On this page

What Is Airway Inflammation?
Airway inflammation is the swelling and irritation of your breathing tubes (bronchi and bronchioles). It’s your immune system’s response to a trigger. The lining puffs up, blood flow rises, and your airways make extra mucus. Your immune system sends white blood cells and chemical signals that drive this swelling and mucus.
Muscles around the tubes can tighten, which further narrows the space for air to move.
It can feel like trying to breathe through a pinched straw. Less room for air means cough, wheeze, chest tightness, or shortness of breath.
Airway inflammation isn’t a disease by itself. It shows up in many conditions, including asthma, bronchitis, and COPD. You can have airway inflammation from allergies or irritants even when there’s no infection. Calming that inflammation is a big step toward easier breathing.
Bottom line: Airway inflammation means swollen, narrowed breathing tubes that usually produce extra mucus.
Common Causes of Airway Inflammation
Most inflamed airways trace back to a few triggers. Here are the big ones to watch:
Allergens and Irritants
- Pollen, dust mites, pet dander, and mold can spark inflammation in the airway lining.
- Cigarette smoke (including secondhand smoke), wood smoke, and air pollution can irritate and inflame the bronchi.
- Workplace dust or chemical fumes (for example, in factories, farming, or salons) can also irritate and inflame your airways over time.
Infections (Viruses and Bacteria)
- Cold viruses and influenza infect the airway lining and stir up inflammation.
- RSV is a frequent cause of airway inflammation in young children.
- Most acute bronchitis is viral, not bacterial.
Chronic Lung Disease
- In asthma and COPD, the airway lining is prone to ongoing inflammation that can flare with triggers.
In some people, acid reflux (GERD) that reaches the airways can also keep the lining irritated and inflamed.
Key takeaway: Allergens, infections (like flu/RSV), and irritants such as cigarette smoke are the most common causes of airway inflammation.
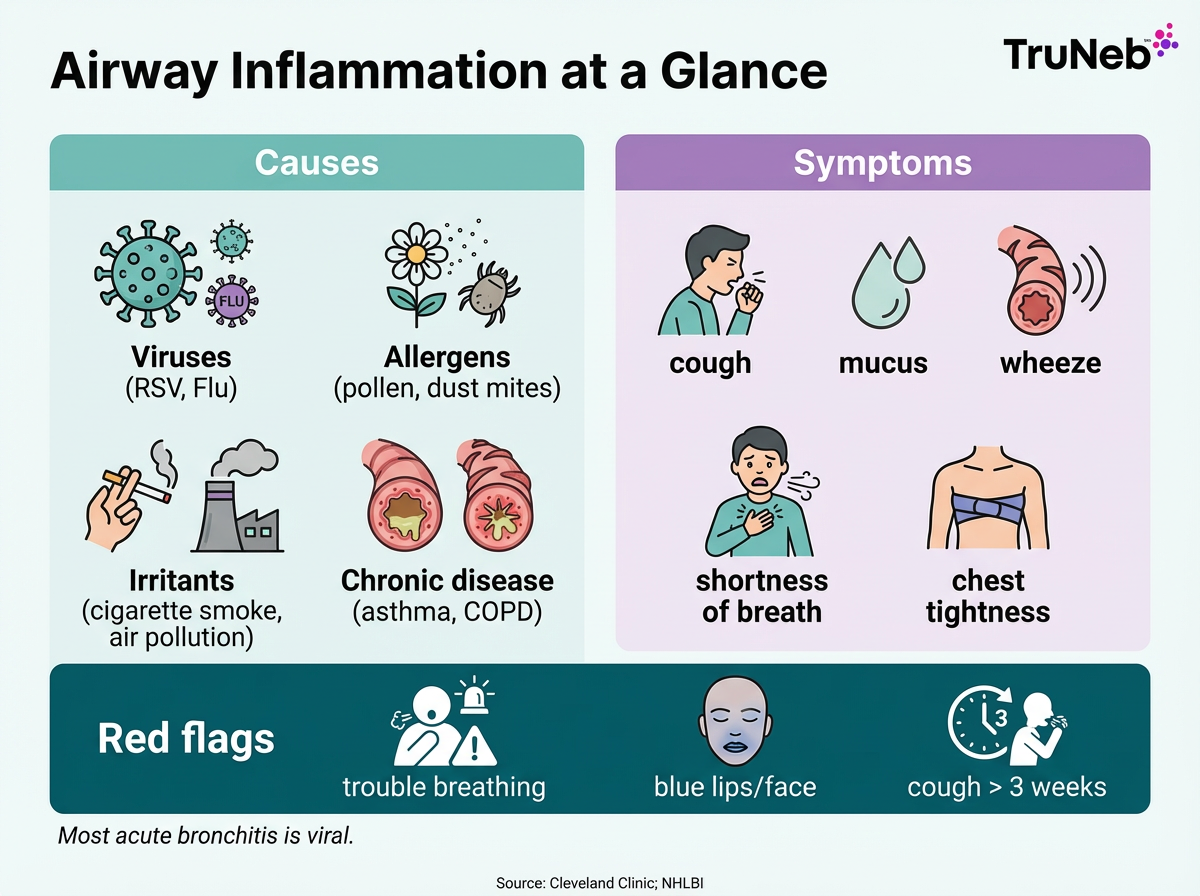
Symptoms and When to Seek Care for Airway Inflammation
Symptoms to Watch
- Cough that hangs on: Your body is trying to clear irritated, swollen airways.
- Mucus or phlegm: Inflammation boosts mucus, leading to mucus buildup that can be clear or colored.
- Wheezing: A whistling sound when you breathe out, from narrowed passages.
- Shortness of breath: Air has a hard time getting through swollen, tight tubes.
- Chest tightness or discomfort: Your chest can feel squeezed or heavy.
- Tiredness: Working harder to breathe can wear you out.
If an infection is involved, you might also notice fever, chills, or body aches. If allergies or asthma are driving your airway inflammation, you’re less likely to have fever but you might notice more wheeze and chest tightness.
When to Get Help
- ⚠️ Call 911 or go to the ER if you’re struggling to breathe, can’t speak in full sentences, your lips or face look blue, or your rescue inhaler isn’t helping during a bad flare.
- See a doctor soon if your cough lasts more than 2–3 weeks, wheeze or shortness of breath is new or getting worse, you have repeated flare-ups, or your asthma/COPD plan isn’t keeping symptoms under control.
⚠️ Bottom line: Seek emergency care for severe breathing trouble; see your doctor if symptoms persist, worsen, or keep coming back.
Airway Inflammation in Common Conditions
Asthma
Asthma is a chronic inflammatory condition of the airways. This airway inflammation in asthma makes the lining extra sensitive to triggers like pollen, dust, cold air, or exercise. That swelling, plus tighter airway muscles and more mucus, leads to wheeze, cough, and chest tightness. That’s why you might wheeze or feel your chest tighten during a flare.
Bronchitis (Acute vs Chronic)
Acute bronchitis is short-term airway inflammation, usually from a virus (also called a chest cold). The bronchi swell and make lots of mucus, which causes a nagging cough.
Chronic bronchitis is long-term airway inflammation, usually from years of smoke or irritant exposure. Daily cough and phlegm for months at a time is common, and it’s part of COPD.
COPD
In COPD, airway inflammation is persistent. Over time it thickens and damages the airway walls, narrowing the tubes and making breathing harder. Flare-ups, commonly from infections, can spike inflammation even more. This chronic airway inflammation in COPD can lead to permanent narrowing over time.
RSV Bronchiolitis (Infants)
RSV inflames the tiniest airways (bronchioles) in babies and toddlers. These small tubes swell and fill with mucus, leading to fast breathing and wheeze. It can be serious in little ones and can need medical care. ⚠️ If a baby is breathing very fast, using their belly or neck muscles to breathe, or looks blue around the lips or face, seek emergency care right away.
Key takeaway: Asthma, bronchitis, COPD, and RSV all involve airway inflammation, but the pattern (acute vs chronic) and triggers differ.
How to Reduce and Manage Airway Inflammation
Reducing airway inflammation usually takes a mix of avoiding triggers, using the right medicines, and giving your lungs some support at home.
Avoid Triggers and Irritants
- Quit smoking and avoid secondhand smoke.
- Limit exposure to allergens.
- Improve indoor air quality: use a HEPA air purifier, wash bedding often, and control dust and mold.
- Check air quality and skip outdoor exertion on high-pollution or high-pollen days.
- Stay up to date on vaccines (flu, COVID) to lower infection-related flares.
Medications that Reduce Inflammation
- Inhaled corticosteroids help quiet the airway lining over time (core therapy in asthma; used in COPD as directed by a doctor).
- Bronchodilators (like albuterol) don’t treat inflammation but open tight airways so you can breathe easier.
- Doctors sometimes prescribe short courses of oral steroids for severe flare-ups.
- For severe allergic asthma, specialists sometimes prescribe biologic therapies.
- Antibiotics don’t help most airway inflammation from viruses and aren’t routine unless a bacterial infection is confirmed. Your doctor will decide if antibiotics are needed based on your exam and test results.
Your doctor can use breathing tests or imaging to figure out what’s driving your airway inflammation before choosing a treatment plan.
Nebulizer Therapy and Saline
A nebulizer turns liquid medicine into a fine mist you breathe in. It can help when you need steady, deep delivery or when inhalers are hard to use during symptoms.
Modern portable mesh nebulizers, like the TruNeb™ Portable Mesh Nebulizer, are small, quiet, and battery-powered. TruNeb is compact and portable, so you can take treatments at home or on the go. A device like TruNeb can fit into the plan your doctor gives you, but it doesn’t replace medical advice or prescriptions.
Hypertonic saline (3% or 7%) is a salty solution that can draw water to the airway surface, thin sticky mucus, and help reduce airway wall swelling. Doctors sometimes recommend it for mucus-heavy conditions. TruNeb also offers 3% and 7% hypertonic saline produced in an FDA-registered lab for use as directed with a nebulizer. Your doctor can tell you if hypertonic saline is right for your lungs, since it isn’t suitable for everyone.
Only use medications or solutions in your nebulizer that your doctor has prescribed. Skip essential oils or homemade mixtures. You might see boxes labeled "steam inhaler" in stores; these are not the same as nebulizers and aren’t meant for breathing medication.
Supportive Care at Home
- Drink fluids and use a clean humidifier to help thin mucus.
- Take warm showers or breathe moist air to soothe irritated airways.
- Rest and pace activity while symptoms settle.
⚠️ Safety note: Always talk to your doctor before trying a new medication or nebulized solution, or making changes to your existing treatment plan.
Key takeaway: Cut triggers, use prescribed anti-inflammatory treatments, and add nebulized therapy if your doctor recommends it.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before starting, stopping, or changing any treatment.