage and can worsen snoring or apnea. Side-sleeping or sleeping propped up usually feels better if you’re short of breath.
Start around a 30° incline. A wedge pillow makes this easy. Your head and chest should be above your abdomen. Adjust until you find the lowest angle that eases your breathing.
Yes, for a lot of people. A clean humidifier can ease dryness and cough. A fan improves air movement and can lower anxiety, though it doesn’t add oxygen. Keep humidifiers clean to prevent mold.
If position changes don’t help, or symptoms are new or getting worse, make an appointment. Get urgent help if you have severe breathlessness that doesn’t improve when you sit up, chest pain, or bluish lips.
Key takeaway: Most people breathe best on their side or slightly upright; avoid lying flat and see a doctor for severe or worsening symptoms.