On this page
Step 1: Why an Asthma Action Plan for School Is Essential
Every student with asthma needs a written action plan at school so adults know exactly what to do every day and in an emergency.
What it is:
- A doctor-approved set of instructions for daily care and emergency steps.
Why it matters at school:
- Staff can follow specific steps right away when coughing, wheezing, or shortness of breath shows up.
- Less confusion, faster care, fewer emergencies.
The bigger picture:
- National groups like the CDC and AAFA emphasize written plans for everyone with asthma.
- Asthma leads to many missed school days; good planning helps kids stay in class.
What your plan will include:
- Color zones (Green, Yellow, Red)
- Medicines and doses
- Triggers to avoid
- When to call parents or 911
Step 2: Get the Right Asthma Action Plan Form
Bring a trusted, zone-based action plan form to your child’s doctor so you leave with a signed plan the school can follow.
Where to get it:
- Ask your pediatrician or allergist for their preferred form.
- Download a standard form from a trusted group.
- Check your school or state health website for a school-ready version, because some districts require you to use their specific form.
What to look for on the form:
- Green, Yellow, and Red zones
- Sections for medicines, triggers, and emergency contacts
- Signature lines for your doctor and you (schools need these to give medicine)
Quick tip:
- Print two copies (or keep a clean digital file) so updates are easy at the start of each school year.
Step 3: Fill the Plan With Your Doctor
Use the traffic light system: Green is daily care, Yellow is act early, Red is emergency.
Book a visit to complete the plan with your child’s doctor, ideally before school starts or after any big change in symptoms or medicines.
Green Zone (doing well):
- No symptoms; normal play and sleep.
- Lists daily controller medicines (name, dose, when to take).
- Can include your child’s personal-best peak flow number.
Yellow Zone (getting worse):
- Cough, wheeze, tight chest, trouble keeping up, or peak flow around 50–79%.
- Clear steps like: use the rescue inhaler (how many puffs and how often), recheck, and when to call the nurse or parents.
Red Zone (emergency):
- Hard to breathe, can’t speak full sentences, ribs pulling in, lips turning blue, or peak flow under 50%.
- Immediate rescue medicine and clear instructions on when to call 911 and parents.
Also include:
- Triggers to avoid (for teachers to help prevent flares).
- Emergency contacts and your doctor’s number.
- Signatures from the doctor and parent/guardian so the school can follow the plan.
Your child’s doctor should fill in the Green, Yellow, and Red zones so the plan spells out exactly which medicines to use and when to get emergency help.

Step 4: Share the Plan and Medicines With the School
Put a signed plan and the right medicines in the nurse’s hands before day one.
Make copies and deliver them:
- Give the signed plan to the school nurse, your child’s teachers, and any coaches or after-care staff.
- Keep a copy in your child’s backpack and one at home.
Meet to review:
- Ask for a short meeting with the nurse and teacher to walk through key parts of the plan.
- Point out your child’s triggers and what early symptoms look like for them.
Medicines and devices at school:
- Provide a labeled rescue inhaler and a spacer (a backup inhaler often stays in the nurse’s office).
- If your child needs nebulized medicine at school, a quiet, portable mesh nebulizer like the TruNeb™ portable mesh nebulizer can help the nurse fit treatments into the school day and on field trips.
- Make sure any nebulizer use at school is written into the signed plan and approved by the school.
- In some cases, a specialist may include 3% or 7% hypertonic saline for thick mucus; the nurse should give this only as written in the plan.
- If you see products labeled “steam inhaler”, know these are not for breathing asthma medications - prescription asthma medicines need a nebulizer device your doctor recommends.
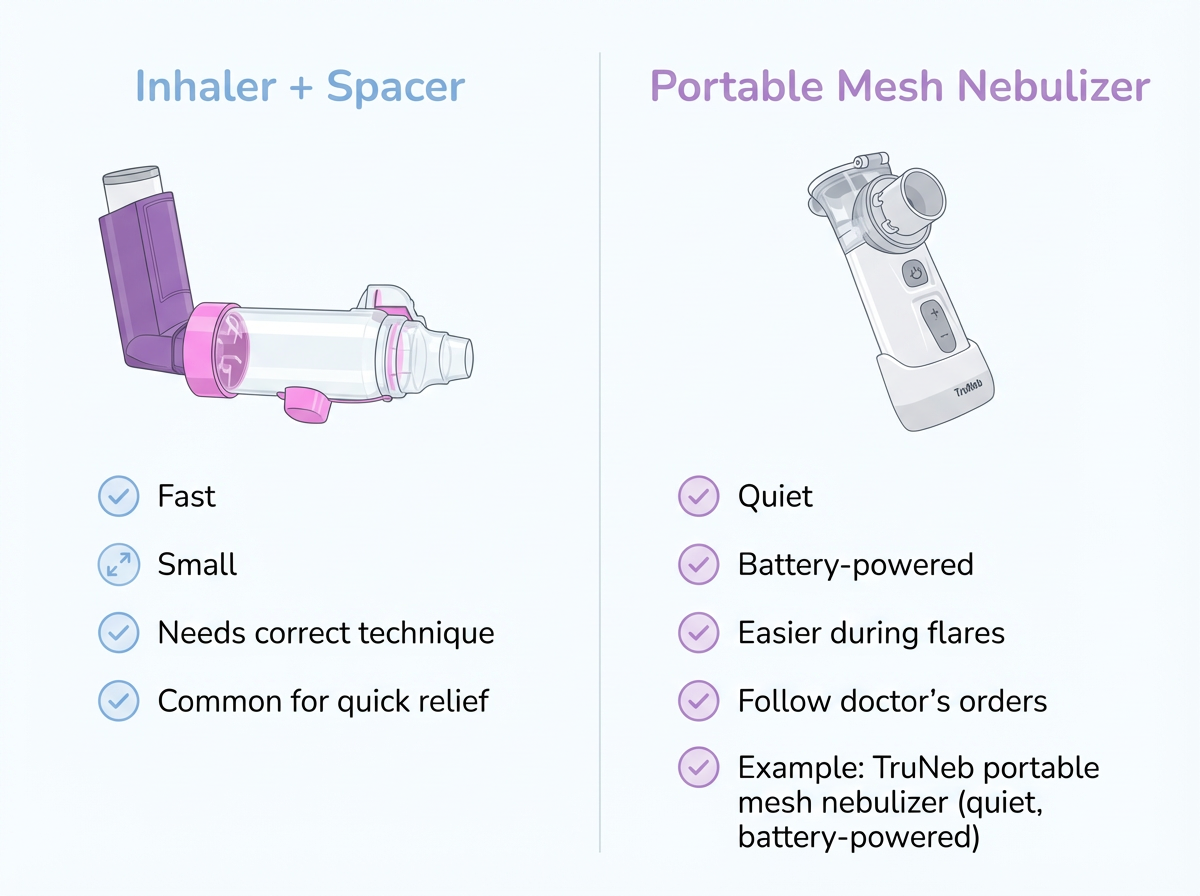
Device comparison for school use — key takeaway: inhalers with spacers and nebulizers both deliver prescription asthma medicine; use what the doctor writes in the student’s plan and what the school approves.
| Device | Speed | Noise | Portability | Technique help | School fit |
|---|---|---|---|---|---|
| Inhaler + spacer | Fast (seconds) | Low | Pocket-size | Spacer helps get more medicine into lungs | Common for quick relief per plan |
| Portable mesh nebulizer (example: TruNeb) | Moderate (minutes) | Very quiet | Handheld, battery-powered | No strong inhale needed | Good when flares make inhaler technique hard; follow plan and policy |
| Tabletop nebulizer | Moderate (minutes) | Low–moderate | Needs outlet, less portable | No strong inhale needed | Usually used in nurse’s office; depends on doctor’s order |
Note: Always check medication compatibility and cleaning steps with your child’s doctor and the school nurse.
Paperwork:
- Some districts require a medication authorization form in addition to the action plan; ask the nurse what’s needed.
Safety note: Talk to your doctor before trying a new medication or adding a nebulized treatment at school.
Step 5: Teach Staff and Your Child What to Do
A two-minute walk-through now prevents panic later.
Help adults feel ready:
- Show the teacher and nurse how your child uses the inhaler with a spacer.
- If a nebulizer will be used, demonstrate how it fits and runs so staff remember.
- Offer a one-page cheat sheet for the classroom or substitute teacher folder with your child’s triggers and Red Zone steps. Make sure the cheat sheet matches the doctor-signed plan; don’t add new instructions.
Try an "asthma drill":
- Talk through what happens if symptoms start in class or on the playground (a quick practice conversation so everyone knows the steps).
Empower your child:
- Practice at home: “I need my inhaler” or “Please call the nurse.”
- Older kids should know what each color zone means and where their medicine is.
Walking teachers and the school nurse through your child’s asthma plan ahead of time makes real emergencies calmer and safer for everyone.
Step 6: Keep Daily Triggers Low and Watch for Early Signs
Reduce triggers, act early, and the day stays in the Green Zone.
Tame common school triggers:
- Dust and pollen: ask for seating away from chalk dust, and keep windows closed on high-pollen days.
- Pets: limit contact with classroom animals if dander is a trigger.
- Cold air: use a scarf or mask outdoors in winter.
- Exercise: if your child’s plan includes medicine before PE, make sure the teacher or coach knows the timing and allows flexible activity when symptoms flare.
Stick to the routine:
- Make sure any school-time doses are given on schedule.
- For older kids who use a peak flow meter, follow the plan’s numbers.
Keep everyone in the loop:
- Ask the nurse to send a quick note or email if rescue medicine was needed.
- Tell the teacher if your child had a tough night so they can watch closely.
Step 7: Follow the Red Zone Emergency Protocol
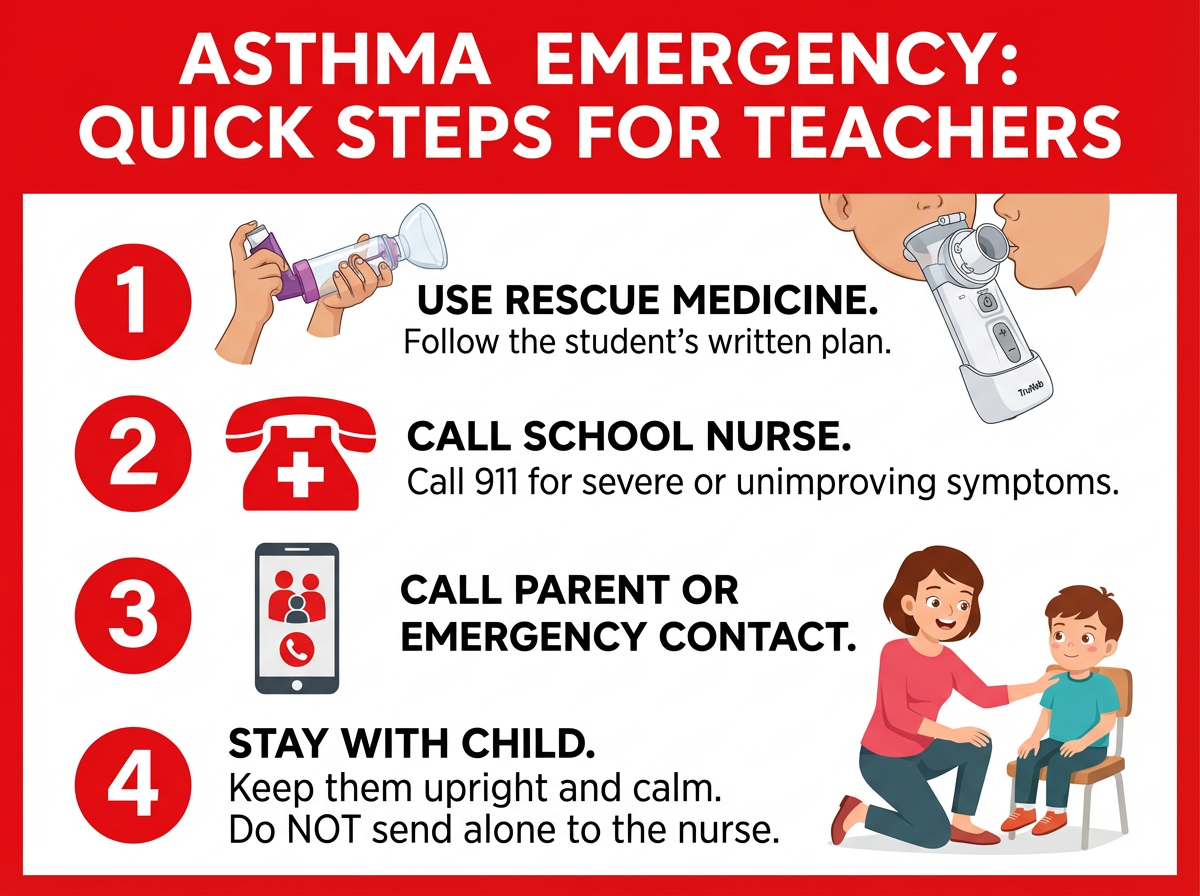
In a Red Zone emergency, school staff should follow the written plan to give rescue medicine right away, call 911 if symptoms are severe or not improving, and stay with the child until help arrives.
⚠️ Severe asthma symptoms are a medical emergency; always follow the written plan and call 911 when the plan says to.
Here’s what you can ask teachers and school staff to do if your child has a severe asthma episode at school:
Know the Red Zone signs:
- Struggling to breathe, can’t speak full sentences, ribs pulling in, lips or nails look blue.
What to do immediately:
- Make sure the student’s rescue medicine is used right away, following the steps in their written plan (inhaler with spacer or nebulizer treatment).
- Call the school nurse.
- Call 911 if the plan says to or if symptoms are severe or not improving quickly.
- Call parents or emergency contacts.
- Keep the child upright and calm; stay with them until help arrives.
When in doubt:
- If you’re unsure between Yellow and Red and the child isn’t improving, treat it like Red and follow the emergency section of the plan.
⚠️ If a child has severe trouble breathing, blue lips, or isn’t improving after rescue medicine, school staff should call 911 right away.
Step 8: Update the Plan Before Each School Year
Review and refresh the plan yearly or any time something changes.
Update it:
- At least once a year (the start of school is perfect).
- Most schools ask for a fresh, doctor-signed plan each school year.
- Any time medicines, doses, or symptoms change.
- After an ER visit or hospitalization.
Also check:
- Expiration dates on school-held inhalers and nebulizer supplies.
- Peak flow zones for older kids; personal bests can change as they grow.
- Send the new signed plan to the nurse and teachers right away.
Step 9: Use a 504 Plan for Classroom Accommodations
The action plan covers medical steps; a 504 plan secures school accommodations.
How it helps:
- Lets students carry and use their inhaler (if appropriate).
- Allows water breaks and rest when needed.
- Adjusts PE or outdoor time when air quality or pollen is poor.
- Protects against penalties for asthma-related absences.
When to consider it:
- If asthma affects school days, activities, or attendance.
- If you want accommodations clearly documented and consistent.
Your Asthma Action Plan can be attached or referenced in the 504 so staff must follow it.
Step 10: Handy Tools and Resources
Use trusted forms, simple checklists, and digital copies of your child’s asthma plan to stay organized for school.
Helpful moves:
- Scan or photograph the signed plan so you can share it quickly by email.
- Ask your school about asthma education programs.
- Keep a simple checklist for back-to-school: doctor visit, signed plan, medicines delivered, staff meeting done.
Where to find forms and guidance:
- National groups and state health sites offer ready-to-use templates and tips. Some organizations also offer Spanish or other language versions.
Safety note: Talk to your doctor before trying a new medication.
Frequently Asked Questions
This FAQ answers common questions about school asthma plans, inhaler rules, 504 plans, and using nebulizers at school.
Tap or click a question below to see the answer:
It’s a written set of doctor-approved steps for daily care and what to do when symptoms start or become an emergency. Having it at school lets teachers and the nurse act fast and correctly, which can help prevent a crisis and keep your child learning.
Clear Green, Yellow, and Red zones; daily controller medicines; when and how to use the rescue inhaler; triggers; peak flow numbers for older kids (if used); emergency contacts; and signatures so the school can give medicine.
Usually yes, with written permission from the doctor and parent. A lot of states and schools allow self-carry and self-use once it’s documented. Ask your nurse about the local rules, and keep a backup inhaler at school.
A 504 Plan is helpful if asthma affects class time, activity, or attendance. It secures accommodations like inhaler access, rest breaks, and PE adjustments. If asthma is mild and well-controlled, the action plan alone can be enough.
Update the plan at least once a year and any time your child’s asthma medicines, doses, or symptoms change—especially after an ER visit or hospitalization. Send the updated, signed plan to the school right away.
The safest step is to follow the student’s written plan right away. Make sure their rescue medicine is used as the plan describes, call the school nurse, and call 911 if the plan says to or if symptoms are severe or not improving. Keep the child upright and calm, and don’t send them alone to the nurse.
The action plan is your doctor’s medical instructions. An Individual Health Care Plan (IHCP) is the school nurse’s document for how the school will carry out those instructions during the day and in emergencies.
Yes, if the doctor writes it into the plan and the school agrees. The nurse can give nebulized medicines as ordered. Portable mesh nebulizers can make treatments quieter and easier to fit into the school day. Talk to your doctor before adding nebulized medicines.
They should have two plans: an Asthma Action Plan and an Anaphylaxis Action Plan. Make sure the school has both and knows when to use an inhaler vs. epinephrine. Keep both rescue medicines accessible.
Check national groups and state health departments for free forms and tips. You can bring these to your doctor to complete together. Always follow your doctor’s instructions.
Bottom line: A doctor-signed Asthma Action Plan, shared with your school and practiced with your child, keeps daily care on track and makes emergencies safer.
⚠️ Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your child’s doctor about their asthma, medications, and school action plan.