On this page

Can You Give Albuterol Nebulizer Every 2 Hours? What’s Safe
Short answer: no, not on a routine basis. Most care plans space albuterol nebulizer treatments every 4–6 hours as needed. Albuterol is a short-acting beta-2 agonist (SABA), a fast-acting bronchodilator that relaxes the muscles around the airways and usually helps for about 4 hours. Dosing again at 2 hours raises side-effect risk without much extra breathing relief.
This guide is primarily for parents of children with asthma using an albuterol nebulizer; adults can apply the same timing principles unless their doctor advises otherwise.
If your child seems to need another treatment in just 2 hours, treat that as a warning sign and call your pediatrician for guidance.
Safety note: Talk to your doctor before changing your albuterol schedule.
Key takeaway: Routine spacing is 4–6 hours; 2-hour dosing should be short-term and doctor-directed during a flare, not routine home care.
Why Albuterol Nebulizer Treatments Are Usually 4–6 Hours Apart
Albuterol’s effect typically lasts about 4 hours. That’s why the standard guidance is every 4–6 hours as needed. Giving another dose too soon doesn’t add much breathing benefit, but it does increase chances of side effects like jitteriness and a fast heartbeat.
This matches common drug references and labeling, which list albuterol doses every 4–6 hours as needed for most children 4 and older. For younger children, your doctor sets the exact plan. If relief seems to wear off much earlier than 4 hours, the flare is stronger than usual. Instead of redosing early on your own, call your pediatrician to adjust the plan.
Key takeaway: Albuterol’s relief lasts around 4 hours, so safe spacing is every 4–6 hours.
The Risks of Using Albuterol Too Frequently
Giving albuterol too frequently can backfire. Side effects build up - shakiness, a racing heartbeat, headaches, and feeling on edge. Stacking doses can also bring diminishing returns (your airways respond less) while the risks go up.
A simple rule-of-thumb doctors use is the Rule of Four: if you need albuterol more frequently than every 4 hours or more than 4 times in 24 hours, that’s a red flag. It means the asthma isn’t well controlled and the plan likely needs to change. Overreliance on rescue medicine can even worsen overall control over time. If you’re needing albuterol this frequently, it usually means your child’s daily controller medicines (like an inhaled steroid) need to be reviewed and adjusted by your doctor.
If you find yourself reaching for a nebulizer again at the 2-hour mark, don’t keep stacking doses. Call your doctor to update the action plan.
Key takeaway: Using albuterol more than every 4 hours or over 4 times a day signals poor control and higher risk.
When Doctors Allow More Frequent Dosing
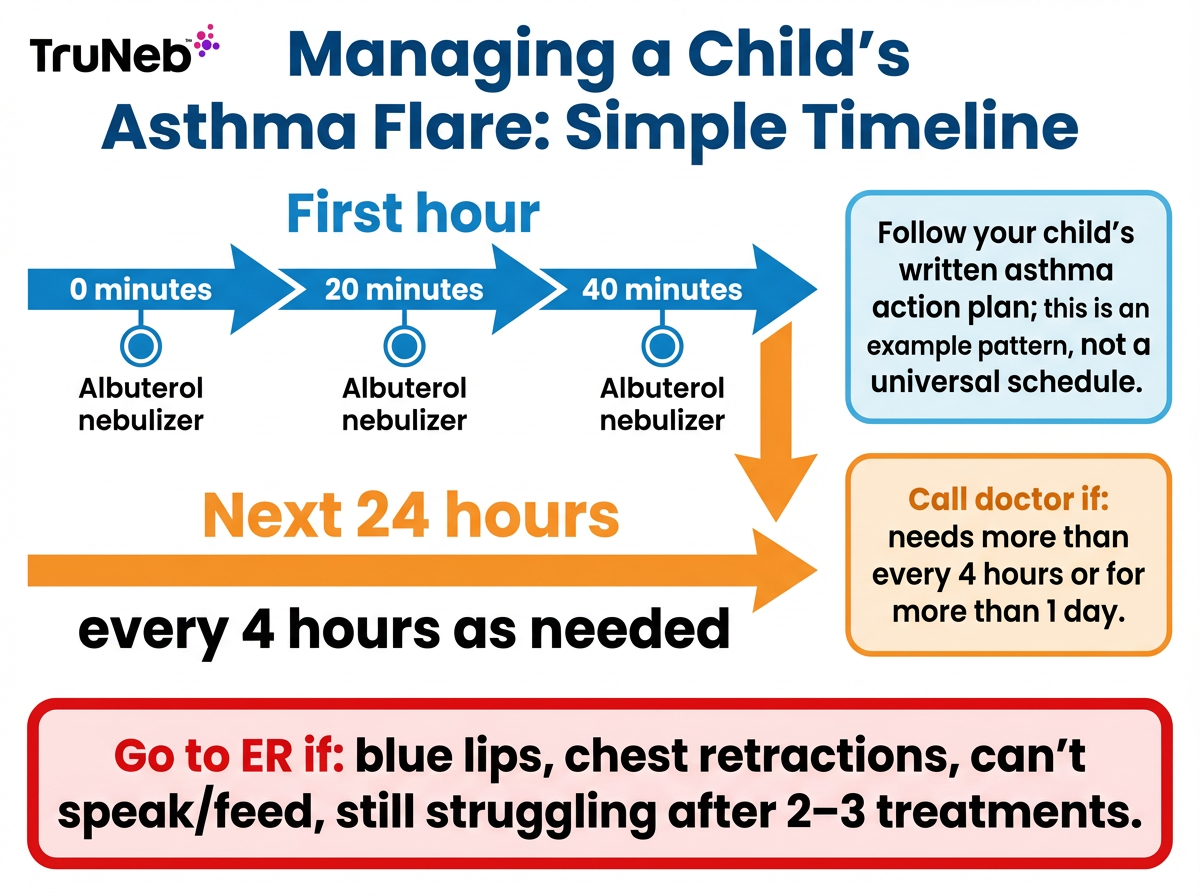
There are emergency exceptions. During a bad asthma flare, some asthma action plans call for back-to-back albuterol treatments in the first hour (for example, one treatment, then another at 20 minutes, and a third at 40 minutes). If your child improves, you move back to every 4 hours as needed afterward. This kind of schedule should only be followed if it’s written in your child’s asthma action plan or your doctor has told you to do it. These steps are usually described in the Yellow or Red Zone of an asthma action plan. Do not create your own schedule from an article.
If symptoms don’t settle, your doctor may add other medicines (like oral steroids) and ask you to head to urgent care or the ER. In the hospital, they sometimes give continuous albuterol with monitoring.
In practice, that looks like back-to-back in the first hour when your child’s plan calls for it, then spacing to every 4 hours.
More frequent dosing is short-term and doctor-directed. If you don’t have a written asthma action plan, ask your pediatrician to create one so you know exactly what to do.
Key takeaway: Frequent dosing is a temporary, guided step during a flare, not routine home care.
How Many Albuterol Nebulizer Treatments Are Safe in 24 Hours?
A practical rule-of-thumb is about 4 albuterol nebulizer treatments in 24 hours before you call your doctor. Hitting or exceeding this number, or needing treatments closer than every 4 hours, is a red flag that the flare is more serious or that long-term control needs adjustment.
This mirrors the Rule of Four: more than 4 doses a day or dosing sooner than every 4 hours signals poor control. Plans can differ by child, so follow your doctor’s instructions. Treat this as a signal to call for help, not a guaranteed safe ceiling.
Key takeaway: If you’re needing more than about 4 albuterol nebulizer treatments in 24 hours, it’s time to call your doctor, not to keep increasing doses.
Signs of Albuterol Overdose or Overuse in a Child
If treatments have been given more frequently than prescribed, or you’re worried about too much albuterol, watch for:
- Severe tremors or shaking (can’t sit still)
- Very fast heartbeat (palpitations)
- Agitation, restlessness, or unusual fussiness
- Nausea or vomiting
- Headache or dizziness
- Chest pain or chest tightness (older kids may report this)
- Weakness or muscle cramps (can be tied to low potassium)
- Trouble sleeping or extreme hyperactivity
- Breathing gets worse right after a dose (rare paradoxical reaction)
If you suspect an overdose, call Poison Control at 1-800-222-1222 (in the U.S.) or seek emergency care.
Key takeaway: Shakiness and a racing heartbeat are early overdose signs; worsening breathing is an emergency.
When to Stop Home Treatment and Seek Emergency Care
These thresholds mirror the Yellow and Red Zone language in typical asthma action plans.
Call your doctor (same day) if:
- Your child needs albuterol more frequently than every 4 hours to stay comfortable.
- You’ve reached about 4 treatments in 24 hours and they still need more.
- After an hour of repeated treatments, they’re not clearly moving back to the green zone.
- You’re seeing frequent flare-ups or you’re worried the plan isn’t working.
⚠️ Emergency warning: Go to the ER or call 911 now if:
- Your child is still struggling to breathe after 2–3 back-to-back treatments.
- You see chest retractions (skin pulling in at ribs/neck) or a blue tint around lips/fingernails.
- They can’t speak in full sentences (or an infant can’t feed because of breathing).
- Their heart is pounding extremely fast.
- They are very drowsy, confused, or worsening quickly.
- You suspect an overdose or they’re getting worse right after a dose.
Trust your instincts. If you’re alarmed, it’s safer to get urgent care.
Key takeaway: If albuterol isn’t holding for 4 hours or breathing looks hard, seek care now.
Using a Nebulizer Properly to Follow the Dosing Plan
Your child gets the best result when the full dose reaches their lungs. Simple tips help:
- Measure the exact dose and use a snug mask or mouthpiece seal.
- Run the treatment until the medicine is gone (usually several minutes).
- Clean and dry parts after each use to prevent germs and clogs.
- If you see devices labeled “steam inhaler,” don’t use them for albuterol; they’re not designed to deliver prescription medicine to the lungs.
A portable mesh device can make all of this easier. The TruNeb™ Portable Mesh Nebulizer is quiet, compact, and battery powered, so you can give treatments on time at home, in the car, or at school without the noise of a compressor. It doesn’t change what you give or the schedule - it just helps you stick to the plan.
Some doctors prescribe nebulized saline to thin mucus (for example, 3% or 7% hypertonic saline). This is usually used to thin mucus when a doctor prescribes it and is not a rescue treatment for sudden wheezing or an asthma attack. If your doctor adds saline to the plan, TruNeb offers these solutions for use with the device. Always check with your doctor before adding anything new to your child’s nebulizer plan.
Key takeaway: The right device helps you follow safe timing; it never replaces your doctor’s dosing plan.
Frequently Asked Questions
Tap or click a question below to see the answer:
About every 4–6 hours as needed. If you’re thinking about dosing sooner, call your doctor.
Not routinely. Only do this short-term during a severe flare if your doctor has told you to.
A practical max is about 4 sessions in 24 hours before checking in with your doctor. If you hit this number or think you need more, don’t just keep dosing—call your doctor or seek urgent care.
Side effects ramp up (shakiness, fast heartbeat, feeling on edge) with little added relief. It’s also a sign the asthma isn’t controlled and controller medicines likely need review.
Marked tremors, a racing heartbeat, agitation, nausea/vomiting, or worsening breathing after a dose. Get care right away.
If your child is still struggling after 2–3 treatments, shows blue lips or chest retractions, or can’t speak/feed normally, go now.
Key takeaway: Space albuterol 4–6 hours; 2-hour dosing needs explicit doctor direction.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always talk with your doctor about your or your child’s symptoms, medications, and treatment plan.







