On this page
Breathing isn’t something we really think about... until it gets tough. Asthma and COPD can both leave you wheezing and gasping for air, but they aren’t the same problem. The tricky part? They can look a lot alike, but they’re not the same.
Asthma tends to come and go, showing up when something sets it off. COPD, on the other hand, sticks around and gets worse over time. Knowing the difference between asthma vs COPD matters because the right diagnosis means the right treatment. Let’s review both to get the full scoop.
What Is Asthma?
Asthma is what happens when your airways overreact to certain triggers. Something harmless like pollen, pet dander, or exercise, sends the body into defense mode. The muscles lining the airways tighten, swelling kicks in, and mucus clogs things up. Asthma shows up in both kids and adults. Some people are lucky enough to outgrow it, and others have it for life.
Is Asthma Restrictive or Obstructive?
Lung diseases fall into two categories: restrictive (where the lungs can’t expand properly) and obstructive (where air gets trapped inside). Asthma is obstructive. Air goes in just fine, but when you try to breathe it out, tight airways and extra mucus slow everything down. This makes it difficult for someone with an asthma attack to properly exhale carbon dioxide.
Asthma Symptom Checklist
Asthma has a long list of triggers. Some are easy to avoid, like smoke or strong perfumes. Others, like cold air or stress, are harder to dodge.
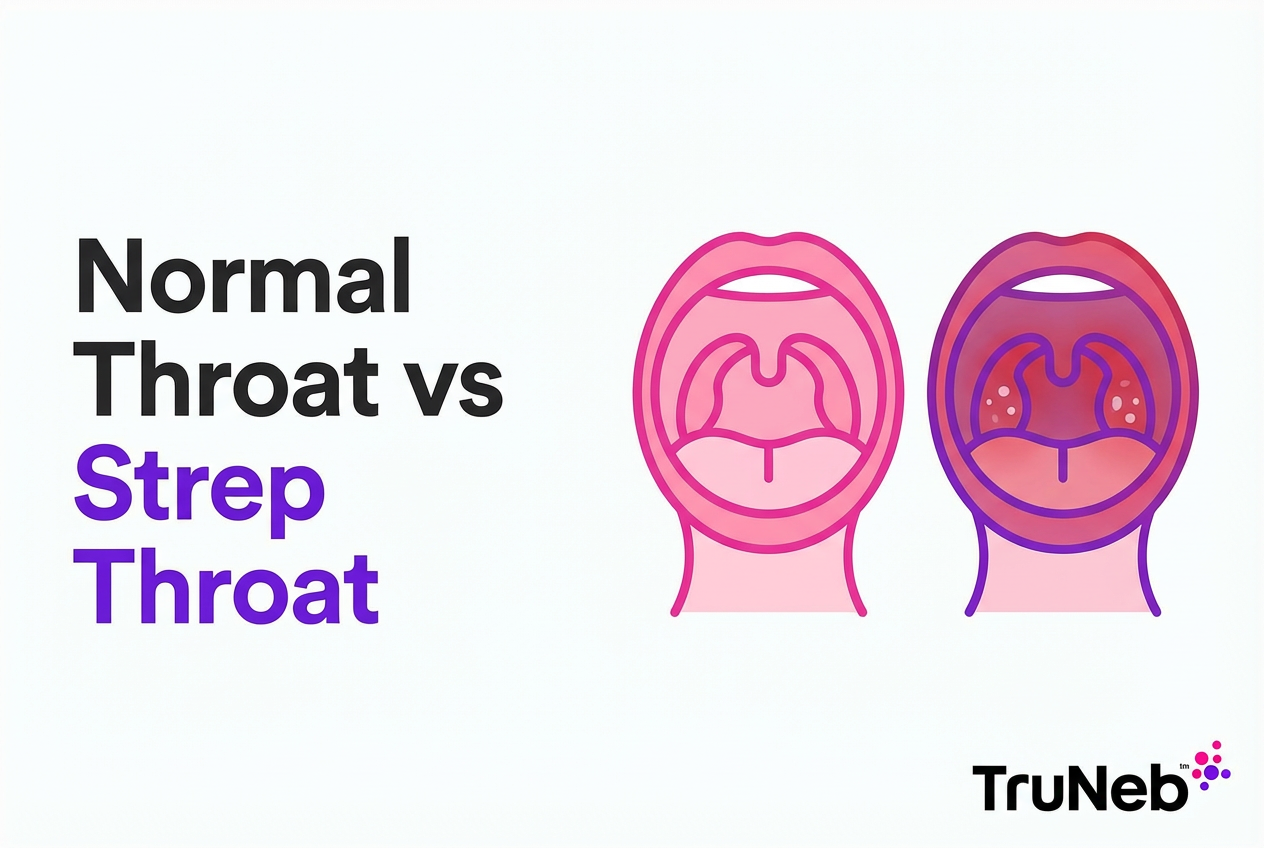
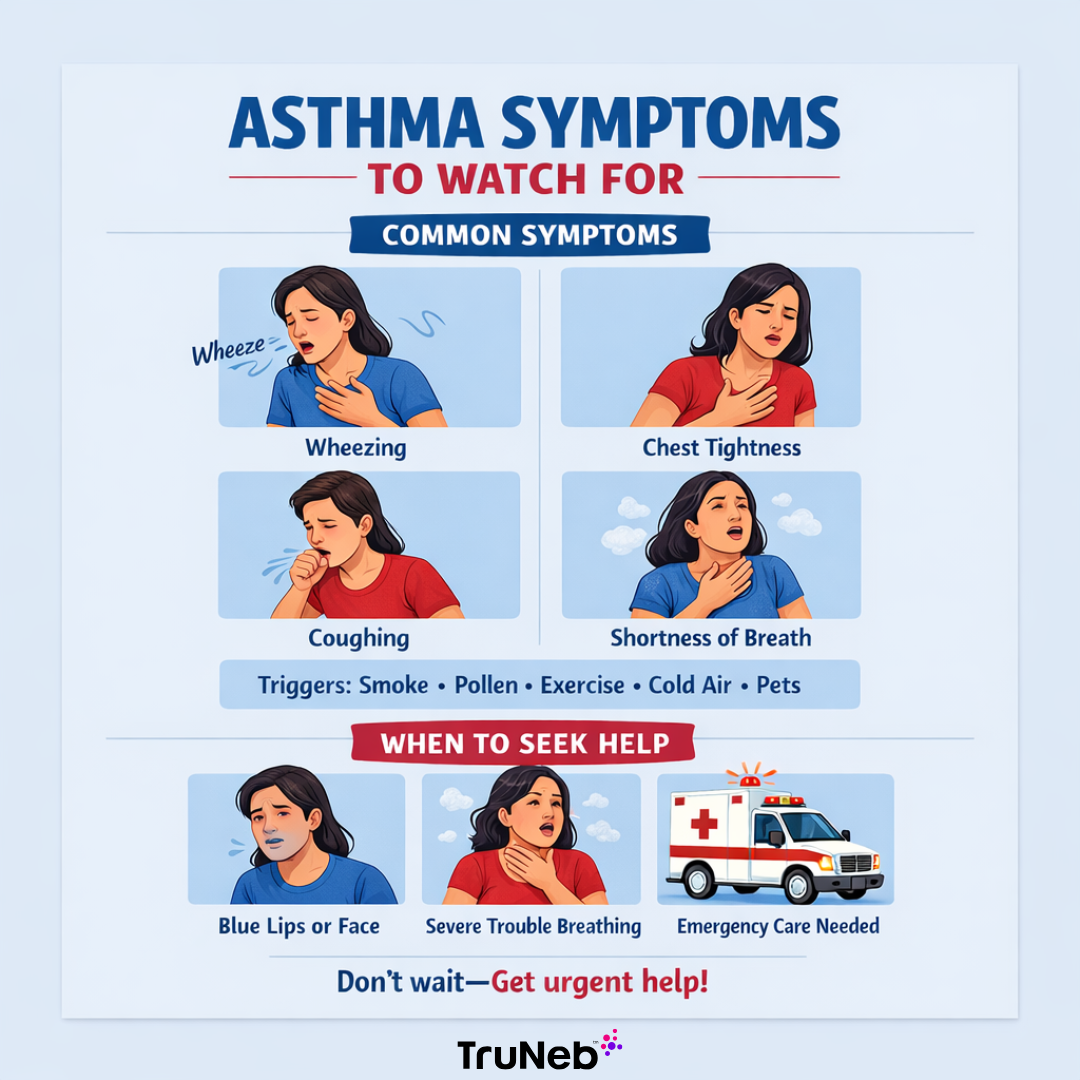
When asthma flares up, you might notice:
- Wheezing – a high-pitched whistling sound when you breathe
- Shortness of breath – feeling like you can’t get enough air
- Chest tightness – like someone is squeezing your lungs
- Coughing – especially at night or after exercise
Asthma can feel different from person to person, but these are the usual warning signs that it’s time to grab a rescue inhaler, nebulizer, or other prescribed treatment. Severe episodes can land you in the emergency room.
What Is COPD?
COPD (Chronic Obstructive Pulmonary Disease) doesn’t show up overnight. It creeps in slowly, making breathing harder over time. It’s an umbrella term for two lung conditions: emphysema and chronic bronchitis. Both make it tough to move air in and out, leaving people short of breath, even when they’re just sitting still.
Smoking is the biggest culprit. Years of exposure to cigarette smoke damage the lungs, causing inflammation and scarring. But COPD isn’t just a smoker’s disease. Long-term exposure to air pollution, chemical fumes, or dust on the job can also wreck the lungs. Some people even inherit a genetic condition (alpha-1 antitrypsin deficiency) that makes them more vulnerable, even if they’ve never touched a cigarette.
COPD Subtypes: Emphysema vs. Chronic Bronchitis
COPD isn’t one-size-fits-all. Some people lean more toward emphysema, while others have chronic bronchitis. Some even deal with both.
- Emphysema damages the tiny air sacs in the lungs (alveoli). Instead of stretching and bouncing back like they should, they lose their shape and collapse. That traps air inside the lungs, making exhaling a struggle.
- Chronic bronchitis inflames the airways and fills them with thick mucus. Coughing becomes a daily battle, and breathing feels like trying to suck air through a straw clogged with syrup.
Both conditions block airflow, and neither is reversible. Once the damage is done, it’s permanent. This is why ongoing management is critical to slow progression.
COPD Symptom Checklist
The early warning signs of COPD can be easy to ignore... until they aren’t. A nagging cough or mild breathlessness might not seem like a big deal at first, but as the disease progresses, everyday tasks become exhausting.
Common symptoms include:
- Chronic cough – usually with mucus (the “smoker’s cough”)
- Shortness of breath – even during simple activities like walking
- Wheezing – a whistling or squeaky sound when breathing
- Fatigue – feeling drained from the effort of breathing
- Frequent lung infections – colds and respiratory infections hit harder and linger longer
Unlike asthma, COPD symptoms don’t come and go. They stick around and slowly get worse over time.
Difference Between Asthma and COPD
People mix up asthma and COPD because both can have overlapping symptoms. But they work differently, and knowing the differences of asthma vs. COPD can help with getting the right diagnosis and treatment.
Who Usually Gets It?
Asthma can hit at any age. It’s common in kids but can also appear in adults out of nowhere. Genetics play a role. If a parent has asthma, the chances go up.
COPD, on the other hand, is usually a slow burn. It rarely shows up before age 40, and by the time symptoms appear, lung damage has already been happening for years. Smoking, pollution, and workplace exposures are the biggest risk factors.
Asthma vs COPD Symptoms
One of the biggest clues in telling asthma and COPD apart is how symptoms behave.
- Asthma acts like an on-again, off-again condition. Symptoms flare up, then settle down. One day, breathing might be normal, and the next, a strong perfume or cold air could trigger wheezing and coughing.
- COPD doesn’t take breaks. Symptoms stick around and gradually get worse, making everyday activities harder over time.
Reversibility and Disease Progression
- Asthma symptoms can be reversed with medication. A quick puff from an inhaler or nebulizer treatment can open up the airways and restore normal breathing.
- COPD symptoms don’t fully go away. Inhalers and other treatments can help, but they don’t reverse lung damage that’s already been done.
The longer COPD goes untreated, the harder it becomes to breathe. Even on the best days, people with COPD never fully regain normal lung function.
Asthma-COPD Overlap Syndrome (ACO)
Asthma and COPD aren’t always separate. Some people have both—a condition called asthma-COPD overlap (ACOS). It’s a tricky mix of reversible asthma symptoms and irreversible lung damage from COPD.
People with ACOS tend to have:
- More severe breathing issues than asthma or COPD alone
- More frequent flare-ups that don’t respond as well to standard treatment
- A history of allergies or childhood asthma combined with risk factors for COPD (like smoking or pollution exposure)
Since ACOS doesn’t have a one-size-fits-all treatment, doctors pull from both asthma and COPD treatment plans to manage symptoms. Catching it early is key. It helps slow down lung damage and keeps breathing from getting worse faster than it needs to.
Risk Factors and Triggers
Smoking History
Cigarette smoke is enemy number one when it comes to COPD. It’s responsible for up to 90% of COPD cases. The chemicals in tobacco smoke cause inflammation, scarring, and narrowing of the airways over the years.
Asthma isn’t caused by smoking, but it definitely makes it worse. Smokers with asthma tend to have more severe symptoms, more asthma attacks, and worse lung function compared to non-smokers. Secondhand smoke isn’t harmless either. It can trigger wheezing and coughing in people with asthma, especially kids.
Quitting smoking is the single best thing a smoker can do to slow down COPD or reduce asthma flare-ups. The lungs can’t undo years of damage, but quitting prevents things from getting worse.
Environmental and Occupational Exposures
Smoking isn’t the only cause of COPD. Long-term exposure to airborne pollutants can be just as bad—sometimes worse.
- Workplace hazards: Jobs that involve dust, fumes, chemicals, or tiny airborne particles (think construction, mining, farming, manufacturing, hairdressing, and cleaning) put workers at risk of developing COPD.
- Air pollution: Living in areas with high levels of air pollution can make both asthma and COPD symptoms worse. Pollutants like smoke, exhaust fumes, and industrial chemicals irritate the lungs and trigger inflammation.
- Indoor pollutants: Even inside the home, certain exposures like cooking fumes, cleaning chemicals, and mold can cause breathing problems.
Allergies and Genetics
Some people are born with lungs that don’t handle the environment well. Asthma runs in families, so if a parent or sibling has it, the chances of developing it go up significantly. Many people with asthma also have other allergic conditions, like hay fever (allergic rhinitis) or eczema. Their immune system is more reactive to allergens, which can lead to airway inflammation.
COPD is rarely inherited—except in people with a genetic condition called alpha-1 antitrypsin deficiency (AATD). This condition prevents the body from producing enough alpha-1 antitrypsin, a protein that protects the lungs from damage. Without it, even non-smokers can develop COPD at a young age.
Diagnosing COPD vs Asthma
Pulmonary Function Tests (PFTs)
The first step in diagnosing asthma or COPD is checking how well the lungs work. Pulmonary function tests (PFTs) measure how much air a person can breathe in and out, and how fast they can do it.
The most common test is spirometry. A person takes a deep breath and blows into a machine as hard and fast as they can. The test measures some key numbers:
- FEV1 (Forced Expiratory Volume in 1 Second) – How much air a person can blow out in one second.
- FVC (Forced Vital Capacity) – The total amount of air exhaled after a deep breath.
- FEV1/FVC Ratio – The percentage of air exhaled in one second compared to total lung capacity.
In healthy lungs, the FEV1/FVC ratio is above 70%. In obstructive diseases like asthma and COPD, this number drops because it’s harder to push air out.
Bronchodilator Reversibility and Methacholine Challenge
A key difference between asthma and COPD is how the lungs respond to medication.
- Bronchodilator Reversibility Test: After the spirometry test, the patient uses a bronchodilator (a medication that opens the airways). After 15-20 minutes, they take the test again.
- Asthma: Lung function improves significantly (FEV1 increases by 12% or more).
- COPD: Little to no improvement, since lung damage is permanent.
- Methacholine Challenge Test: Methacholine is a drug that triggers airway narrowing.
- Asthma: Airways react strongly, causing a drop in lung function.
- COPD: Little or no reaction.
These tests help doctors confirm asthma, COPD, or an overlap of both.
Imaging and Lab Tests
Lung function tests tell a lot, but sometimes imaging or blood tests are needed to rule out other conditions.
- Chest X-ray – Used to check for lung infections, scarring, or emphysema
- CT Scan – Provides a detailed look at lung damage in COPD
- Arterial Blood Gas (ABG) Test – Measures oxygen and carbon dioxide levels in the blood to see how well the lungs are functioning
These tests aren’t always necessary but can help confirm a diagnosis or assess lung damage. For people who deal with breathing problems regularly, an early diagnosis can mean the difference between managing symptoms and struggling to breathe.
Treatment Options Side-by-Side
Medications and Inhalers
When it comes to managing symptoms for asthma vs. COPD, inhalers are the go-to treatment because they quickly get medication into the lungs. But not all inhalers work the same way.
- Rescue inhalers (short-acting bronchodilators) – These act fast to open airways during an asthma attack or sudden COPD flare-up. They provide quick relief but don’t last long.
- Maintenance inhalers (long-acting bronchodilators) – Used daily to keep symptoms under control. These work for 12+ hours and help prevent flare-ups.
Other medications can be added depending on how severe the condition is:
- Inhaled corticosteroids (ICS) – Reduce inflammation in the lungs. More common in asthma treatment but sometimes used in COPD.
- PDE4 inhibitors – Used for COPD to reduce inflammation and prevent exacerbations.
- Biologic medications – Advanced treatment for severe asthma that doesn’t respond well to traditional inhalers. These target specific immune responses that trigger asthma attacks.
- Hypertonic saline - Inhaled saline with a higher salt concentration is often recommended by lung doctors to manage mucus in chronic bronchitis.
Nebulizers
Inhalers are small and convenient, but they aren’t the best option for everyone. Some people with weaker muscles aren’t able to effectively use an inhaler. Inhalers are also expensive and cost more out of pocket. That’s where nebulizers are a great alternative.
- A nebulizer turns liquid medication into a fine mist, making it easier to inhale.
- Best for: Infants, young children, elderly patients, or anyone who has difficulty using an inhaler correctly.
- Useful during flare-ups – Inhalers require a deep, controlled breath, which can be tough when breathing is already difficult. Nebulizers deliver medication passively, so patients can breathe normally while getting treatment.
A portable nebulizer (like TruNeb™) makes treatments even easier by eliminating the need for bulky machines and tubing. It’s small, quiet, and battery-powered, making it perfect for travel or on-the-go relief.
Lifestyle Adjustments
Managing asthma or COPD involves more than medications. Small lifestyle changes can dramatically improve breathing and reduce flare-ups.
- Quit smoking. This is the single best decision for anyone with COPD and asthma.
- Stay active. Light exercise (walking, swimming, yoga) helps strengthen the lungs. But overdoing it or skipping warm-ups can trigger asthma symptoms, so pacing is key.
- Avoid triggers. Allergens, pollution, strong scents, and even cold air can set off symptoms. Keeping a clean indoor environment and using an air purifier can help.
- Get vaccinated. Flu, pneumonia, and COVID-19 can hit people with asthma or COPD harder. Staying up to date on vaccines can prevent severe respiratory infections.
Pulmonary Rehabilitation
For people with moderate to severe symptoms, COPD self care and pulmonary rehab can make all the difference:
- Exercise training – Helps improve lung efficiency and stamina.
- Breathing techniques – Teaches methods like pursed-lip breathing to reduce breathlessness by creating more back pressure in the lungs.
- Nutritional counseling – Weight plays a role in breathing—excess weight makes it harder, while being underweight can weaken muscles. Proper nutrition helps maintain lung function.
Pulmonary rehab is standard for COPD but can also benefit people with severe asthma who struggle with daily activities.
Answering Your Questions: Asthma vs COPD
Is asthma restrictive or obstructive?
Asthma is obstructive, meaning air gets trapped in the lungs because of narrowed airways. Restrictive lung diseases, like pulmonary fibrosis, make it hard to expand the lungs fully.
Think of it this way:
- Obstructive disease (asthma, COPD) = Air gets in but has trouble getting out.
- Restrictive disease = Air can’t get in properly
Can asthma become COPD?
No, but there’s a connection. Childhood asthma doesn’t automatically turn into COPD, but if asthma is poorly controlled for years, the airways can become permanently damaged.
Smokers with asthma are at higher risk of developing COPD later in life. This combination is called asthma-COPD overlap (ACOS), which means they have traits of both conditions.
What’s the difference between asthma and COPD at older ages?
Asthma can appear for the first time in adulthood, leading to confusion with COPD. Here’s how to tell them apart:
- Asthma in older adults still follows its classic pattern—symptoms come and go, typically triggered by allergens or activity.
- COPD in older adults is usually linked to smoking history and progressively gets worse, regardless of exposure to triggers.
When should I use a nebulizer instead of an inhaler?
A nebulizer might be the better option if:
- Inhalers aren’t delivering enough relief.
- A person struggles to use an inhaler correctly (common in young children and older adults).
- Severe asthma or COPD flares make it difficult to take deep breaths.
- Someone needs a higher dose of medication than an inhaler can provide.
Portable nebulizers are especially useful for people who need quick, effective treatment without the hassle of a traditional bulky machine. They deliver consistent, deep medication penetration, which can be a lifesaver during exacerbations.
Breathe Better, Feel Better
For people with asthma and COPD, the TruNeb™ Portable Nebulizer is a convenient treatment option to add into your routine. Breathing treatments take around 5 minutes, and there’s no bulky machines or tubing to worry about.