On this page
Asthma–COPD Overlap Syndrome: What It Means and Why It Matters
Asthma–COPD Overlap Syndrome, also called ACOS, means you have features of both asthma and chronic obstructive pulmonary disease at the same time. It's not a separate disease. You might also see this called asthma–COPD overlap (ACO). Doctors use this term to choose tests and combine treatments that address both asthma‑type inflammation and COPD‑type lung damage.
Why it matters: people with ACOS usually have worse symptoms and more flare‑ups than with asthma or COPD alone. Getting the right plan can improve breathing and reduce hospital visits. Studies suggest ACOS affects a smaller but meaningful share of adults with chronic airway disease.
Key Takeaway: ACOS means asthma and COPD features occur together, so treatment must address both.
Asthma vs COPD: How They Differ and Overlap
Asthma and COPD share shortness of breath, cough, and wheeze, but they aren't the same.
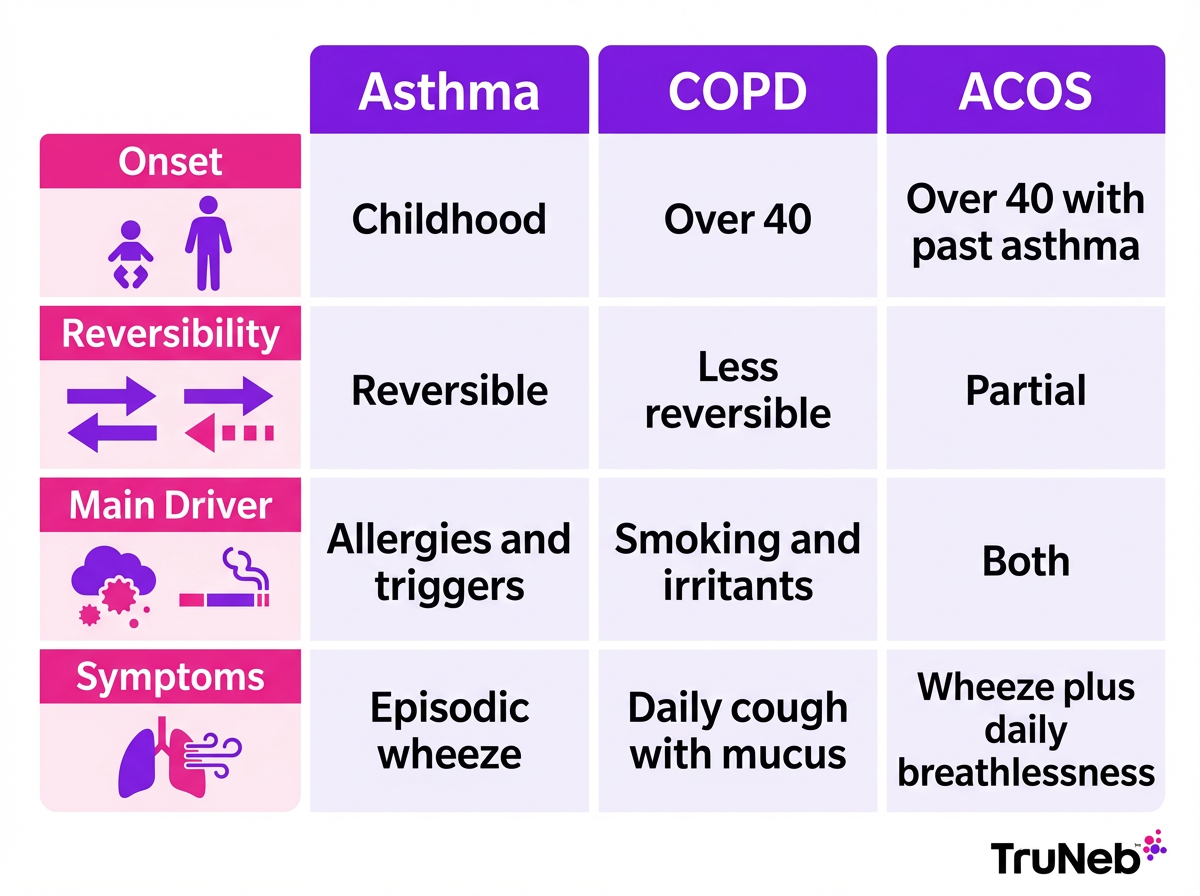
How they differ:
- Typical age: asthma usually starts in childhood or young adulthood; COPD usually appears after age 40.
- Reversibility: asthma airflow blockage usually improves a lot with medicine; COPD airflow blockage is less reversible and tends to worsen over time.
- Triggers: asthma is linked to allergies, exercise, and cold air; COPD is tied to years of smoking or irritant exposure and includes chronic bronchitis and emphysema.
- Mucus: COPD commonly brings daily cough with phlegm; asthma cough comes and goes.
Where they overlap:
- Some people have both patterns. For example, someone who had asthma and also smoked can develop airflow blockage that doesn't fully go away along with asthma flare‑ups. Doctors call this overlap ACOS.
Key Takeaway: Asthma is usually reversible and trigger based, COPD is long term and less reversible, and ACOS sits where they meet.
Signs and Symptoms of ACOS
People with ACOS can have daily symptoms like COPD and variable, asthma‑style symptoms that come and go.
Common symptoms:
- Shortness of breath that worsens with activity.
- Wheezing, a whistling sound when you breathe.
- Chronic cough that can bring up mucus.
- Chest tightness or pressure.
- Fatigue and low exercise tolerance.
ACOS is also linked to more frequent flare‑ups (exacerbations) than having only asthma or only COPD.
Key Takeaway: ACOS symptoms combine daily breathlessness with asthma‑style wheeze and frequent flare‑ups.
Causes and Risk Factors for ACOS
ACOS doesn't have one single cause. It happens when risk factors for asthma and COPD come together over time.
What raises risk:
- Smoking or long‑term exposure to fumes, dust, or biomass smoke.
- A personal or family history of asthma or allergies.
- Age over 40, when long‑term smoke damage starts to show.
- Occupational exposures, like chemicals or dusts.
- Some studies show higher COPD risk in women.
People with long‑standing asthma who smoke are especially likely to develop COPD‑type changes later, leading to ACOS. For example, someone who had asthma growing up and smoked for years might develop constant breathlessness and daily cough in midlife.
Key Takeaway: Most ACOS patients have a mix of past asthma and years of smoke or irritant exposure.
Diagnosing Asthma–COPD Overlap
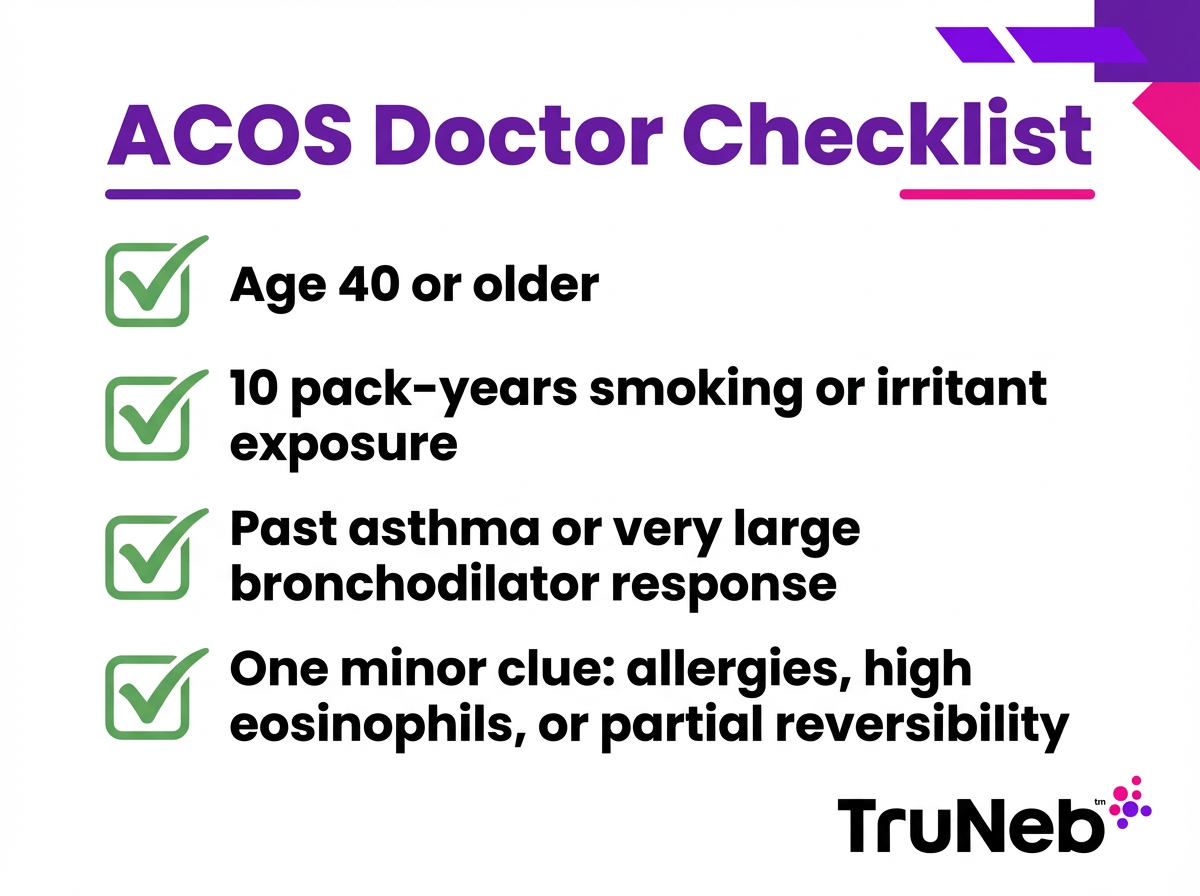
There's no single lab test for ACOS. Doctors look for a pattern using your history and lung tests.
What doctors check:
- History: past asthma or allergies, plus a long smoking or irritant exposure history.
- Symptoms: both daily breathlessness and variable wheeze or chest tightness.
- Spirometry: a breathing test that shows airflow blockage that doesn't fully go away after a bronchodilator. Spirometry typically shows a low FEV1/FVC ratio (meaning you can't blow air out as quickly as expected) that improves some, but not all the way.
Experts use different sets of criteria, and there isn't one universally agreed‑upon definition. A common framework includes three major items: chronic airflow limitation after a bronchodilator, a smoking or irritant exposure history, and a past diagnosis of asthma or a very large bronchodilator response. One or more minor clues can support the diagnosis, like allergy history, high blood eosinophils, or partial reversibility.
Chest X‑rays, CT scans, and some blood tests can add clues, but your doctor mainly puts the pieces together from your story and breathing tests. These criteria are tools for doctors, not something you can diagnose yourself at home.
Key Takeaway: ACOS is a clinical diagnosis based on history plus spirometry that shows fixed airflow (airways that stay narrowed) with partial reversibility.
Treatment Options for Asthma–COPD Overlap
There's no single medicine that fixes ACOS, but the right mix can cut symptoms and flare‑ups. Treatment is individualized and set by your doctor, and most plans address both inflammation and airflow blockage.
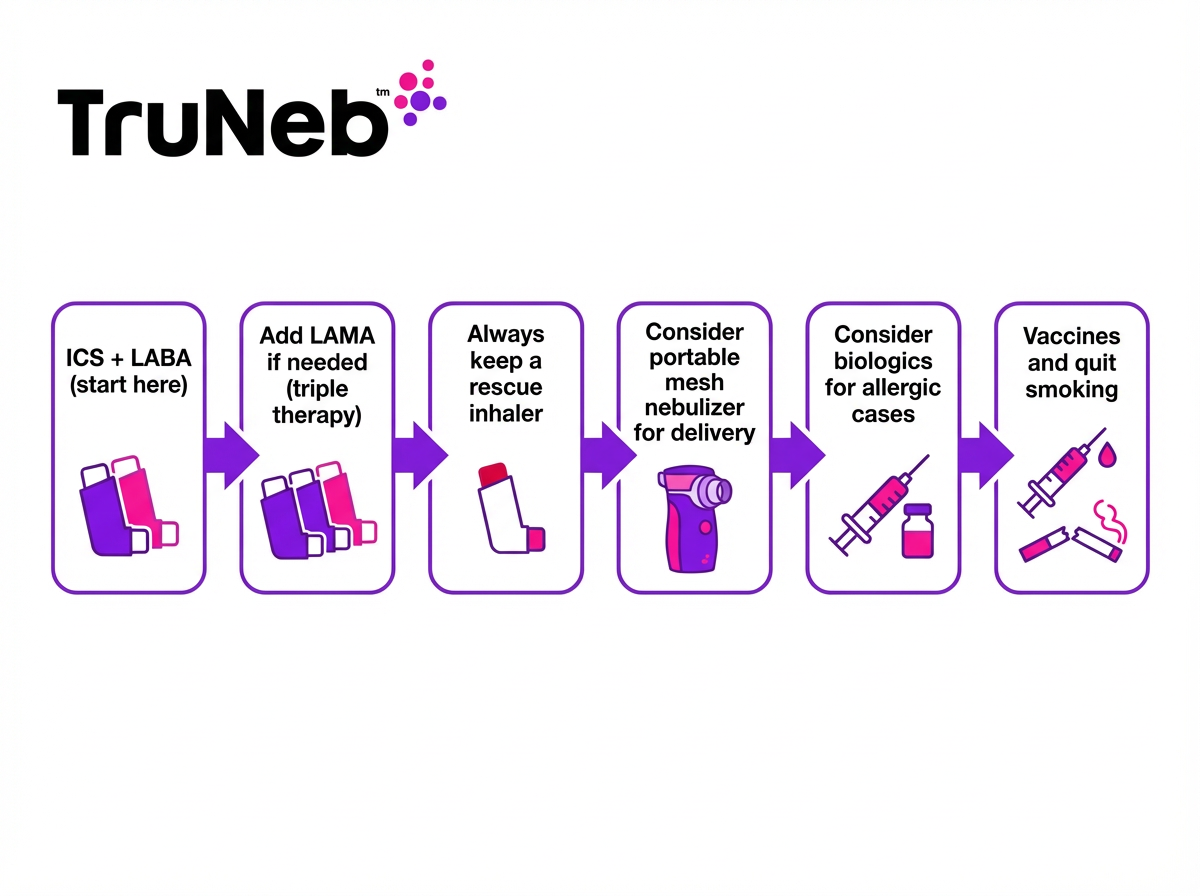
Core medicines:
- Inhaled corticosteroids (ICS): daily controllers that calm airway inflammation. Usually a key part when asthma features are present.
- Long‑acting bronchodilators: LABA and LAMA relax and open airways for many hours. Doctors pair LABAs with an ICS when asthma features are present. Triple therapy (ICS + LABA + LAMA) can help when symptoms persist despite simpler regimens.
- Quick relief: a short‑acting bronchodilator for sudden shortness of breath.
If allergic features are strong and symptoms persist, specialist‑directed injected biologic medicines can be considered.
Key Takeaway: Most ACOS treatment plans combine a daily steroid inhaler with one or more long‑acting bronchodilators.
Inhalers vs Nebulizers: Getting Medicine In
Most ACOS medicines come as inhalers. Some people also use a nebulizer, which turns liquid medicine into a fine mist you breathe in through a mask or mouthpiece. A nebulizer can help if you struggle with inhaler technique or need longer treatments during a flare, and doctors sometimes add one in those situations.
Portable mesh nebulizers make this easier than older tabletop machines. A handheld device is quiet and portable, which can make it easier to fit treatments into daily life.
Consumer tip: you might see products labeled "steam inhaler"—these are not nebulizers and shouldn't be used to deliver prescription medications.
Key Takeaway: Inhalers are usually used for daily control, while a nebulizer can help when someone needs a slower, deeper inhaled treatment or has trouble using inhalers.
Airway Clearance and Mucus Management
People with ACOS commonly deal with thick mucus from the COPD side of the overlap.
What can help:
- Hydration and breathing techniques like huff coughing to move mucus.
- Chest physiotherapy or airway clearance exercises as taught in pulmonary rehab.
- Sometimes, a doctor can suggest nebulized saline to thin secretions. Hypertonic saline, such as 3% or 7%, draws water into the airway and can make mucus easier to cough up. TruNeb offers 3% and 7% hypertonic saline for nebulizer use.
Important: this approach isn't standard for everyone with ACOS and is used more in chronic bronchitis‑type disease. Asthmatic airways can be sensitive, and some people feel more wheezy with saline. Talk to your doctor before trying hypertonic saline or any new nebulizer solution.
Key Takeaway: Hypertonic saline can thin mucus, but only use it under medical guidance in ACOS.
Lifestyle Changes and Home Management
Daily habits can make a big difference with ACOS.
- If you smoke, quitting is the most important step to slow lung damage and improve how well treatments work. Your doctor can help you find a quitting plan that fits you.
- Reduce exposure to irritants. Limit secondhand smoke, heavy dust, chemical fumes, and outdoor air pollution when possible. Control indoor allergens if you're allergic.
- Vaccines. Doctors usually recommend annual flu shots and pneumococcal vaccines to lower the risk of severe infections and hospital stays.
- Pulmonary rehabilitation. Supervised exercise, breathing techniques, and education can raise stamina and confidence.
- Regular follow‑ups and an action plan. Regular visits with your doctor and a written plan for flare‑ups can help you stay on top of ACOS.
Small, steady changes add up to easier breathing and better days.
Key Takeaway: Quitting smoking and staying vaccinated are two of the biggest wins for ACOS.
Prognosis and Outlook
ACOS can be serious. People usually have more flare‑ups and a lower quality of life than with asthma alone. In studies, overall outlook is similar to people who have COPD of the same severity.
ACOS can affect life expectancy, especially when the COPD component is severe, but outcomes vary widely by person. The good news: quitting smoking, taking daily medicines as prescribed, getting vaccines, and staying active can slow decline and reduce hospital visits. Your outlook depends on how severe your COPD features are and how well your asthma is controlled.
Stay proactive with care, and you can improve your course over time.
Key Takeaway: ACOS outcomes usually mirror COPD severity, but good care can improve your long‑term course.
Safety Note
This article is for informational purposes only and is not a substitute for professional medical advice. Always talk to your doctor before trying a new medication, changing a dose, or starting treatments like hypertonic saline.
⚠️ If you have severe trouble breathing, chest pain, blue lips or fingers, or can't speak in full sentences, call 911 or your local emergency number right away.
Key Takeaway: Always talk to your doctor before changing ACOS medications or starting treatments like hypertonic saline.
FAQs: Asthma–COPD Overlap Syndrome
Tap or click a question below to see the answer:
Yes. Having both at once is called Asthma–COPD Overlap Syndrome (ACOS or ACO). It means features of both conditions show up together, like asthma‑style wheeze and COPD‑type breathlessness.
Doctors use spirometry and your medical history to look for an ACOS pattern; there's no single test. They check for airflow blockage that doesn't fully improve after a bronchodilator, plus clues like past asthma and smoking or irritant exposure. Experts use different criteria, so your doctor puts the pieces together from your story and tests.
Asthma usually has trigger‑based symptoms and airflow blockage that improves a lot with medicine. COPD involves long‑term lung damage from smoking or irritants with less reversible airflow blockage and includes chronic bronchitis and emphysema. ACOS is where both patterns show up in one person.
Doctors often prescribe a daily inhaled corticosteroid along with one or two long‑acting bronchodilators. They typically also provide a rescue inhaler for sudden symptoms and recommend quitting smoking, staying up to date on vaccines, and considering pulmonary rehab. Your doctor will tailor the plan to your needs.
Yes, ACOS can affect life expectancy, especially if lung damage is severe, but outcomes vary widely by person. Good care can improve quality of life, reduce flare‑ups and hospital visits, and support better long‑term health.
Both inhalers and nebulizers can work for ACOS. Inhalers are usually used for daily control, and a doctor might recommend a nebulizer if you have trouble with inhaler technique or during flares. A portable mesh nebulizer like TruNeb can be a quiet, travel‑friendly option. Ask your doctor which option fits your situation.
Key Takeaway: ACOS is the overlap of asthma and COPD; diagnosis uses spirometry and history, treatment combines inhaled steroids with bronchodilators, and daily habits matter.