On this page

Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, diagnosis, and treatment options.
What Are Allergic and Non-Allergic Asthma?
Allergic asthma means your immune system reacts to allergens like pollen, dust mites, pet dander, mold, or cockroach debris. Non-allergic (intrinsic) asthma means your airways react to non-allergic factors such as viral infections, exercise, cold air, smoke, or strong fumes. Both types cause the same airway swelling and narrowing; what changes is the trigger.
Doctors sometimes call allergic asthma atopic or extrinsic, and non-allergic asthma intrinsic. About 60 percent of people with asthma have an allergic type, and some people have both kinds of triggers.
In short: Allergic asthma reacts to allergens; non-allergic asthma reacts to other triggers.
Triggers: What Sets Off Allergic vs Non-Allergic Asthma
Triggers are the main difference. In allergic asthma, your immune system makes IgE that reacts to harmless things like pollen (trees, grasses, weeds), dust mites, pet dander, mold, or cockroach debris. Exposure can spark wheeze and cough right away or within hours, and patterns can be seasonal or tied to certain indoor spaces.
In non-allergic asthma, allergy tests are negative. Flares come from other factors: viral infections like a cold or flu, exercise (especially in cold, dry air), sudden weather shifts, tobacco or wildfire smoke, strong perfumes or cleaning fumes, air pollution, stress, or certain medicines. These irritate and inflame the airways without an allergy pathway.
Takeaway: Allergens drive allergic asthma; infections, cold air, irritants, and exertion drive non-allergic asthma.
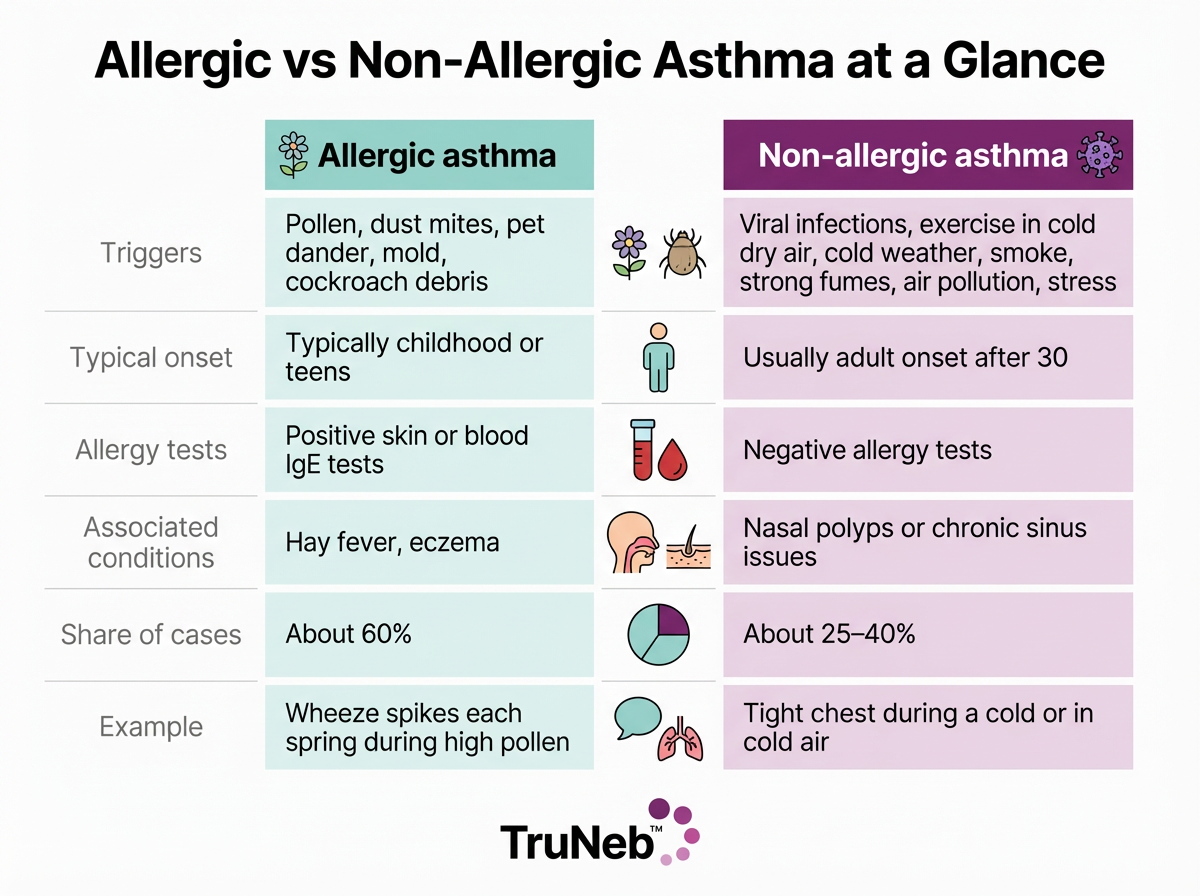
Allergic vs non-allergic asthma differ by triggers, typical age of onset, allergy test results, and share of cases. Symptoms are similar in both.
| Feature | Allergic asthma | Non-allergic asthma |
|---|---|---|
| Triggers | Pollen, dust mites, pet dander, mold, cockroach debris | Viral infections, exercise in cold dry air, smoke/fumes, air pollution, weather changes, stress |
| Typical onset | Childhood or teens | Adulthood (30+) |
| Allergy tests | Positive (skin or IgE blood) | Negative |
| Associated conditions | Hay fever, eczema | Nasal polyps or chronic sinus issues |
| Share of cases | About 60% | About 25–40% |
| Example pattern | Spring pollen flare | Flare during a cold or in cold air |
Numbers are approximate and vary by study. Talk to your doctor about your specific pattern.
Example: Pollen vs Cold Air
Mark steps outside on a high-pollen day and soon starts sneezing and wheezing. That pattern points to allergic asthma. Emily feels fine in spring, but a blast of cold air tightens her chest when she runs. That pattern points to non-allergic asthma.
In short: Sneezing plus wheeze with pollen suggests allergic asthma; tight chest in cold air suggests non-allergic asthma.
Symptoms: Do They Differ Between Allergic and Non-Allergic Asthma?
Core asthma symptoms are the same in both types, because both narrow and inflame the airways.
- Wheezing, especially on exhale
- Cough, typically worse at night or early morning
- Chest tightness
- Shortness of breath
Clues come from context. Allergic flares usually ride along with allergy signs like sneezing, a runny or stuffy nose, or itchy eyes during high exposure. Non-allergic flares can show up without allergy signs and during a cold, a hard workout, a smoky room, or a winter snap.
In short: The symptoms match; the timing and context point to the type.
Non-allergic asthma triggers often include viral infections, exercise in cold dry air, smoke or strong fumes, and air pollution (ACAAI).
Who Gets Each Type: Age of Onset and Risk Factors
Allergic asthma typically begins in childhood or the teen years, especially in families with allergies or asthma. It commonly travels with other allergic problems like hay fever or eczema.
Non-allergic asthma tends to appear later, usually after age 30. It’s reported more in adult women and can follow repeated respiratory infections or exposures at work; some people also have chronic sinus issues or nasal polyps.
Takeaway: Allergic asthma tends to start young with an allergy history; non-allergic asthma more commonly starts in adults without allergies, but there are exceptions and overlap.
Inhalers, Nebulizers, and Medication Delivery: Finding What Works
Most people do well with inhalers when technique is solid. A nebulizer turns liquid medicine into a fine mist you breathe in over several minutes. It can help during bad flares, for young children, or for adults who struggle with inhalers.
For example, a portable mesh nebulizer like TruNeb™ can offer quiet, steady delivery at home or on the go. Some people with either asthma type keep a nebulizer in their toolkit for tough moments.
Key point: The best device is the one that gets medicine into your lungs correctly and consistently.
Safety notes: Talk to your doctor before trying a new medication. Hypertonic saline isn’t a standard asthma treatment; specialists use it only in specific mucus‑heavy lung conditions. ⚠️ Steam inhalers are not the same as nebulizers and aren’t meant for breathing in prescription asthma medicines.
In short: Use the device you can use well; your doctor can help you choose and adjust.
How Doctors Differentiate the Two Types
Doctors diagnose asthma with lung tests like spirometry and by your history. To tell the type, they look at allergy testing and your pattern of triggers.
Allergic asthma is more likely when skin prick tests or specific IgE blood tests show sensitization to things that also match your flares, like dust mites or pollen. When allergy tests are negative and the story points away from allergens, the label is non-allergic (intrinsic) asthma. Some clinics also use exhaled nitric oxide (FeNO) to gauge allergy-related inflammation, but it isn’t a standalone diagnostic.
In short: Allergy testing plus your symptom pattern is what separates allergic from non-allergic asthma.
Fast facts: Inhaled corticosteroids are the first-line controller for persistent asthma. Using your inhaler or nebulizer correctly every day helps prevent attacks (NHLBI).
Living With Your Asthma Type: Action Plan and Next Steps
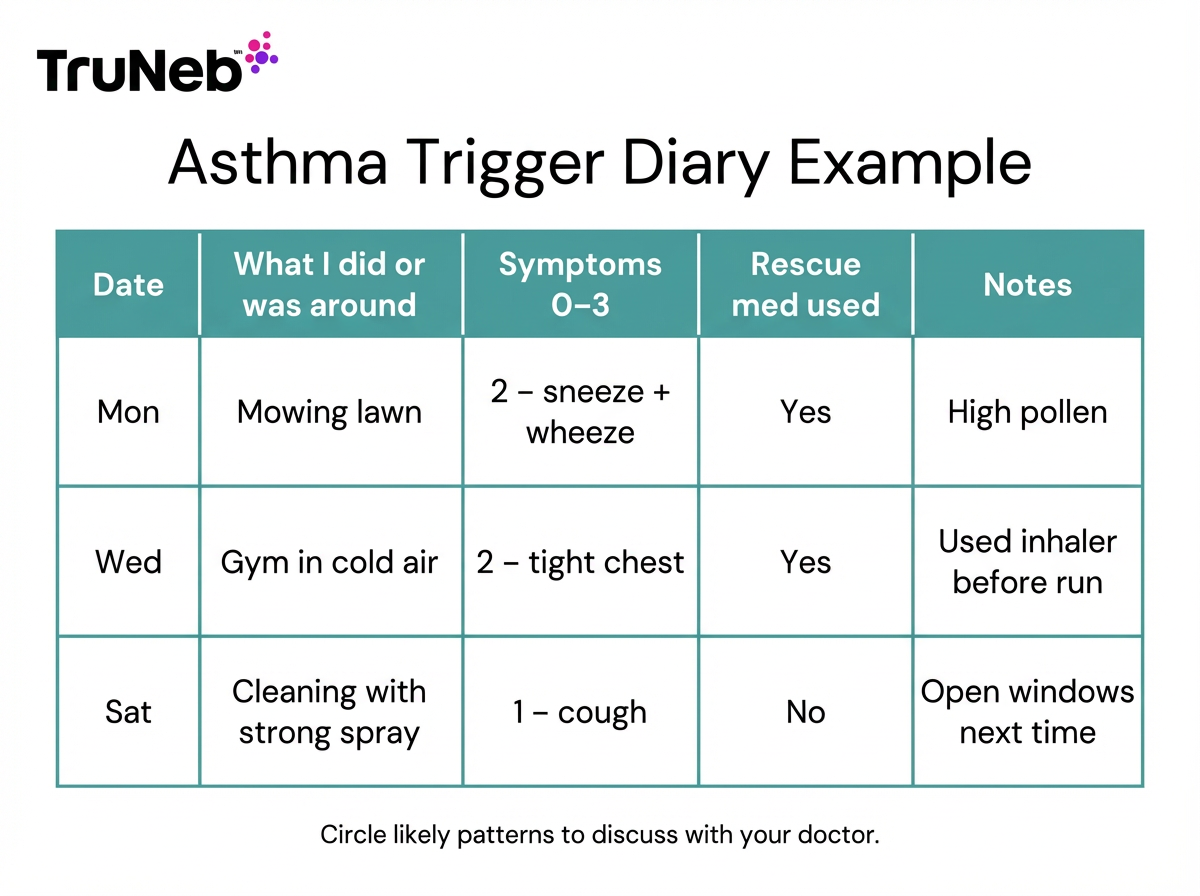
1) Track your triggers. Write down what you were doing, where you were, and the weather when symptoms hit. Patterns typically pop out in 2–3 weeks.
2) Share your notes and ask about testing. If patterns hint at allergies, ask about skin or IgE blood testing.
3) Personalize your asthma action plan. Include steps for high‑pollen days if allergic, and cold or sick days if non‑allergic.
4) Tune your environment. For allergic triggers, reduce dust, dander, and mold. For non‑allergic triggers, avoid smoke and harsh fumes and check air quality.
5) Controller medicines work best when you take them regularly, the way your doctor prescribed. If symptoms keep breaking through, ask your doctor to adjust the plan.
6) Know when to see a specialist. If control is poor or triggers are unclear, an allergist or pulmonologist can add options.
7) ⚠️ If you have severe trouble breathing, can’t speak in full sentences, notice blue lips or face, or your rescue inhaler isn’t helping, seek emergency medical care right away (call 911 or your local emergency number).
Talk to your doctor if symptoms don’t improve, wake you at night, or you’re using your rescue inhaler more than usual.
In short: Track, test, plan, and adjust with your doctor to keep control.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes, you can have both at the same time. A lot of people react to allergens like pollen and also flare with colds or cold air, so your plan should cover both.
No. Any type of uncontrolled asthma can be serious or life‑threatening—the key is good control and regular follow‑up with your doctor.
Look for patterns with pollen, pets, or dust and allergy symptoms like sneezing or itchy eyes, then confirm with skin or IgE blood testing through your doctor.
The core inhaler medicines are the same. Allergic asthma can also benefit from allergen avoidance, treating nose allergies, and sometimes immunotherapy or biologics if your doctor recommends them.
Not exactly. Exercise can trigger non‑allergic asthma, but exercise‑induced bronchospasm is a specific pattern your doctor can diagnose and manage with pre‑exercise steps if needed.
Treatment Options for Allergic vs Non-Allergic Asthma
The core treatment is similar for both types: daily controller inhalers to reduce airway swelling, a quick‑relief inhaler for symptoms, and a written asthma action plan you follow with your doctor.
If you have allergic asthma, reducing exposure helps. Dust‑proof bedding, HEPA filtration, pet‑dander steps, and planning for high‑pollen days can cut flares. Treating nose allergies can also improve control. For some, allergen immunotherapy and, in tougher cases, biologic medicines that target allergy‑related pathways can reduce attacks.
If you have non‑allergic asthma, you focus on other triggers. Try to prevent infections when you can, warm the air you breathe in winter, avoid smoke and harsh fumes, and ask your doctor about using medicine before exercise if that’s a trigger for you. Doctors often recommend staying up to date on vaccines to help reduce infection‑related flares. Some people with certain inflammation patterns respond well to biologics, even without allergies.
Takeaway: Both types use the same base inhalers; allergic asthma adds allergen‑focused steps and options like immunotherapy.