On this page
Best Place to Live with COPD: What Matters Most
COPD (Chronic Obstructive Pulmonary Disease) makes breathing harder. The air around you can make that better or worse. Clean air and steady, mild weather can ease day-to-day symptoms. Polluted air and weather extremes can trigger coughing, wheezing, and flare-ups.
Here’s the simple truth:
- Air quality matters. Fine particles and ozone irritate lungs and can raise your risk of exacerbations.
- Weather matters. Big swings in heat, cold, or humidity can make breathing feel harder.
- Altitude matters. Thin air at higher elevations gives you less oxygen per breath.
If you’re thinking about the best place to live with COPD, start by weighing these environmental pieces first. They shape how your lungs will feel every day.
Key takeaway: Clean air and mild weather help; pollution and extremes raise flare-up risk.
Key Factors in a COPD-Friendly Environment
Use these to compare places or plan your day:
Air Quality and Pollution
Smog, wildfire smoke, and fine particles (PM2.5) irritate lungs. Cities on the American Lung Association’s clean‑air lists are usually easier on breathing. Check the Air Quality Index (AQI) for your city; “Good” days are best, and frequent “Unhealthy” days make a place tougher for COPD.
Temperature and Humidity
Mild is best. Extreme heat or deep cold can tighten airways. Very humid air can feel heavy; very dry air can dry out airways. A middle range (about 40–60% humidity) is usually most comfortable.
Altitude and Oxygen
Higher elevations have thinner air, which means less oxygen per breath. Some people do fine; others feel worse. Test your tolerance before moving. Your doctor might adjust oxygen settings or parts of your plan if you’ll spend time at higher elevation.
Allergens and Irritants
Pollen, mold, dust, and smoke can set off symptoms. Check local pollen seasons and wildfire risk.
Access to Healthcare and Support
Being near pulmonologists, pulmonary rehab, and smoke‑free policies makes day‑to‑day life easier. Quick access to urgent or emergency care also matters when symptoms suddenly worsen.
Key takeaway: Your COPD‑friendly place balances clean air, mild temps, moderate humidity, tolerable elevation, low allergens, and good access to care.
Best Places and Climates for COPD
There isn’t one perfect city for everyone, but patterns are clear. Western states and some coastal or northern spots tend to rank well for lung health because of cleaner air and healthier habits.
Good places to explore:
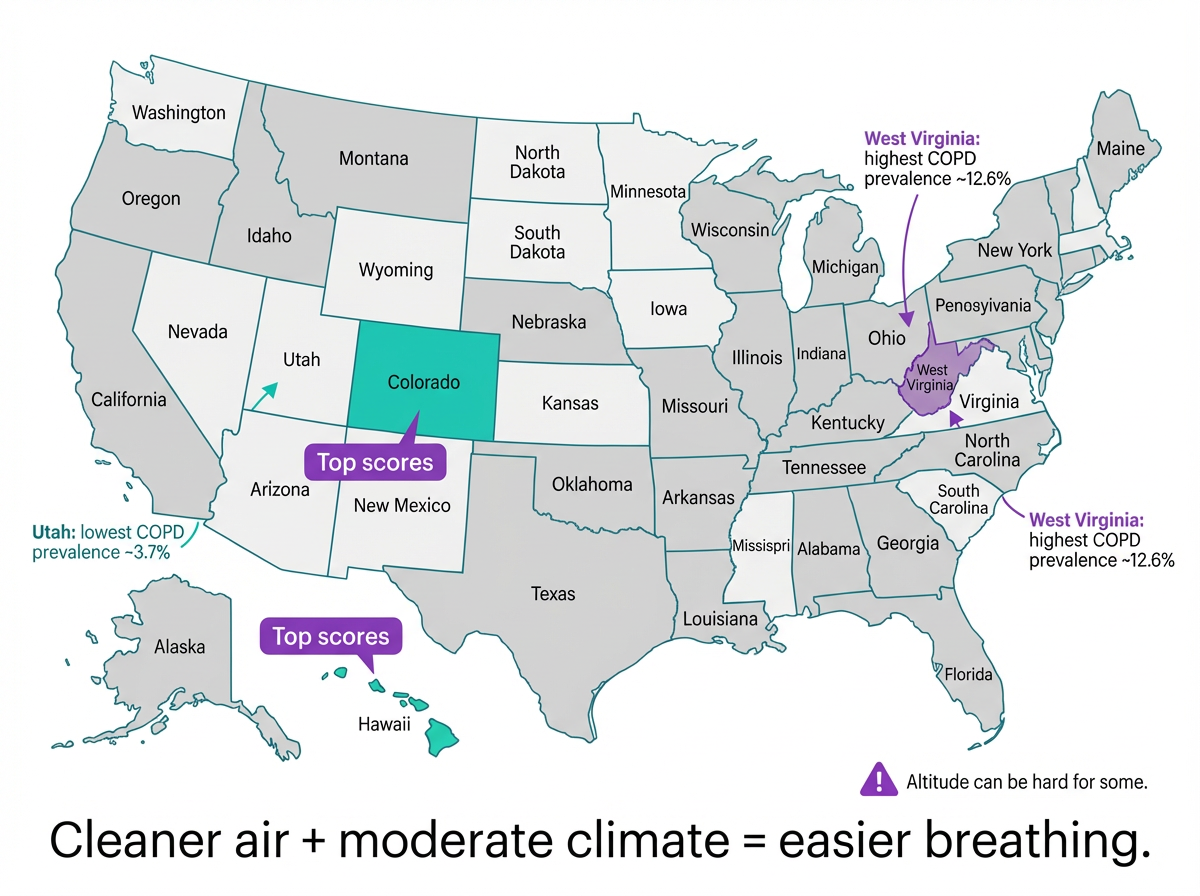
- Colorado and Hawaii: Both score high for lung health. Clean air and strong public‑health measures help. Note Colorado’s altitude can be hard for some.
- New Mexico and Utah: Dry air and lower smoking rates help. Utah also has the nation’s lowest COPD prevalence (~3.7%). Test altitude tolerance.
- Clean‑air cities: Places like Asheville, NC, and Bangor, ME, show up on clean‑air lists and can feel easier for daily breathing.
Use these as a starting list, then dig into neighborhood‑level air and weather to find your best personal fit.
Key takeaway: Western, drier states with cleaner air usually feel easier for COPD. Just weigh how you handle altitude.
Places and Conditions That Can Worsen COPD
Some environments commonly aggravate COPD. Watch for:
- Heavy pollution: Frequent smog or smoke irritates lungs. Parts of California’s Central Valley (like Bakersfield) regularly rank among the most polluted.
- Hot, humid summers: Gulf Coast heat plus high humidity and ozone can make air feel heavy and breathing labored.
- Frigid winters: Very cold, dry air can tighten airways and trigger bronchospasm.
- Very high elevation: Thin air above ~5,000–8,000 feet can be too hard for some with moderate to severe COPD.
- Regions with high COPD burden: Parts of Appalachia face higher COPD rates linked to smoking and care gaps.
If you live in a tougher climate, you still have options. Optimize your indoor air, plan outdoor time, and keep your treatment plan ready.
Key takeaway: High pollution, high humidity or deep cold, and very high altitude can make COPD symptoms worse.
How to Evaluate a COPD‑Friendly Location (Checklist)
Use this quick checklist to size up any city:
1) Check air quality: Look up annual particle pollution and high‑ozone days in ALA reports. Also check the Air Quality Index (AQI) for your city with an air‑quality app. More “Good” days and fewer “Unhealthy” days are better.
2) Review climate norms: Average humidity and temperatures. Aim for mild seasons and moderate humidity.
3) Note elevation: Above ~4,000–5,000 feet? Plan a test visit and talk with your doctor about oxygen needs.
4) Scan allergens and risks: Pollen seasons, wildfire smoke, or dust events.
5) Map healthcare access: Nearby pulmonologists, hospitals, and pulmonary rehab, plus reasonable distance to an ER for sudden severe flares.
6) Consider local policies: Smoke‑free laws and lower smoking rates make daily life easier.
Aim for more “Good” AQI days; frequent “Unhealthy” days make a location tougher for COPD.
| AQI category | Range | What it means for COPD | Planning tip |
|---|---|---|---|
| Good | 0–50 | Air is clean and easiest on breathing. | Normal outdoor activities. |
| Moderate | 51–100 | Generally OK; sensitive lungs might notice symptoms. | Shorten strenuous outdoor time on hazy days. |
| Unhealthy for Sensitive Groups | 101–150 | Higher risk for people with lung disease. | Plan indoor activities; use filtered air. |
| Unhealthy or worse | 151+ | Poor air quality that can trigger symptoms. | Stay indoors with filtered air and follow your action plan. |
Note: Check daily AQI in your area with an air‑quality app.
Key takeaway: Judge any city by air, climate, altitude, allergens, and care access—not just by reputation.
Living (and Breathing) Well Anywhere
You can’t always move—but you can shape your environment. These steps help a lot of people with COPD breathe easier right where they are.
Make Your Home a Safe Breathing Zone
- Keep it smoke‑free. Avoid cigarettes, wood smoke, and strong fumes.
- Filter the air. Use a HEPA purifier and change HVAC filters on time.
- Control humidity. Aim for ~50% indoors. Use a dehumidifier in muggy climates and a clean, well‑maintained humidifier if it’s very dry.
- Reduce irritants. Go unscented with cleaners and avoid paraffin candles.
- Know the difference: steam inhalers aren’t nebulizers. Only put COPD medications or saline into a nebulizer designed for them.
Plan Your Day by the Forecast
- On high‑pollution or high‑pollen days, try to stay indoors in a climate‑controlled space with filtered air.
- In heat, it’s easier on your lungs to go out earlier or later in the day. In winter, cover your nose and mouth to warm the air.
Stay Active and Be Prepared
- Gentle activity helps you feel and function better. Walk indoors on bad‑air days; enjoy parks on good days.
- A portable mesh nebulizer like the TruNeb™ Portable Mesh Nebulizer can make on‑the‑go treatments simpler and quieter. Use it only with medications or sterile saline your doctor has approved, and follow the plan you’ve set together.
Clear Mucus and Follow Your Plan
- Hydrate, practice controlled coughing, and use airway‑clearance tools if your care team recommends them.
- Some people use nebulized hypertonic saline (3% or 7%) to thin mucus. Use only sterile, pre‑mixed saline made for nebulizers - don’t mix your own or use other liquids unless your doctor tells you to. Ask your doctor if it fits your plan.
- Ask your doctor about staying up to date on flu, pneumonia, and COVID vaccines to help prevent infection‑triggered flare‑ups.
⚠️ If you notice severe or suddenly worsening shortness of breath, chest pain, confusion, or blue lips or fingers, call 911 or seek emergency medical care right away.
Safety note: Talk to your doctor before trying a new medication or changing your treatment.
Key takeaway: Optimize your home air, plan around the forecast, and use the right tools to stay active and in control.
FAQs: COPD and Climate
Tap or click a question below to see the answer:
Usually. A lot of people with COPD breathe easier in moderate, drier air. High humidity (above ~60%) can feel heavy and can worsen shortness of breath. Aim for a mid‑range around 40–60%.
It can. Cold, dry air can irritate and tighten airways. Warm the air with a scarf or mask, stay active indoors, and keep rescue meds handy.
It can be challenging. Thin air at higher elevations delivers less oxygen per breath. If you already use oxygen, ask your doctor about setting changes before trips above ~5,000 feet.
Western states tend to lead. Colorado and Hawaii rank among the best for lung health, with New Mexico and Utah close behind. Utah has very low COPD prevalence.
Areas with heavy pollution, very humid hot summers, or extreme cold are harder on lungs. Some Central Valley metros are highly polluted, and parts of Appalachia have a high COPD burden.
Yes. Improve indoor air (no smoke, use HEPA filters), plan your day by air quality, stay active, and follow your treatment plan. Portable tools and airway‑clearance steps can help on flare‑prone days.
Key takeaway: Dry, clean, and mild beats humid, polluted, or extreme—and smart habits help you breathe better anywhere.
Conclusion & Next Steps
There’s no single perfect city for COPD. Your best place is the one with clean air, comfortable weather, good care nearby, and a routine you can keep. Use the checklist, test the fit, and shape your home air so every day feels a little easier.
Even if you stay where you are, you can still improve the air around you and how you navigate your climate. A portable mesh nebulizer can make treatments easier away from home, and airway‑clearance steps can make tough days more manageable.
Talk to your doctor about your plan and any new therapies you’re considering.
Key takeaway: There’s no single paradise—use data and daily habits to build your best place to breathe.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options.