On this page
How Asthma Affects Breathing (and Why Techniques Can Help)
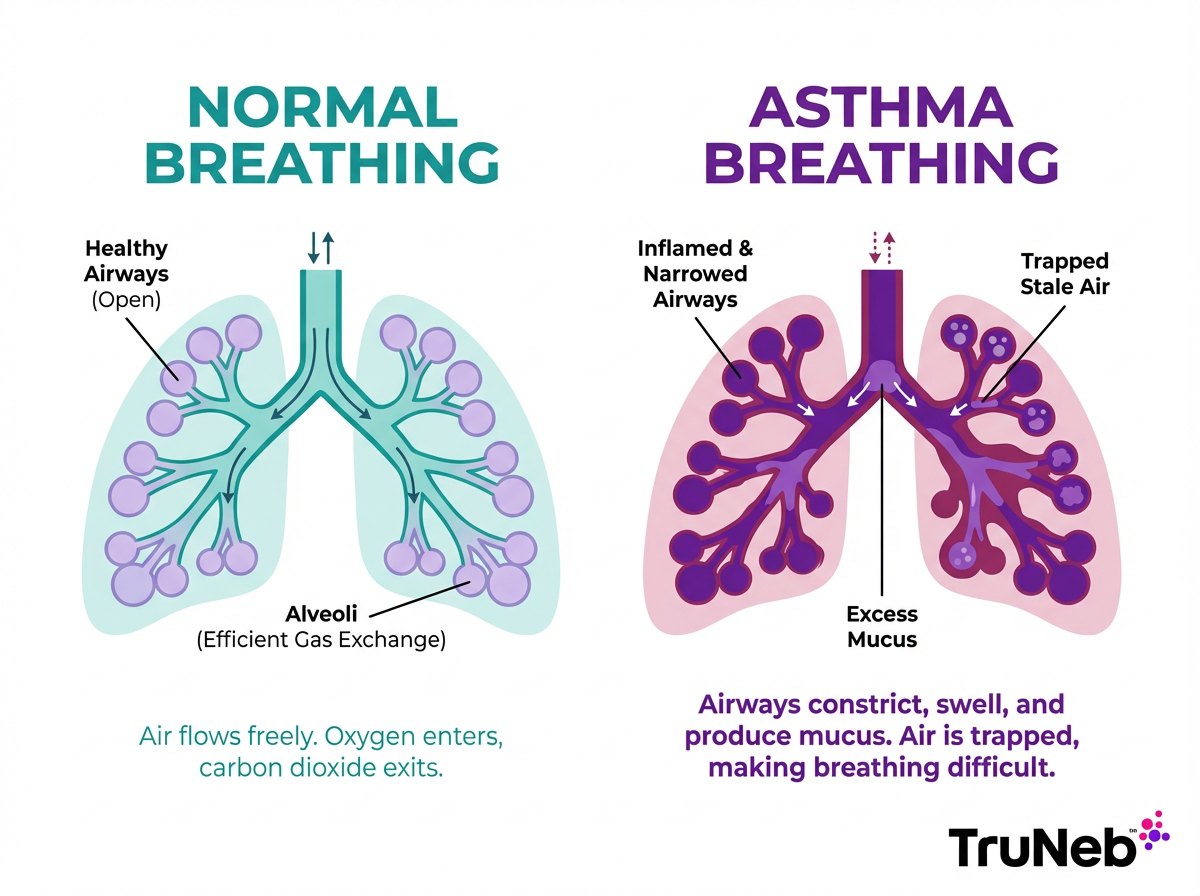
Asthma narrows and irritates your airways. That makes it hard for air to move in and out. Old, stale air can get trapped, so fresh air has less room. This can feel like shortness of breath and chest tightness.
When that happens, you can start breathing fast from your upper chest. Panic can creep in, which tightens your breathing even more.
Breathing techniques for asthma train your body to slow down and use your diaphragm, the big muscle under your lungs. That helps air move more smoothly. These skills also calm your nervous system, which can cut the spiral of stress and shortness of breath.
Think of this like physical therapy for your breathing. You still use your asthma medicines. These exercises are an add-on, not a replacement.
Takeaway: Asthma can trap stale air; simple drills retrain your diaphragm so fresh air moves more easily.
Benefits of Breathing Exercises for Asthma Management
- Improved air exchange: better emptying of stale air leaves more room for fresh air.
- Stronger breathing muscles: training your diaphragm makes each breath more efficient.
- Less hyperventilation: slow, steady breathing prevents the dizzy, panicky feeling of over-breathing.
- Relaxation: calm breathing helps ease stress-triggered symptoms.
- Better day-to-day control: adults who practice breathing exercises often report modest quality-of-life gains. A 2020 review in adults with asthma found modest improvements in quality-of-life scores.
Reminder: these exercises support your care. They don't replace your controller or rescue medicines.
Takeaway: Breathing practice can improve comfort and control, but it works alongside your meds.
Getting Started: Overview and Why You Should Not Replace Your Inhaler
Start when you are calm and comfortable. Sit upright or lie down. Wear loose clothing. Aim for about 5 to 10 minutes once or twice a day.
Keep using your prescribed controller and rescue medicines. Breathing exercises help, but they don't open inflamed airways as fast as a rescue inhaler.
If your chest feels tight, follow the steps in your Asthma Action Plan, which usually include using your rescue inhaler or sometimes a nebulizer as your doctor has instructed. As the medicine starts to work, use slow breathing to settle your rhythm.
Practice tips:
- Learn the pattern while you feel well, so it's easy to use under stress.
- Breathe in through your nose whenever you can.
- If your nose is blocked, clear it first.
Most research on breathing exercises is in adults, so this guide is focused on adult asthma unless your doctor suggests otherwise.
Takeaway: Learn the patterns when you are calm, and keep your rescue inhaler or nebulizer as first-line relief.
Diaphragmatic Breathing: The Belly Breathing Technique
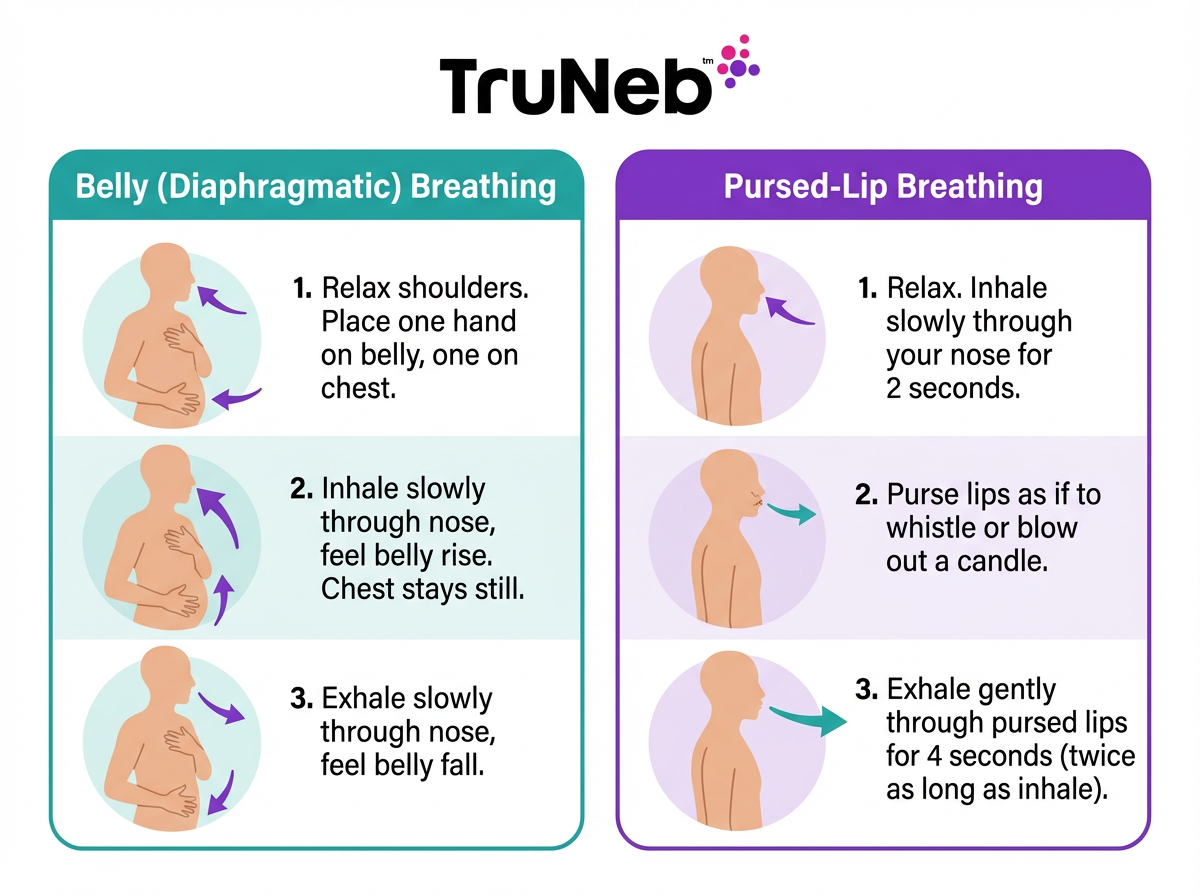
Diaphragmatic breathing teaches you to use your belly, not your upper chest. It's also called a deep breathing exercise for asthma. It helps you fill the lower parts of your lungs and slow your pace.
How to do it:
- Get comfortable. Lie on your back with a pillow under your knees, or sit upright.
- Place one hand on your chest and one on your belly.
- Inhale slowly through your nose. Feel your belly rise under your hand. Keep chest movement small.
- Exhale gently through pursed lips or your nose. Feel your belly fall.
- Try an easy rhythm like inhale for 2 counts, exhale for 4 counts.
- Repeat for several minutes. Keep your shoulders relaxed.
Tips: If it helps, rest a light object on your belly and watch it rise and fall. If you feel lightheaded, pause and breathe normally, then restart more gently. If dizziness keeps happening, stop and talk with your doctor.
Takeaway: Belly up on inhale and belly down on exhale is the core pattern.
Pursed-Lip Breathing: Exhale to Slow Down
Pursed-lip breathing helps you breathe out longer and prevent air trapping. It also lowers your breathing rate, which eases the feeling of breathlessness.
Steps:
- Inhale slowly through your nose.
- Purse your lips like you're gently blowing out a candle.
- Exhale softly through your pursed lips for about twice as long as you inhaled. For example, in for 2, out for 4.
- Don't force the air. Let it flow out.
- Repeat for several breaths until your breathing settles.
People often use this when they feel short of breath, like after climbing stairs or while they wait for their rescue medicine to work, as long as they've already followed their Asthma Action Plan. This technique is also taught in pulmonary rehab for asthma and COPD.
Takeaway: In through your nose, out through gently pursed lips for twice as long.
Buteyko Breathing Method: Controlled Breathing
The Buteyko method was developed to reduce over-breathing. It teaches slower, gentler breaths and brief, safe breath holds to help reset your breathing drive.
Try the control pause:
- Inhale through your nose normally.
- Exhale normally.
- Pinch your nose and hold your breath until you feel a clear urge to breathe. Don't push into dizziness.
- Release and inhale calmly through your nose.
- Breathe gently for about 10 seconds, then repeat.
Over time, your comfortable hold time can increase, which suggests your body is getting more used to the breathing pattern. Most programs also focus on nose breathing and relaxation. Evidence is mixed but suggests symptom and quality-of-life benefits in some adults, and results vary. It's usually learned with a trained instructor or therapist.
Caution: Practice seated. Stop if you feel unwell. If you have heart or other medical problems, talk to your doctor before adding breath-holding work.
Takeaway: Buteyko slows over-breathing with brief, safe breath holds to steady your rhythm.
Papworth Method: Breathing and Relaxation
The Papworth method blends nose-and-belly breathing with relaxation training. It was developed to help people with asthma breathe more efficiently and stay calmer during daily tasks.
A simple routine:
- Sit comfortably. Relax your neck and shoulders.
- Breathe in gently through your nose using your belly. Count to 4.
- Breathe out softly through your nose or pursed lips. Count to 6.
- Keep your chest and shoulders relaxed. Let your belly do the work.
Practice for 5 to 10 minutes. This method was originally developed at Papworth Hospital in the UK for people with asthma. It's typically taught by a physiotherapist or a respiratory therapist, then practiced at home.
Takeaway: Papworth pairs diaphragmatic nose breathing with relaxation to ease symptoms.
Yoga Breathing Exercises: Pranayama for Asthma
Gentle yoga breathing can build control and reduce stress. It focuses on nasal breathing and steady rhythms.
Two options to try:
- Alternate Nostril Breathing: Sit comfortably. Close your right nostril with your thumb. Inhale through your left nostril. Close left with your ring finger, open right, and exhale through right. Inhale through right, switch, and exhale through left. Continue gently.
- Equal Breathing: Inhale for a count of 4 and exhale for a count of 4 through your nose. Keep it easy and smooth.
Go slowly and stop if you feel uncomfortable. Always have your rescue inhaler nearby when trying new breathing practices.
Studies suggest yoga breathing can modestly improve asthma symptoms and quality of life in some adults, but it's considered an add-on therapy based on small studies. It doesn't replace medical treatment.
Takeaway: Gentle pranayama builds calm and steady nose breathing as a complement to your care.
Huff Cough and Airway Clearance Techniques
If mucus is part of your asthma picture, clearing it can make breathing easier. The huff cough moves mucus up without harsh coughing. This is most helpful when mucus builds up, like during colds or mucus-heavy asthma.
How to do a huff cough:
- Take a medium breath in.
- Hold for 2 to 3 seconds.
- With your mouth open, exhale firmly as if fogging a mirror and say "ha". That is the huff.
- Repeat 2 to 3 huffs, then cough to clear mucus.
Positions like sitting and leaning forward or lying on your side propped up can also help you recover your breath.
Some people use a bronchodilator or doctor-prescribed 3% or 7% hypertonic saline before airway clearance to loosen mucus, only when their doctor has recommended this as part of their plan. Then huff cough to bring it up. Safety note: Talk to your doctor before trying a new medication.
Takeaway: Huff like you're fogging a mirror to move mucus up, then cough it out.
Integrating Breathing Techniques Into Your Asthma Action Plan
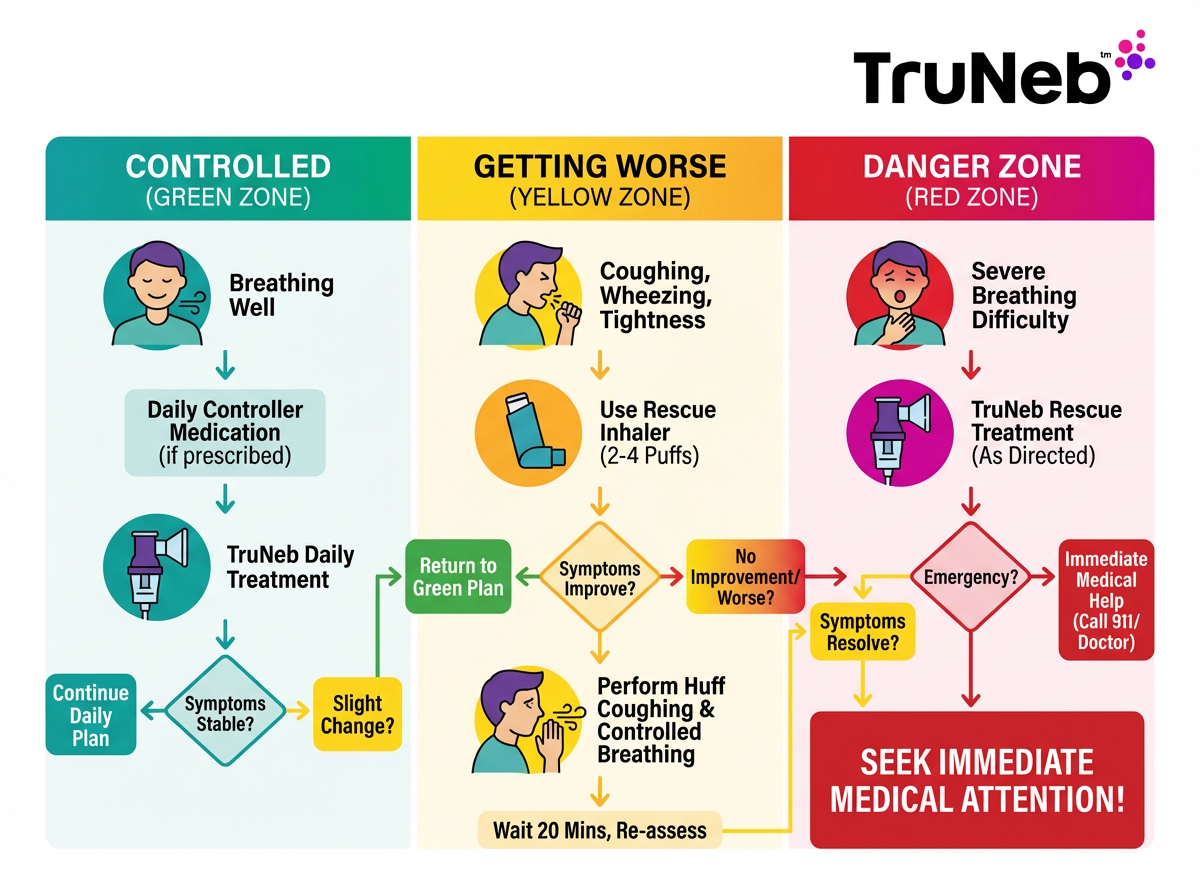
Make breathing practice part of your plan.
Green Zone: When you feel well, practice 5 minutes of belly breathing daily. Add a few cycles of pursed-lip exhales. This builds skill and confidence.
Yellow Zone: At the first sign of tightness, follow your plan. Use your rescue inhaler or nebulizer as prescribed. While you wait for relief, breathe in through your nose and out through pursed lips to slow your rate and help prevent air trapping.
Flares: These techniques support you, but they are not rescue care. Use your medicines first and get help if symptoms are severe. ⚠️ If you have severe symptoms like trouble speaking, ribs pulling in, feeling very breathless at rest, or blue lips or face, use your emergency medicines and seek emergency medical care right away (call 911 or your local emergency number).
On the go: A portable nebulizer can deliver your bronchodilator quietly at home, work, or travel. Don't confuse a nebulizer (which delivers prescription medicine as a mist you breathe in) with a steam inhaler. Steam inhalers aren't meant for asthma medications. A lot of adults treat first, then use calm breathing to steady their rhythm. If mucus is an issue, your doctor might prescribe hypertonic saline for nebulizing, followed by huff cough to clear.
Review: Ask your doctor or asthma educator to check your technique and update your plan.
Takeaway: Use medicine first, then breathing to calm and clear, and write these steps into your plan.
Tips for Success and Precautions
- Practice daily. Short, steady practice beats long, rare sessions.
- Tie it to a routine, like after brushing your teeth or before bed.
- Avoid practicing in dusty or smoky spaces.
- Stop if you feel lightheaded and restart more gently.
- In a severe flare, focus on medicines and getting help. Use breathing to support you, not as rescue care.
- ⚠️ If you have severe symptoms like trouble speaking, ribs pulling in, feeling very breathless at rest, or blue lips or face, use your emergency medicines and seek emergency medical care right away (call 911 or your local emergency number).
- Ask your doctor or a respiratory therapist to watch your technique and personalize it.
Takeaway: Short daily practice in a calm setting builds real breathing control.
FAQs: Breathing Techniques and Asthma
Tap or click a question below to see the answer. These quick answers cover common questions about how breathing exercises fit into asthma treatment, safety, and everyday use.
Yes. They can improve breathing comfort and control when used with your usual treatment. Most of the research is in adults, and a 2020 review found modest improvements in quality-of-life scores. They don't cure asthma and shouldn't replace your medicines.
There's no single best technique. Most adults start with diaphragmatic (belly) breathing and pursed-lip breathing because they're simple and effective. Methods like Buteyko or Papworth can add more tools after you learn the basics.
Practice once or twice daily for 5 to 10 minutes when you're calm. Regular practice trains your body so the patterns feel natural during stress.
No. Keep taking your controller meds and carry your rescue inhaler. Breathing exercises are a complement, not a replacement. Use your medicine first during symptoms, then use breathing to settle your rhythm.
If symptoms are severe, follow your emergency plan and use your rescue medicine right away. While you wait for relief, pursed-lip breathing can help you slow your breathing and feel more in control after you've used your medicine. ⚠️ If your symptoms are severe or not improving after using your rescue medicine, call 911 (or your local emergency number) or seek urgent medical care.
Evidence is limited for children. Older kids and teens can benefit with guidance, but they should never delay their inhaler. If interested, ask your pediatrician or a respiratory therapist for age-appropriate instruction. Most studies are in adults.
Slow down and take smaller breaths. Don't force your lungs to empty. Sit, rest, and try again gently. If dizziness continues, stop and talk with your doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, asthma action plan, and any treatments or breathing exercises you want to try.







