On this page
Asthma vs Pneumonia: Key Differences at a Glance
Asthma is a chronic airway disease. Pneumonia is an acute lung infection. Both make breathing hard, but they're not the same. If you're wondering about the difference between asthma and pneumonia, here's the short version.
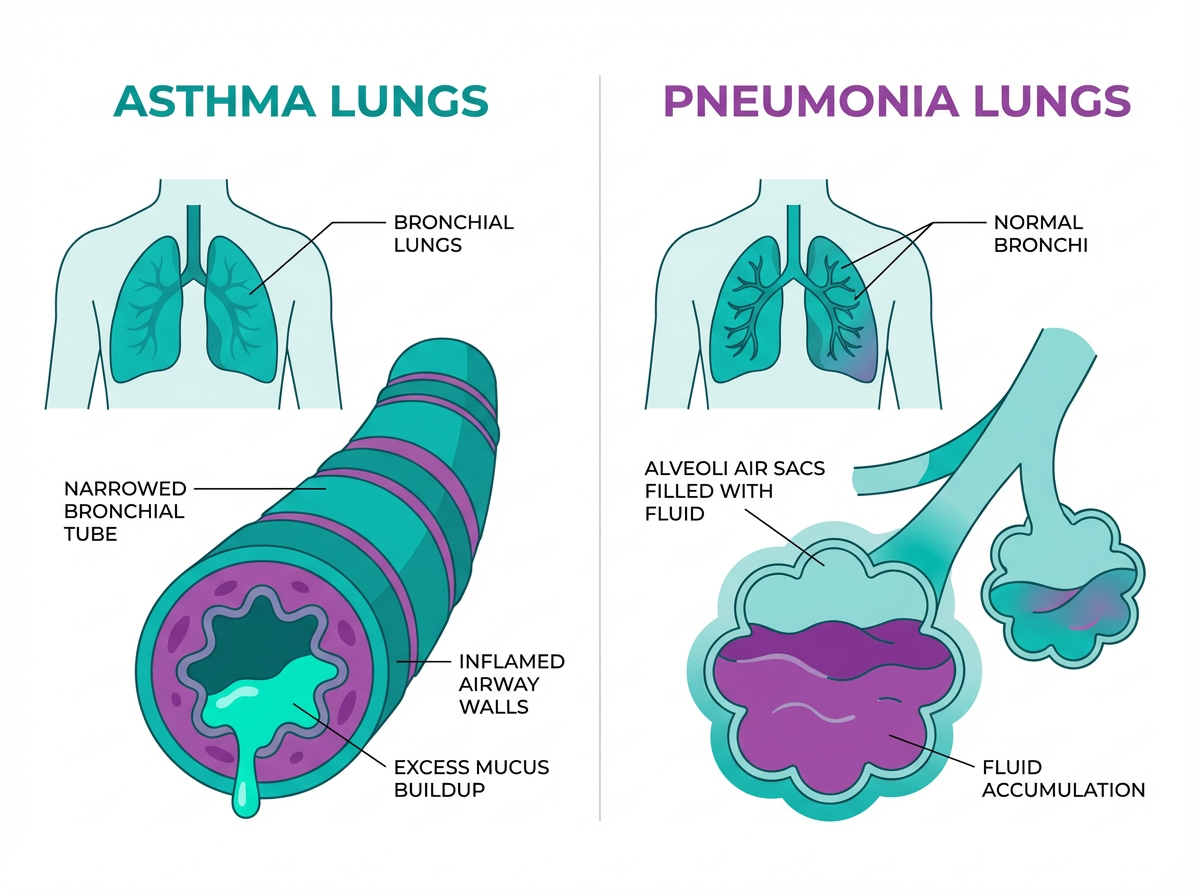
Where it happens:
- Asthma affects your bronchial tubes, the airways that carry air in and out.
- Pneumonia affects the air sacs in the lungs, called alveoli, which can fill with fluid or pus.
Quick differences:
- Timeline: Asthma is long term with flare-ups. Pneumonia is short term and usually clears with treatment.
- Cause: Asthma is not an infection. Pneumonia is caused by germs like bacteria or viruses.
- Contagious: Asthma is not contagious. Pneumonia can be.
- Clues: Asthma commonly brings wheezing and chest tightness. Pneumonia typically brings fever, chills, and a wet cough.
- Diagnosis: Asthma is confirmed with breathing tests like spirometry. Pneumonia shows up on a chest X-ray.
- Treatment: Asthma needs daily control plus quick-relief meds. Pneumonia needs antibiotics or antivirals and rest.
- Curability: Asthma is managed over time; pneumonia is usually curable with the right treatment.
Key takeaway: Asthma is a condition you manage; pneumonia is an infection you treat.
Asthma affects the airways and is managed long term; pneumonia infects the air sacs and is usually curable with the right treatment.
| What to compare | Asthma | Pneumonia |
|---|---|---|
| Type | Chronic airway condition | Acute lung infection |
| Where it happens | Bronchial tubes (airways) | Air sacs (alveoli) |
| Timeline | Long-term with flare-ups | Short-term illness |
| Contagious | No | Sometimes, depending on cause* |
| Hallmark signs | Wheezing, chest tightness, episodic shortness of breath | Fever, chills, wet cough, chest pain with deep breaths |
| How doctors diagnose | Lung function testing (spirometry), bronchodilator response; X-ray typically normal | Chest X-ray shows infection; blood/sputum tests and oxygen checks |
| Treatment focus | Controller medicines and quick-relief inhaler or nebulizer | Antibiotics when bacterial; antivirals for some viral cases; rest, fluids, fever control |
*Contagiousness depends on the cause; bacterial and viral pneumonia can spread.
Symptoms Comparison: How to Tell Asthma from Pneumonia
Asthma and pneumonia can both cause coughing and shortness of breath, but a few signs help you tell them apart. If you're comparing asthma vs pneumonia symptoms, use the lists below as a quick guide.
Asthma symptoms:
- Wheezing, especially on the exhale
- Chest tightness
- Shortness of breath that comes and goes
- Dry or night-time cough
- Triggers like exercise, allergies, or cold air
Pneumonia symptoms:
- Fever and chills
- Cough with yellow or green mucus (sometimes blood-tinged)
- Chest pain that worsens with deep breaths or coughing
- Constant fatigue and feeling unwell
- Fast breathing or low oxygen
Symptoms can overlap—pneumonia can sometimes cause wheezing, and asthma flares can show up during a cold. In children, high fever plus lethargy and a wet cough leans toward infection, while recurrent wheezing with triggers leans toward asthma. See a doctor promptly for any breathing trouble in a child.
A quick rule: Wheezing points more to asthma. Fever plus a wet cough points more to pneumonia. Only a doctor can diagnose for sure, so get checked if you're not sure.
Key takeaway: Wheezing leans toward asthma; fever with a wet cough leans toward pneumonia.
Causes and Risk Factors: Why Asthma Happens vs Why Pneumonia Happens
Causes of asthma:
- An overreactive immune response and family history
- Triggers like dust mites, pollen, smoke, cold air, or exercise
- Viral colds can trigger flares but don’t cause asthma itself
Causes of pneumonia:
- Infection in the lungs from bacteria, viruses, or fungi
- Common causes include Streptococcus pneumoniae and influenza
Risk factors for asthma:
- Family history of asthma or allergies
- Exposure to smoke or strong irritants
- Air pollution and certain jobs
Risk factors for pneumonia:
- Very young or older age
- Chronic conditions such as asthma or COPD
- Smoking, a weak immune system, and skipping the flu shot and pneumococcal vaccination
Asthma doesn’t turn into pneumonia. Chronic airway inflammation and some steroid treatments can make the lungs more vulnerable to infections, which is one reason asthma raises pneumonia risk.
Key takeaway: Infections cause pneumonia; asthma raises risk but doesn’t become pneumonia.
Diagnosis: How Doctors Distinguish Asthma from Pneumonia
Asthma diagnosis:
- History of repeated symptoms and triggers
- Breathing tests like spirometry show airflow that improves with a bronchodilator
- Chest X-rays are usually normal
Pneumonia diagnosis:
- Chest X-ray shows lung spots from infection
- Blood tests and sometimes sputum culture look for infection
- Oxygen level checks, especially if breathing is fast or labored
Exam clues:
- Asthma usually has widespread wheezing
- Pneumonia can have crackles or decreased breath sounds in one area
Asthma tends to cause a musical wheeze across the chest, while pneumonia can cause crackling sounds in a single area. Both can co-exist—someone with asthma who gets pneumonia can have wheezing and an abnormal X-ray.
Bottom line: If a chest X-ray is abnormal, doctors think pneumonia. If breathing tests show reversible airflow limits, doctors think asthma.
Key takeaway: X-rays point to pneumonia; lung function tests point to asthma.
Treatment and Management: Asthma vs Pneumonia
Asthma treatment:
- Daily control: inhaled corticosteroids and other controllers to calm airway inflammation
- Quick relief: short-acting bronchodilators (rescue inhaler or nebulizer) for fast breathing relief
- A portable mesh nebulizer like TruNeb™ can deliver your prescribed liquid medicine as a fine mist when inhaler technique is hard (use it as part of a doctor-recommended asthma plan, at home or on the go)
Pneumonia treatment:
- Antibiotics for bacterial pneumonia; antivirals when flu is confirmed early
- Some viral pneumonias are managed with supportive care only
- Rest, fluids, fever reducers, and oxygen if levels are low
- If wheezing or tight airways are present, doctors may add bronchodilators by inhaler or nebulizer
- In some cases, doctors use nebulized hypertonic saline (a stronger salt solution) to loosen thick mucus. It’s supportive—not a primary cure—and should only be used if your doctor recommends it.
Antibiotics treat bacterial pneumonia; they don’t treat asthma or purely viral infections.
Consumer warning: Steam inhalers aren’t the same as nebulizers and shouldn’t be used to inhale prescription medications.
Safety note: Medicines and devices work differently for each person. Talk to your doctor before trying a new medication.
Key takeaway: Asthma needs long-term control; pneumonia needs short-term infection care.
Complications and When to Seek Medical Help
In severe cases, complications can include:
- Severe asthma attacks that can lead to respiratory failure if untreated
- Pneumonia complications such as pleural effusion, sepsis, or low oxygen, especially in young children, older adults, or people with other conditions
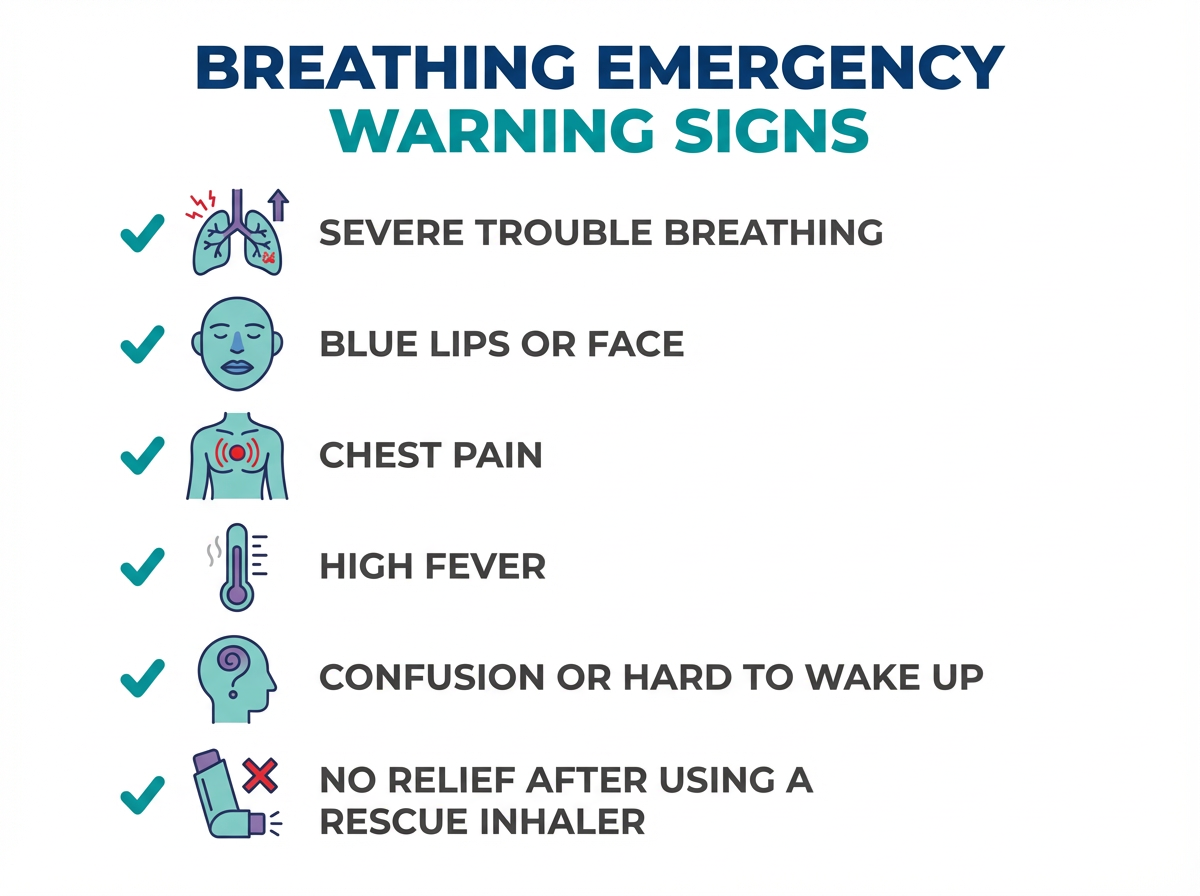
⚠️ Emergency signs – get help right away:
- Severe trouble breathing or fast breathing when you’re resting
- Lips or face turning blue
- Chest pain or pressure
- Confusion, hard to wake, or worsening weakness
- High fever that won’t come down
- For asthma: peak flow in the red zone or no relief after rescue meds
In babies, young children, and older adults, confusion, trouble waking, poor feeding (in infants), or not acting like themselves are red flags.
If you think you have pneumonia or your asthma attack isn’t improving, seek urgent care. If you’re not sure whether it’s asthma or pneumonia but your breathing feels worse than usual, get urgent medical help rather than waiting. Call 911 for severe breathing trouble.
Medical reminder: Don’t start, stop, or change prescription medicines on your own. Your care team should guide every step.
Key takeaway: Breathing trouble with fever, blue lips, or confusion is an emergency.
Prevention and Prognosis: Staying Safe from Asthma Attacks and Pneumonia
Prevent asthma flares:
- Take controller meds as prescribed and keep your rescue inhaler handy
- Avoid smoke and known triggers; use your asthma action plan
- Check in with your doctor to keep control steady
Prevent pneumonia, especially if you have asthma:
- Doctors typically recommend a yearly flu shot, especially if you have asthma
- Ask your doctor about pneumococcal vaccination; people with asthma are a higher-risk group and are often advised to get it earlier
- Wash hands, avoid close contact with sick people, and don’t smoke
Outlook:
- With good management, most people with asthma live full, active lives; asthma isn’t curable but can be well controlled
- Most pneumonia cases improve within days to weeks with the right treatment, though fatigue can linger; pneumonia is usually curable with appropriate treatment, though it can be serious
Simple plan, better breathing: Control asthma daily and lower your chance of serious lung infections.
Key takeaway: Vaccines, good asthma control, and no smoking cut pneumonia risk.
Frequently Asked Questions
Tap or click a question below to see the answer:
Look at the pattern and what tests show. Pneumonia typically includes fever and a wet cough, while asthma causes wheezing and chest tightness. Doctors confirm pneumonia with a chest X-ray and confirm asthma with lung function testing (spirometry) that improves after a bronchodilator. If symptoms are severe or you're unsure, get medical care.
No. Asthma isn’t an infection, so it can’t turn into pneumonia. People with asthma can still catch pneumonia, and the infection can make asthma symptoms worse.
Yes. Pneumonia can trigger wheezing and an asthma flare on top of the infection. Treatment addresses both—antimicrobials for the infection and bronchodilators and steroids for the asthma, as your doctor directs.
Risk depends on age, other illnesses, and how fast you start treatment. Both can be life-threatening in some situations. Get urgent care if breathing is getting worse, you have blue lips, high fever, or confusion.
They don’t cure pneumonia, but doctors may add bronchodilators (by inhaler or a nebulizer like TruNeb) if wheezing or tight airways are present. The main treatment for pneumonia is antimicrobial therapy and supportive care. Don’t start new inhaler or nebulizer treatments for pneumonia without checking with your doctor.
Asthma is chronic inflammation of the airways with wheezing and triggers—it isn’t an infection. Bronchitis is inflammation of the bronchial tubes, usually from a viral infection or smoking, and often causes a cough with mucus. Pneumonia is an infection in the lung tissue (air sacs) that generally causes fever and more serious illness.
Bottom line: Asthma is a chronic airway condition you manage; pneumonia is an infection you treat—see a doctor for any serious or new breathing trouble.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and any questions you have about asthma, pneumonia, or your medications.