On this page
Asthma and pregnancy can go hand in hand, and most people with well‑controlled asthma have healthy pregnancies. This guide covers how asthma can change, the risks of poor control, medicines, labor, and the postpartum period.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your own symptoms, medications, and treatment decisions.
How Pregnancy Affects Asthma and Why Control Matters
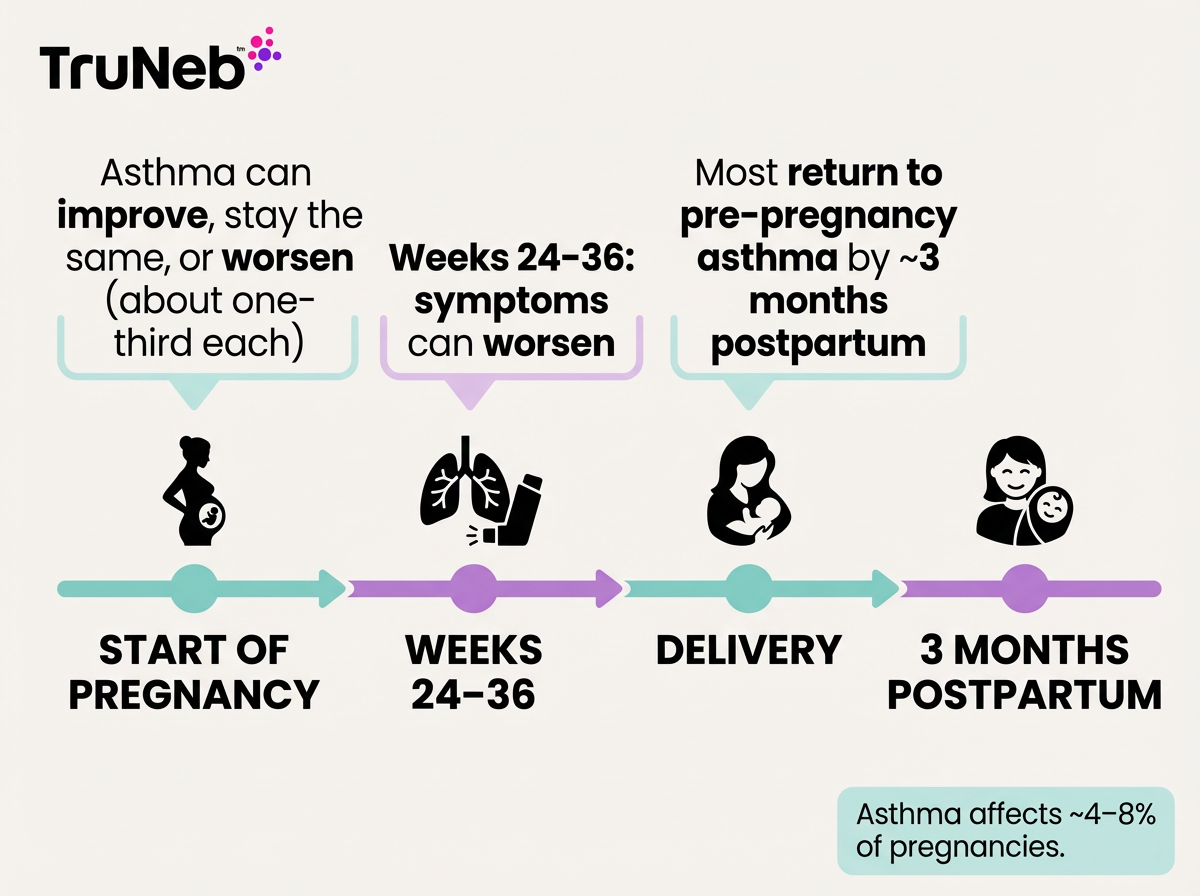
Asthma during pregnancy can change. For some, it gets easier. For others, it gets harder. About one‑third stay about the same. Doctors call this the one‑third rule. Asthma affects about 4–8% of pregnancies.
Symptoms are most likely to flare between weeks 24 and 36. After delivery, most people return to their usual asthma within about three months. That’s normal.
These changes mostly come from pregnancy hormones and how your body grows. Progesterone can make you feel short of breath even when your lungs are working fine. Estrogen can cause a stuffy nose. Your growing belly also lifts the diaphragm a bit. If you’re unsure whether shortness of breath is from pregnancy or asthma, check in with your asthma doctor.
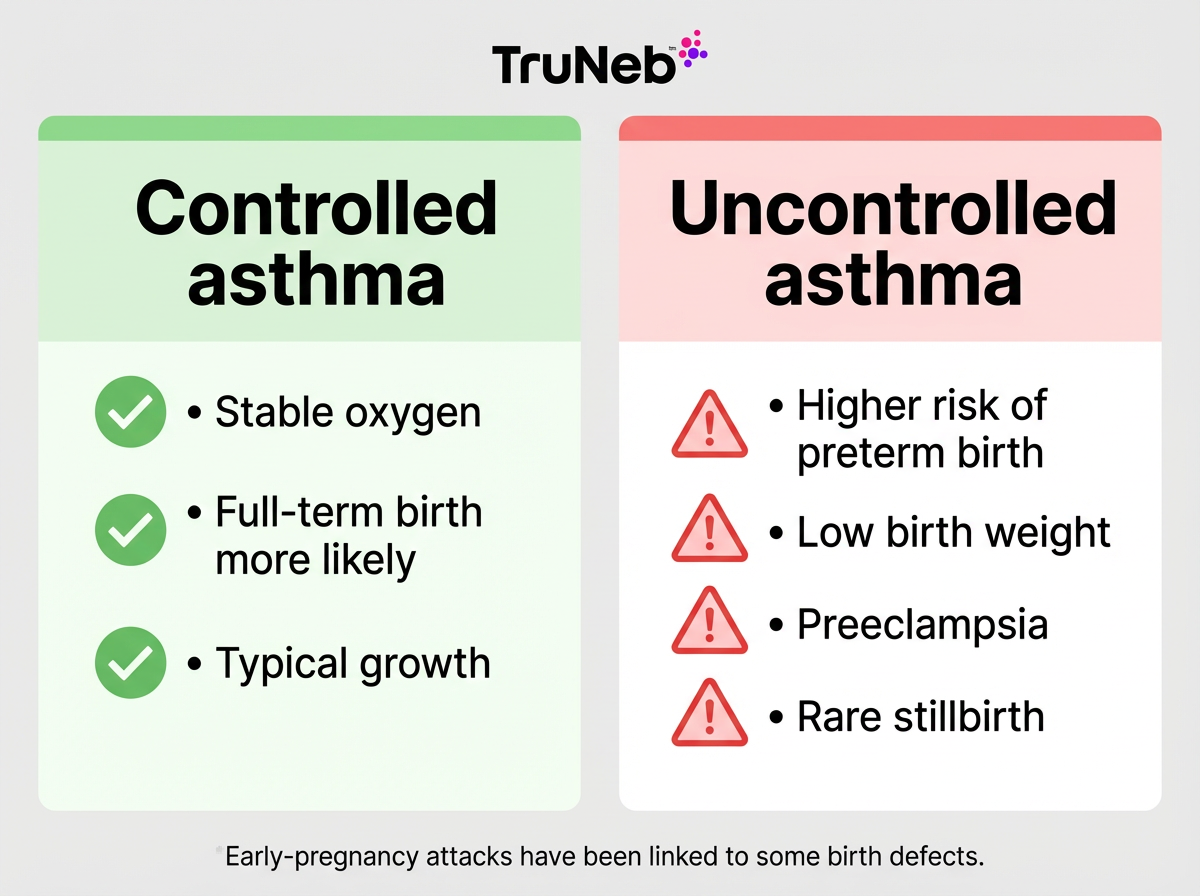
Control matters. Controlled asthma means few daytime symptoms, little to no night waking, and rare need for your rescue inhaler. When asthma is controlled, oxygen stays steady for you and your baby. With good control, outcomes are usually the same as pregnancies without asthma. If asthma isn’t controlled, the risks go up. Simple steps—following your prescribed treatment, avoiding triggers, and keeping up with appointments—can make a real difference. Let your OB/GYN and asthma doctor know about your asthma early in pregnancy so they can support your plan.
With a good plan and support from your doctors, asthma doesn’t have to stand in the way of a healthy pregnancy.
Takeaway: In pregnancy, about one‑third of people with asthma get worse, one‑third improve, and one‑third stay the same.
Risks of Uncontrolled Asthma vs Asthma Medications
The bigger risk in pregnancy isn’t the medicine—it’s uncontrolled asthma. Asthma attacks can lower oxygen levels for you and your baby, which can be harmful if they’re not treated quickly.
Uncontrolled asthma can raise the chance of:
- High blood pressure/preeclampsia (pregnancy‑related hypertension)
- ER visits or hospitalization for severe attacks
- Preterm birth and low birth weight
- In rare cases, stillbirth
- Early‑pregnancy attacks have been linked to some birth defects, so getting control early is key
What about medicines? Inhaled treatments have low body absorption. Inhaled corticosteroids (like budesonide) and quick‑relief albuterol have strong safety records in pregnancy. Stopping your meds on your own isn’t safe.
When asthma is well controlled in pregnancy, outcomes are similar to pregnancies without asthma. The goal is simple: keep asthma controlled so oxygen stays steady. Your doctor will help choose the least medicine needed to keep you well.
Takeaway: Uncontrolled asthma raises risks; well‑controlled asthma carries little to no extra risk.
Working with Your OB/GYN and Asthma Specialist
Let both doctors know you have asthma as soon as you’re pregnant. Ask if they can share one asthma plan so everyone’s working from the same playbook. That way, changes can be made early if you need them.
Some prenatal visits include a brief asthma check‑in. It’s a good idea to bring your rescue inhaler to every appointment. Keep your written asthma action plan with you, and make sure it’s in your chart. Your team may track control with a peak flow meter or quick lung‑function checks (spirometry) to catch issues early. If your asthma is moderate or severe, your OB can loop in a maternal‑fetal medicine specialist if needed.
For delivery, make sure your meds are on your birth plan. Your team will choose pain control and anesthesia options that are safe for asthma.
Takeaway: Sharing one written asthma action plan with both your OB and asthma doctor keeps everyone on the same page about your care.
Tips for Managing Asthma and Preventing Attacks During Pregnancy
Safety note: Talk to your doctor before changing any medication. Here are practical tips for managing asthma while pregnant.
- Avoid triggers: Avoid smoking and secondhand smoke completely—your doctor will strongly recommend this. Reduce dust mites (wash bedding hot, use mattress/pillow covers), mold, pet dander, pollen, strong smells, and cold air.
- Monitor symptoms: Track how often you need your rescue inhaler. Some people use a peak flow meter or a simple symptom diary to spot patterns. If it’s more than your plan allows, call your doctor.
- Follow your action plan: Keep it handy. Know your green/yellow/red zones and what to do in each.
- Ask about vaccines: Ask about getting a flu shot (and other vaccines your OB recommends). Infections can trigger serious asthma flares.
- Support your lungs: Sleep, hydrate, and stay active with your doctor’s okay. Manage heartburn, since reflux can trigger symptoms. Practice calm breathing—these skills also help in labor.
If your symptoms don’t improve over a few days or you’re using your rescue inhaler more than your plan allows, check in with your doctor to review your asthma plan. ⚠️ If you ever have severe trouble breathing, can’t speak in full sentences, or notice blue lips or fingernails, call 911 or seek emergency care right away.
Small, steady steps add up. The aim is fewer triggers, fewer flares, and steady oxygen for you and your baby.
Takeaway: During pregnancy, avoid triggers, follow your plan, and get recommended vaccines to cut attack risk.
Asthma Medications During Pregnancy: What’s Safe and What to Adjust
Most standard asthma medicines can be used in pregnancy. Inhaled medicines are preferred because they act in the lungs with little medicine reaching the rest of the body.
Controllers
- Inhaled corticosteroids (ICS): First‑line for persistent asthma. Budesonide has the most pregnancy safety data.
- Add‑on therapy: LABAs (with an ICS) or montelukast are sometimes used if your doctor recommends them.
Rescue
- Albuterol: Quick relief and considered safe. Doctors usually recommend keeping it with you.
When symptoms spike
- Doctors sometimes prescribe short courses of oral steroids for severe attacks. The risk from an untreated severe flare is higher than the risk from a brief steroid burst.
Allergies and shots
- Several antihistamines and steroid nasal sprays are acceptable—ask your OB.
- If you were already on allergy shots, your specialist can continue your maintenance dose. Don’t start new shots during pregnancy.
Inhaler vs nebulizer
- Most people do well with inhalers (use a spacer if prescribed). If your doctor recommends nebulized medicine, a portable mesh device can make treatments quieter and more convenient at home or on the go.
- Nebulizers and inhalers typically use the same medications—a nebulizer just delivers them as a mist over several minutes.
- Some doctors recommend saline‑only neb sessions for mucus relief. If so, use medical‑grade sterile saline (3% or 7%) made in FDA‑approved facilities, and follow your doctor’s directions. Hypertonic saline isn’t a primary asthma treatment and can irritate airways in some people, so use it only as directed.
- ⚠️ Don’t use steam inhalers for asthma medicine - steam devices aren’t the same as nebulizers and don’t deliver medication to your lungs.
Important: Never start, stop, or change asthma treatment on your own. Talk to your doctor before trying a new medication.
Takeaway: Inhaled asthma medicines are the first choice in pregnancy, and drugs like budesonide and albuterol have strong safety records.
Key takeaway: Inhaled medicines are preferred in pregnancy; budesonide and albuterol have strong safety records. Nebulizers and inhalers use the same medications—your doctor will tailor the device to you.
| Treatment | Role in pregnancy | Typical notes |
|---|---|---|
| Budesonide (inhaled corticosteroid, ICS) | Controller for persistent asthma | Most pregnancy safety data; continue if prescribed unless your doctor changes it |
| Albuterol (short‑acting beta‑agonist, SABA) | Quick‑relief rescue | Keep available per your plan; considered safe in pregnancy |
| LABA + ICS or montelukast | Add‑on controller | Sometimes used when needed under doctor guidance |
| Short oral steroid burst | Severe flare | Short courses are used when needed; untreated severe flares are riskier |
| Delivery method: inhaler + spacer vs nebulizer | How medicine is delivered | Same medications; nebulizer gives a fine mist over minutes; device choice depends on technique and doctor recommendation |
| Allergy shots (immunotherapy) | Allergic asthma support | Continue only if already on maintenance; don’t start during pregnancy |
| Saline nebulization (3% or 7%) | Mucus relief (not a primary asthma treatment) | Use medical‑grade sterile saline only if directed; can irritate airways |
Notes: Nebulizers and inhalers use the same medications; a nebulizer isn’t “stronger.” Steam inhalers are not nebulizers and aren’t used to deliver asthma medicine.
Asthma and Labor and Delivery: What to Expect
Most people with well‑controlled asthma go through labor without breathing problems. Asthma attacks during labor are uncommon. Symptoms often improve late in the third trimester.
Bring your inhaler. If you use a nebulizer, pack it or confirm the hospital has one ready. Tell your team about your asthma history and medicines. Most people continue their usual asthma medicines right up to and during labor, unless their doctor advises otherwise.
Pain control and anesthesia can be tailored for asthma. If a C‑section is needed, anesthesiologists choose options that avoid bronchospasm and can even help open the airways. Breathing techniques you practiced for labor also help you stay calm and well‑oxygenated.
Takeaway: Asthma attacks during labor are rare, and your team will be ready just in case.
Postpartum and Breastfeeding with Asthma
After birth, most people return to their pre‑pregnancy asthma within a few months. Still, keep your plan going—newborn life can mean less sleep and more germs, which can trigger symptoms.
Good news: most asthma medicines are compatible with breastfeeding. Inhaled medicines enter breast milk in tiny amounts and are not known to harm babies. If you need a short course of oral steroids, your doctor can guide timing and dosing. Breastfeeding can offer benefits for your baby’s immune system and lungs.
Stay in touch with your asthma doctor. If your plan was stepped up during pregnancy, ask when it’s safe to step back down.
Takeaway: Most asthma medicines are compatible with breastfeeding, and asthma usually returns to its pre‑pregnancy pattern within a few months.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Don’t stop on your own. Most inhaled treatments are considered safe in pregnancy. Review your medicines with your doctor and follow your written asthma action plan.
Most asthma action plans tell you to use your quick‑relief inhaler or prescribed nebulizer right away, then recheck symptoms. If you don’t improve quickly, follow your plan’s emergency steps—which usually means urgent or emergency care. ⚠️ If your breathing is getting worse, you can’t speak in full sentences, or you notice blue lips or fingernails, call 911 or seek emergency care immediately.
Yes. A nebulizer is just a delivery device and is used in pregnancy when needed. Nebulizers and inhalers usually use the same medications. Saline‑only neb sessions for mucus should be done only if your doctor recommends them, using medical‑grade sterile saline (3% or 7%). Steam inhalers are not nebulizers and aren’t used to deliver asthma medicine.
Usually, yes. Light to moderate activity is fine for many people with asthma during pregnancy, with your doctor’s approval. Warm up, avoid triggers, and keep your quick‑relief inhaler handy.
No. Pregnancy itself doesn’t cause asthma. Hormone and immune changes can unmask symptoms in someone who already had mild, undiagnosed asthma.
Not necessarily. A parent with asthma can raise a child’s risk, but lots of children of parents with asthma never develop it. Avoid smoke, manage home allergens, and consider breastfeeding to support your baby’s lungs.
Most standard asthma medicines are acceptable in pregnancy. Your doctors will avoid a few drugs when possible and choose time‑tested options. Always check with your doctor before starting anything new.
Usually, yes. Most people return to their pre‑pregnancy asthma within about three months. Stay in touch with your asthma doctor to adjust your plan if needed.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your own symptoms, medications, and treatment decisions.