On this page

Why Cold Weather Makes Asthma Worse
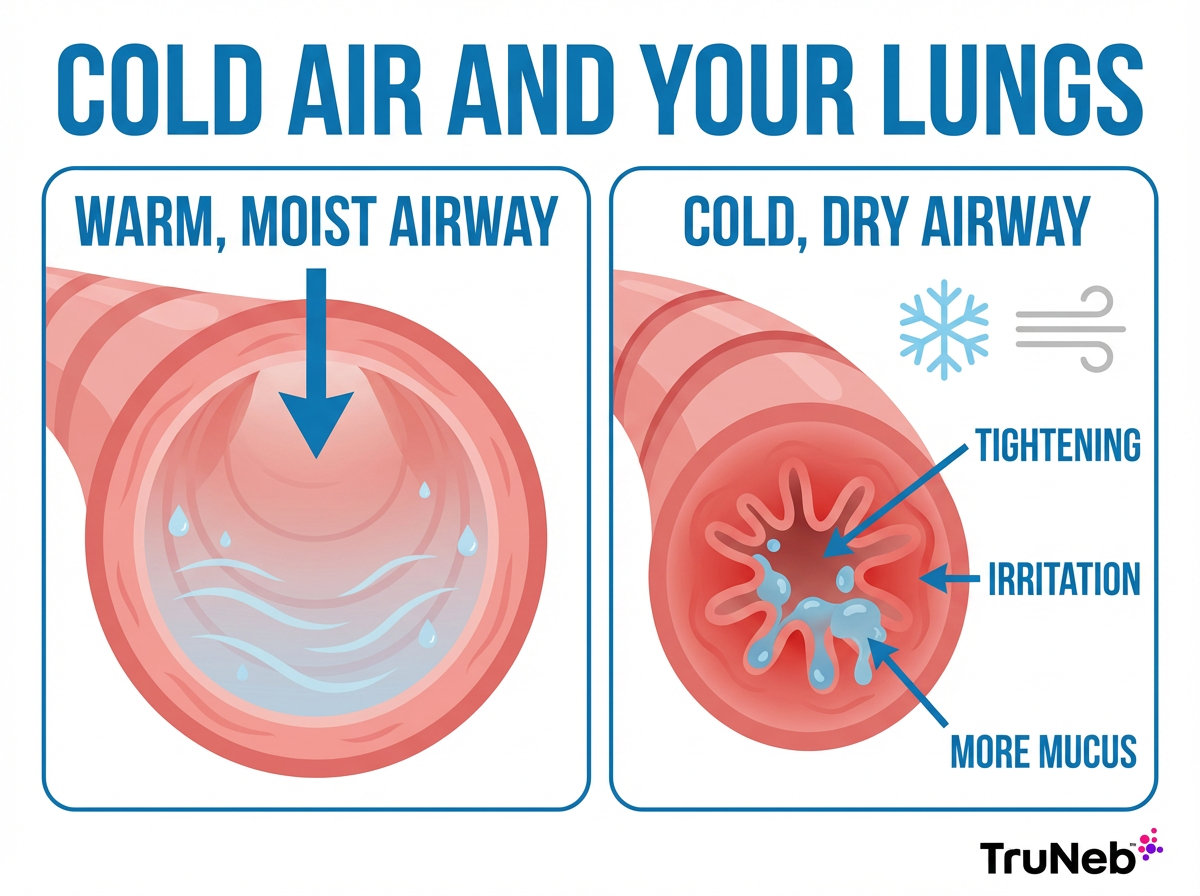
Yes. Cold weather can make asthma worse. Cold, dry air cools and dries the lining of your airways. That can trigger bronchospasm, which means the muscles around your bronchial tubes tighten. The result is coughing, wheezing, chest tightness, and shortness of breath.
What happens inside your lungs:
- Cold, dry air pulls heat and moisture out of your airways. Dry tissue gets irritated and more sensitive.
- Your airways can release chemicals like histamine that tighten airway muscles.
- Sudden temperature changes, like stepping from a warm room into icy wind, can spark symptoms fast.
- Winter viruses like colds and flu inflame airways and increase mucus, adding to cold-air irritation.
People sometimes call this cold-induced asthma. Cold-induced asthma isn't a separate diagnosis; it's your regular asthma reacting to cold, dry air. If Asthma and the Cold Weather feels like a bad mix for you, you're not imagining it.
Bottom line: Cold, dry air narrows and dries your airways, which is why asthma can feel worse in winter.
Protecting Your Airways from Cold and Dry Air
The goal is simple: warm and moisten the air before it reaches your lungs. These winter asthma management tips can help reduce flare-ups and winter asthma attacks.
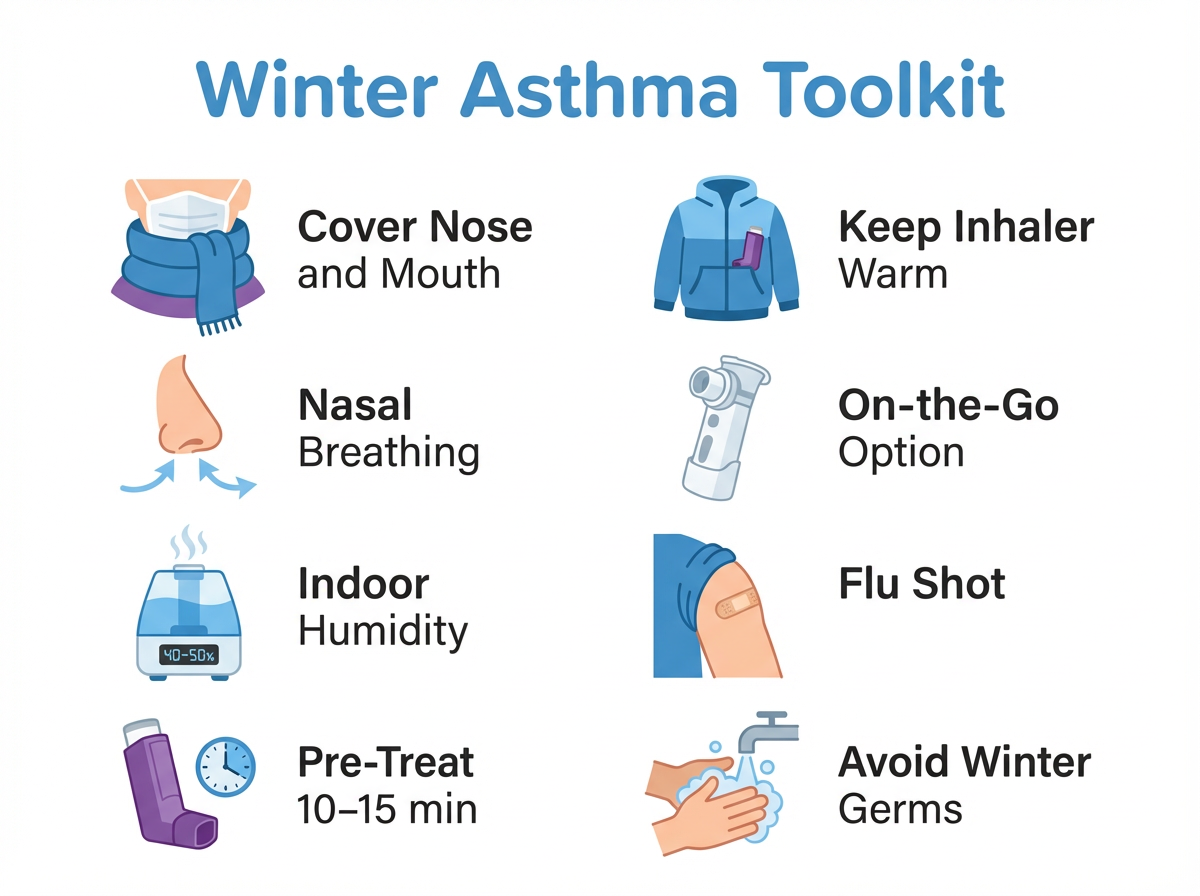
- Cover your nose and mouth: A soft scarf or a cold-weather mask warms and humidifies the air you breathe. This is one of the easiest ways to prevent winter asthma attacks.
- Breathe through your nose: Your nose warms and moistens air better than your mouth. A saline nasal spray can help if stuffiness makes nose breathing hard.
- Layer up: Keep your chest, neck, and face warm. A high-collar coat or neck gaiter helps block cold wind.
- Use a humidifier indoors: Heating dries out indoor air. Aim for about 40 to 50 percent humidity. Clean the unit regularly and use a small hygrometer so you don't over-humidify.
⚠️ If you see steam inhalers near nebulizers in the store, they're not the same. Steam inhalers aren't for breathing prescribed asthma medications.
- Take warm-up breaths: Before you step outside or start moving fast, take slow breaths through your scarf for a minute to pre-warm your lungs.
- Sip warm fluids and stay hydrated: Warm tea or water can soothe your throat, and hydration helps keep mucus thin.
These tips for asthma in cold weather create a warmer, wetter air buffer for your lungs and cut cold weather asthma triggers.
Key takeaway: Nebulizers deliver prescribed asthma medication; steam inhalers and humidifiers don't.
| Device | Main purpose | Delivers asthma meds? | When it's used | Cleaning |
|---|---|---|---|---|
| Nebulizer (mesh or jet) | Turns liquid medication into a mist | Yes, with doctor-prescribed solutions | As part of your asthma action plan | Rinse, disinfect per device guide |
| Steam inhaler | Warm steam for comfort | No | Not for asthma meds; can worsen swelling if misused | Empty water, clean to prevent mineral buildup |
| Humidifier | Adds moisture to room air | No | Dry indoor air; aim for 40–50% humidity | Clean regularly to prevent mold and germs |
Key takeaway: Warm and moisten the air you breathe to lower your risk of a flare.
Adjusting Your Asthma Medications and Plan for Winter
Prevention isn't only about scarves and humidifiers. Your medication plan matters in the cold months.
- Stick with your controller: Taking your daily preventer inhaler as your doctor prescribed helps keep airway inflammation low and can make you less reactive to cold air.
- Pre-treat before cold or exercise: Your doctor might recommend using your quick-relief inhaler about 10 to 15 minutes before going outside or working out in the cold.
- Carry your reliever everywhere: Keep your rescue inhaler with you and store it warm in an inside pocket. Extreme cold can affect performance.
- Update your Asthma Action Plan: Review it each fall. Make sure it includes clear steps for cold-induced symptoms and for exercise days.
- Be ready on the go: A portable mesh nebulizer can deliver medication quietly and anywhere if your doctor recommends nebulizer treatments.
- For thick winter mucus: Some doctors use nebulized hypertonic saline (3 percent or 7 percent) to help loosen mucus. Only use this if your doctor recommends it.
- Protect your meds: Don't let inhalers or neb solutions freeze. Avoid leaving them in the car overnight.
⚠️ If you have severe trouble breathing, chest tightness that doesn't improve after using your rescue inhaler, blue lips or fingernails, or you can't speak in full sentences, seek emergency medical care right away.
Talk to your doctor if your asthma gets worse each winter, you're using your rescue inhaler more than usual, or your current plan isn't controlling symptoms.
Key takeaway: Plan ahead, follow your doctor's winter plan, and keep your rescue tools ready.
Staying Healthy to Prevent Winter Asthma Attacks
Here's how to prevent asthma attacks in winter at home and outside. Cold isn't the only winter trigger. Keep your whole environment asthma-friendly.
Avoid winter illnesses:
- Get your annual flu shot if your doctor recommends it.
- Wash your hands regularly and give yourself space from people who are sick.
- In crowded indoor spaces during peak illness season, a mask can help reduce exposure.
Tidy up indoor air:
- Dust and vacuum regularly. Wash bedding weekly in hot water. Use allergen-proof covers if dust mites are a problem.
- Keep humidity around 40 to 50 percent and clean humidifiers to prevent mold.
- Reduce pet dander if it triggers your asthma: keep pets out of bedrooms, brush them regularly, and use a HEPA filter or vacuum.
- Be cautious with fireplaces, strong candles, or sprays that can irritate airways. Ventilate well.
- Keep indoor temperature comfortable, not overheated, and crack a window briefly on milder days to refresh air.
Exercising with Asthma in Cold Weather
- Warm up indoors for 5 to 10 minutes before activity.
- Shift workouts indoors on very cold or windy days, or schedule outdoor activity during the warmest part of the afternoon.
- Wear a face covering and breathable layers. If your doctor has told you to use your inhaler before exercise, do that before heading out in the cold.
- Keep your inhaler on you and warm. If symptoms start, pause and get to warm air.
- This pattern is called exercise-induced bronchoconstriction (EIB), a type of asthma that shows up as wheezing or coughing during or after exercise, especially in cold air.
Healthy habits help too: stay hydrated, eat well, sleep enough, and manage stress. Small wins add up and reduce the odds of a flare.
Bottom line: Avoid winter germs and indoor irritants, and adjust workouts to protect your breathing.
Helping Children Manage Asthma in Cold Weather
Kids don't always say they can't breathe right away. Watch for coughing, slowing down during play, or saying their chest feels funny.
Make cold air kid-friendly:
- Bundle up and cover the face: A fun scarf or neck gaiter makes wearing it easier.
- Pre-treat before recess, PE, or winter sports if your child's doctor recommends it. Younger children usually do best with an inhaler plus spacer when their doctor prescribes it.
- Have a plan at school: Share the child's Asthma Action Plan with the school nurse and teachers. Keep an inhaler at school, not in a freezing locker. Give permission for breaks when it's very cold.
- Keep outings short on frigid days and choose indoor activities when needed.
- For little ones who already use nebulizers as prescribed, a portable nebulizer like TruNeb can make treatments easier in the car or right after coming indoors.
⚠️ Seek urgent care if a child is struggling to breathe, ribs are pulling in, lips or nails look blue, or they can't speak in full sentences.
Key takeaway: Plan ahead and make cold air kid-friendly with face coverings, a clear school plan, and treatment steps your child's doctor recommends.
Frequently Asked Questions About Asthma and Cold Weather
Here are quick answers to common questions about asthma and cold weather.
Tap or click a question below to see the answer:
Yes. Cold, dry air can irritate and narrow your airways, leading to coughing, wheezing, and shortness of breath.
Cold, dry air plus more viruses and dry indoor air create a strong combination of triggers for symptoms.
There isn't a single number for everyone, but many people notice more symptoms near freezing and below, especially with wind and low humidity. Take precautions and limit exposure once you learn your personal threshold.
Both can be triggers. Cold, dry air tends to cause bronchospasm quickly. Hot, humid days can also bother some people, especially when pollen or pollution is high. Know your pattern and plan ahead.
Cover your nose and mouth, breathe through your nose, use a humidifier indoors, your doctor might suggest using your inhaler before heading out or exercising in the cold, carry your rescue inhaler, and avoid winter germs and dusty, dry indoor air.
Usually helpful. Aim for about 40 to 50 percent humidity and keep the unit clean to avoid mold and dust mites.
Disclaimer: This article is for informational purposes only and isn't a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options.







