On this page

What Is an Asthma Attack During Pregnancy?
An asthma attack is a sudden flare where your airways tighten, swell, and make extra mucus.
Pregnancy doesn't cause asthma, but symptoms can change. Some people improve, some stay the same, and some get worse. Asthma affects a noticeable share of pregnancies, and a lot of pregnant people with asthma have at least one flare-up.
For most people, normal pregnancy breathlessness is mild and usually eases with rest. An asthma attack usually brings wheezing, chest tightness, coughing, or trouble speaking. If those show up and don't fade, follow your asthma action plan and contact your doctor.
Quick treatment keeps oxygen flowing to you and your baby.
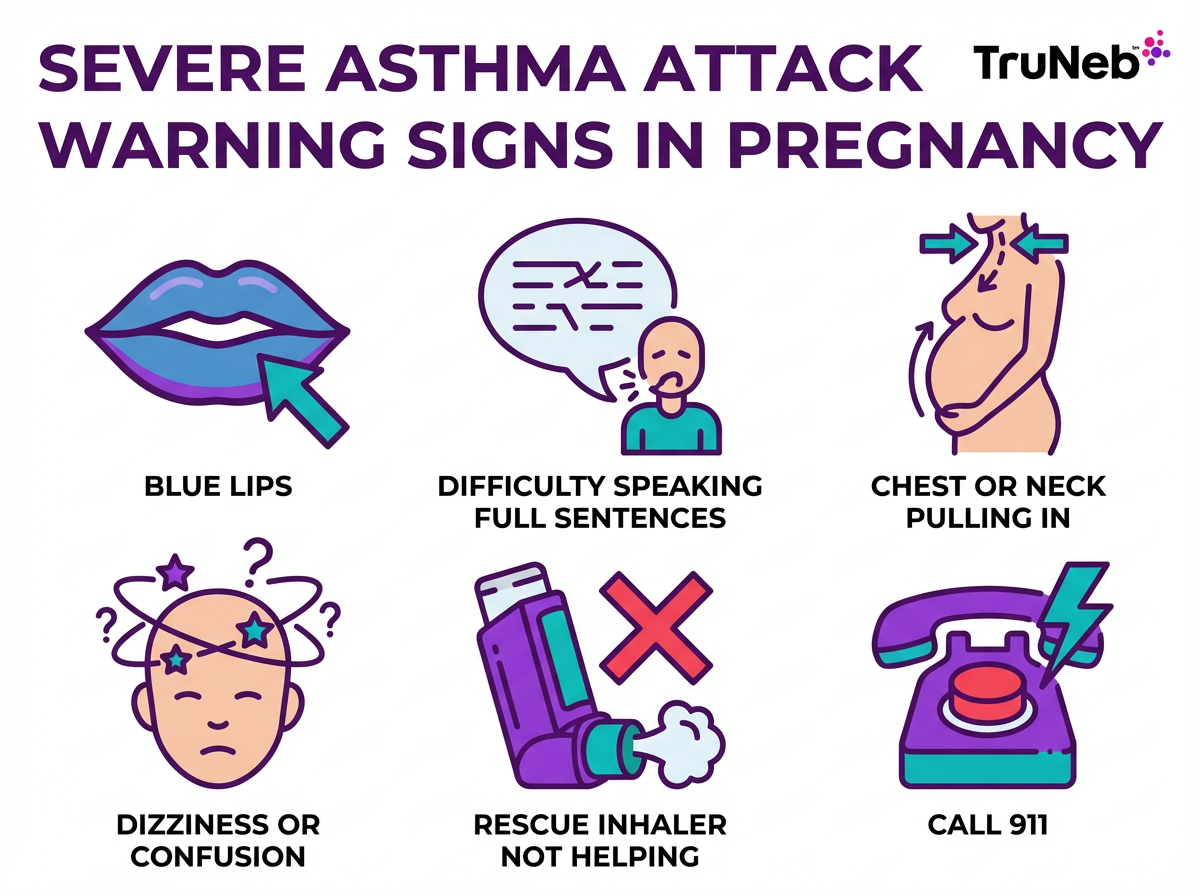
Signs of a Severe Asthma Attack and When to Seek Emergency Care
A severe asthma attack in pregnancy is an emergency if you can't speak in full sentences, your lips or fingers look blue, or your rescue inhaler isn't helping.
⚠️ If any of these symptoms appear, call 911 (or your local emergency number) right away. Severe asthma in pregnancy is an emergency for both you and your baby.
- Too breathless to speak full sentences
- Blue or gray lips or fingernails
- Skin pulling in at the neck or ribs with each breath
- Feeling faint, confused, or very sleepy
- Little or no relief after repeated rescue puffs
- You don't have your inhaler and symptoms are getting worse
- In late pregnancy, much less fetal movement during the episode
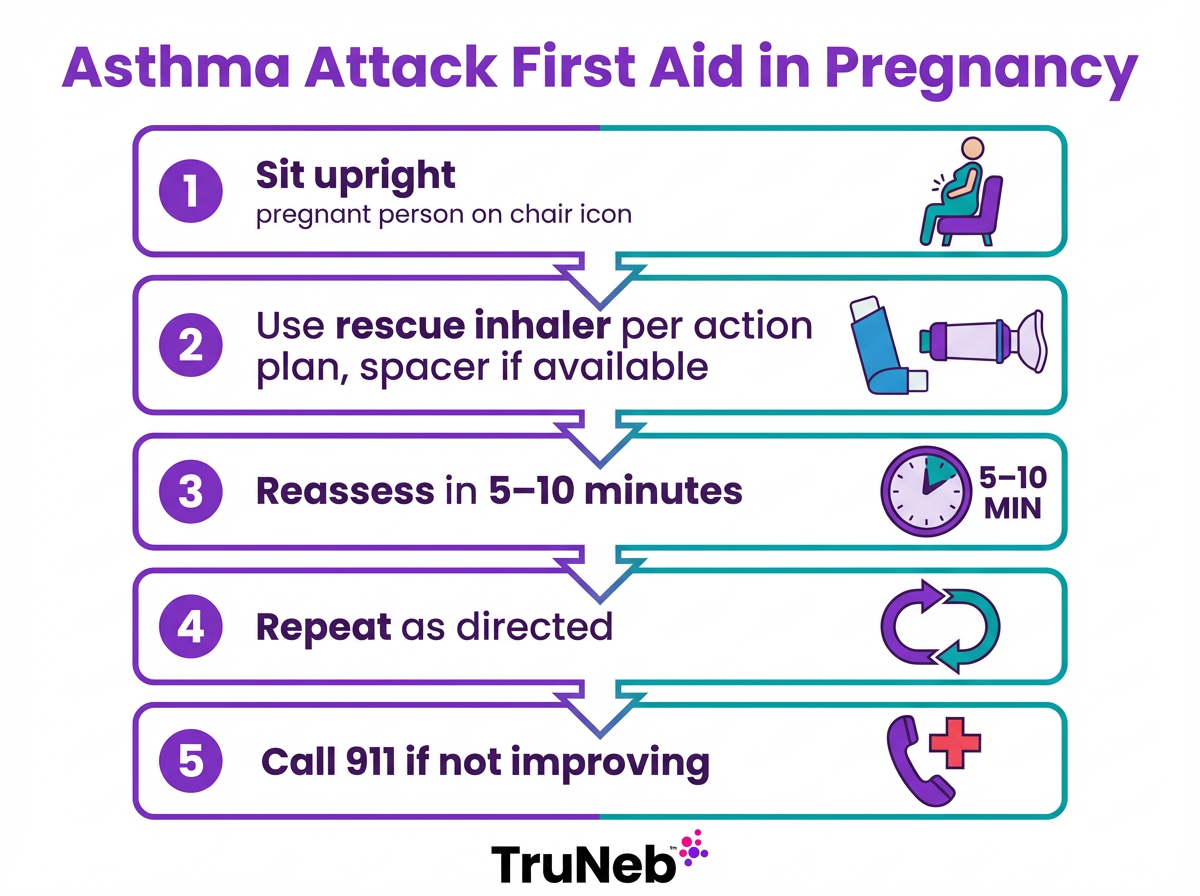
What to Do During an Asthma Attack While Pregnant (Step-by-Step)
Here is a calm, clear plan to follow right away.
During an asthma attack in pregnancy, focus on using your reliever medicine as directed, staying upright, and getting emergency help if symptoms don't ease quickly.
- Stop and sit upright. Loosen tight clothing. Sitting helps your lungs open more than lying down.
- Use your rescue inhaler now, following the dose in your asthma action plan (often 2 puffs with a spacer if you have one). Inhale slowly and deeply with each puff.
- Focus on slow, steady breathing. Inhale through your nose for 2 seconds, then exhale through pursed lips for 4 seconds.
- Move away from triggers. Leave smoky, dusty, or very cold air if you can.
- Ask for help. Tell someone nearby you are having an asthma attack.
- Reassess after 5–10 minutes. If you feel better, rest and call your doctor the same day to report the episode. If not better, repeat your reliever dose as directed in your plan.
- Use a nebulizer if your doctor advised one for home use. A portable mesh device like the TruNeb™ portable mesh nebulizer can deliver your prescribed medicine as a fine mist at home or on the go. Use only as prescribed.
- Call emergency services if you aren't improving quickly or if symptoms worsen at any point. Paramedics can give oxygen and additional treatments on the way.
⚠️ Don't wait if you're getting worse or feel scared you can't breathe—call emergency services.
Note: Some national asthma guidelines for adults allow up to 10 puffs of a reliever inhaler in a severe attack while you wait for emergency help, but always follow your own asthma action plan and your doctor's advice rather than changing your dose on your own.
If a bad attack happens in late pregnancy, your OB might want to check on the baby once you're stable.
Can an Asthma Attack While Pregnant Harm the Baby?
Uncontrolled or long attacks can lower the oxygen you and your baby receive.
Severe or frequent flare-ups are linked with higher chances of preterm birth, low birth weight, and preeclampsia. Treating a flare quickly protects your baby.
Experts stress an important point: unmanaged asthma is riskier to the fetus than standard asthma medicines. After a bad flare, your OB might check the baby’s well-being, but most moms and babies do well once breathing is under control.
Preventing Asthma Attacks During Pregnancy
Prevention is the goal. Good day-to-day control of your asthma is the best way to avoid dangerous flare-ups during pregnancy.
Focus on three things: avoid your triggers, take your medicines as prescribed, and follow a simple written action plan with your doctor.
The next sections cover everyday habits, safe medication use, and planning with your doctor.
Avoiding Common Triggers and Irritants
Cut exposure to the things that set off your asthma:
- Allergens: Use dust-mite covers, wash bedding hot weekly, run a HEPA filter, and keep windows closed on high-pollen days.
- Smoke: Don't smoke. Keep your home and car smoke-free. Avoid secondhand smoke.
- Strong odors and chemicals: Ventilate well. Choose unscented cleaners. Let someone else handle harsh fumes.
- Cold air: Cover your nose and mouth with a scarf in cold weather.
- Exercise: Stay active, but warm up and use your pre-exercise inhaler if prescribed. Keep your reliever with you.
- Illness: Ask your doctor about getting a flu shot and staying up to date on any vaccines they recommend for you during pregnancy. Wash hands frequently and avoid close contact with people who are sick.
- Heartburn and congestion: Pregnancy GERD and nasal stuffiness can worsen asthma. Eat smaller meals, avoid lying down after eating, and ask your doctor about safe options to manage reflux and congestion.
⚠️ If you see products labeled 'steam inhaler,' don't use them to take asthma medicine. They're not the same as nebulizers and aren't meant for breathing medications.
Limiting contact with the triggers that set off your asthma can sharply cut your risk of an attack while you're pregnant.
Taking Asthma Medications Safely: Don’t Skip Your Inhalers
Most standard asthma medicines are considered safe in pregnancy, and keeping asthma controlled protects your baby.
- Controller medicine: Keep taking your daily inhaled corticosteroid if prescribed. Budesonide has a strong safety record in pregnancy. Don't stop unless your doctor tells you to.
- Rescue medicine: Quick-relief inhalers like albuterol are typically used when asthma symptoms start and act fast in the lungs. If you find you need your rescue inhaler more than twice a week, let your doctor know—this can be a sign your asthma isn’t well controlled.
- Short steroid courses: If a severe flare needs oral steroids, short courses are generally considered safe when needed and can be lifesaving for you. In serious attacks, the benefits usually outweigh the risks.
- Avoid self-medicating: Don't start over-the-counter cough or decongestant medicines without checking with your doctor.
Some research shows babies of moms who used prescribed inhaled steroids had better lung function at birth than those whose moms left asthma untreated.
Safety Note: Talk to your doctor before trying a new medication.
Working with Your Doctor and Creating an Asthma Action Plan
Loop in your OB/GYN and asthma specialist early and build a simple, written plan.
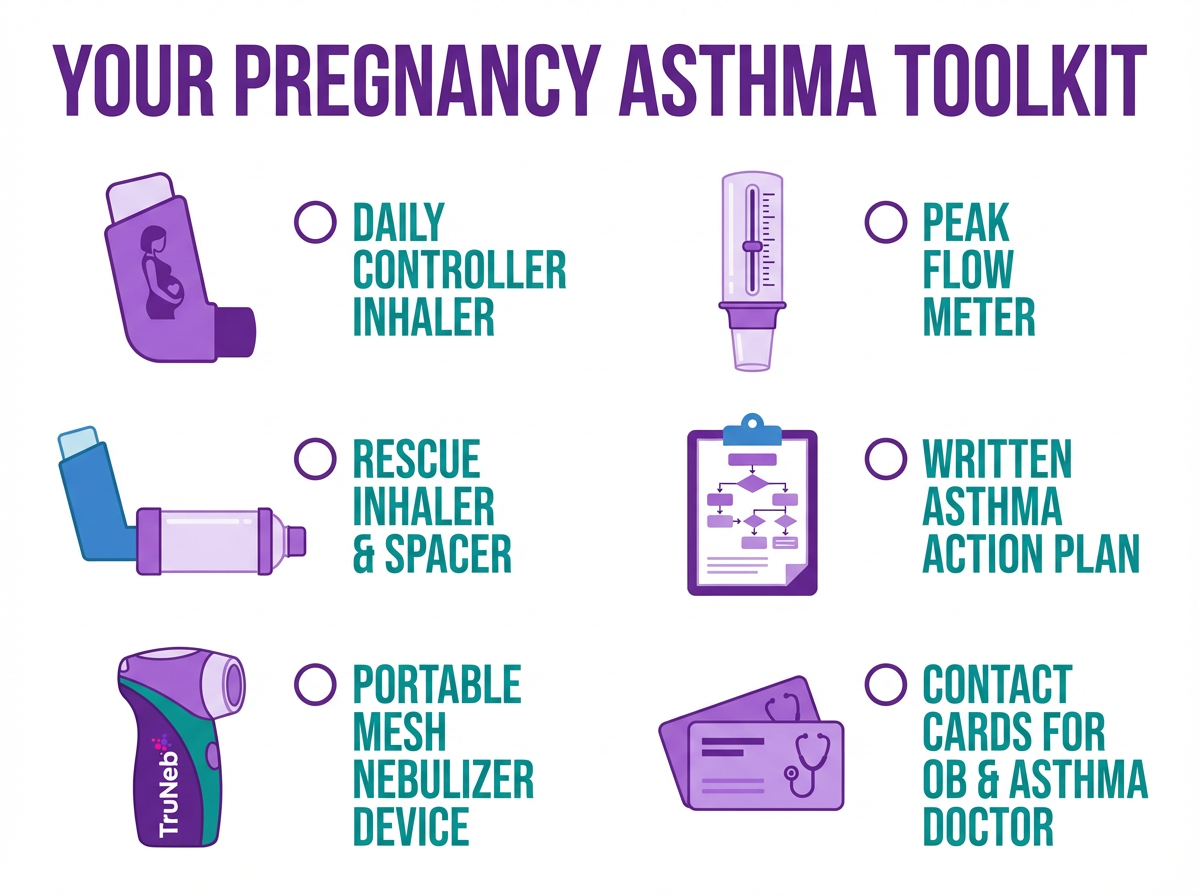
- Personalized plan: Your Asthma Action Plan lists daily meds, early warning signs, when to step up treatment, and when to call your doctor or go to the ER. Most plans use green, yellow, and red zones to show what to do as symptoms change. Keep a copy with you and share it with your partner or family.
- Monitor closely: Your doctor might ask you to track symptoms or use a peak flow meter. A drop can warn of trouble before you feel it.
- Plan for labor and after: Bring your medicines to the hospital and ask your care team how they want you to use your inhalers during labor and after delivery. In most cases, you'll keep using them as usual.
- Tools that help: Ask if you should keep a nebulizer at home as backup. A portable device like the TruNeb Portable Mesh Nebulizer can make it easier to take a prescribed treatment away from home. For thick mucus, some specialists use medical-grade hypertonic saline (3% or 7%) by nebulizer under guidance. Use these only if your doctor recommends them. Don't start hypertonic saline on your own—this should only be part of a plan you and your doctor agree on.
A simple written asthma action plan with your doctors gives you clear steps for everyday control and for what to do if symptoms suddenly get worse.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Don't stop any asthma medicine without your doctor's guidance. Most inhalers, including albuterol and inhaled steroids, are considered safe and necessary in pregnancy. Unmanaged asthma poses more risk to the fetus than standard asthma treatment. If your doctor prefers a specific inhaler with more safety data (like budesonide), they will guide that change. Keep taking your prescribed regimen to stay controlled.
It depends. About one third get worse, one third improve, and one third stay the same. If asthma does worsen, it usually happens in the late second to third trimester and can be managed by adjusting treatment. Most people return to their pre-pregnancy baseline within a few months after delivery.
For most people, normal pregnancy breathlessness is mild and tends to ease with rest. Asthma trouble brings wheeze, chest tightness, cough, or waking at night, and it typically improves after you use a rescue inhaler. If you're unsure, follow your asthma action plan and call your doctor.
Asthma attacks are uncommon during labor. You'll usually keep using your inhalers on schedule—your nurses and doctors will tell you exactly what to do. Hospitals can give oxygen or nebulized medicine if needed. Good pain control can help prevent stress-triggered symptoms. Most people breathe well through labor with standard care.
Yes. Common asthma medicines transfer into breast milk in tiny amounts and aren't known to harm infants based on current evidence. Keeping your asthma controlled helps you care for your baby. If you need a short steroid course or another strong medicine, tell your pediatrician; most are still compatible with breastfeeding.
Having a parent with asthma raises a child's risk, but it doesn't mean they'll have it. You can lower environmental risks by keeping a smoke-free home, reducing dust and allergens, and breastfeeding if possible. If your child ever shows symptoms, early pediatric care keeps them active and well.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, medications, and any questions you have about asthma and pregnancy.







