On this page
Bronchiectasis is a lung condition that causes the airways to become permanently widened, leading to mucus build-up and recurrent infections. Managing bronchiectasis effectively involves regular airway clearance to help remove mucus and prevent complications. This article explores the best airway clearance techniques for bronchiectasis, the benefits they offer, and the supporting research to help those with bronchiectasis breathe easier.
Understanding Bronchiectasis
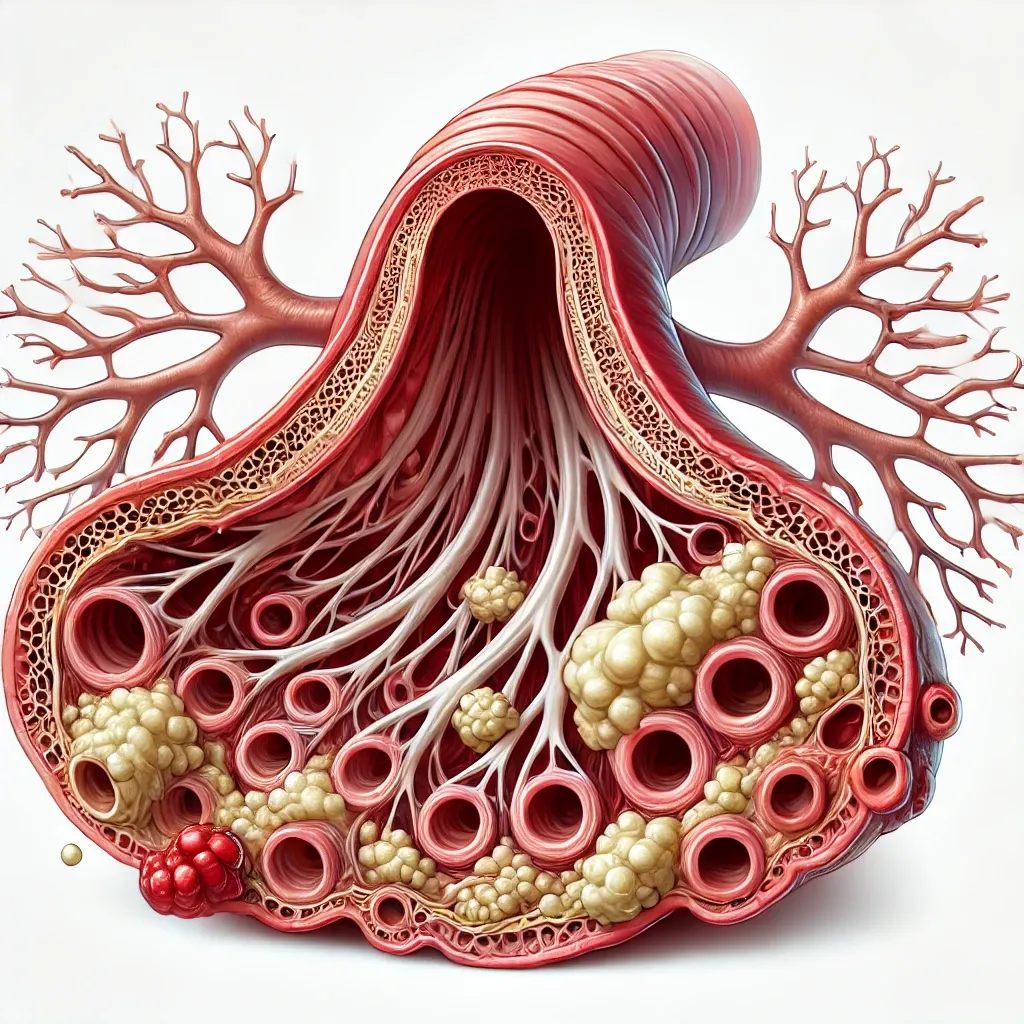
Pathophysiology of bronchiectasis
Bronchiectasis happens when the airways in the lungs become damaged and abnormally widened. This damage makes it hard for the lungs to clear out mucus, which then builds up and creates a breeding ground for bacteria, leading to repeated lung infections. Various factors can cause this condition, including severe infections, genetic disorders like cystic fibrosis, and chronic inflammatory diseases.
Symptoms and complications
People with bronchiectasis often experience a chronic cough, large amounts of mucus, shortness of breath, chest pain, and frequent lung infections. Over time, these symptoms can worsen, leading to decreased lung function and a lower quality of life.
The role of mucus in bronchiectasis
In healthy lungs, mucus traps and removes germs and particles. But in bronchiectasis, the airways produce too much thick mucus, which becomes hard to clear out. This mucus buildup blocks the airways, leading to more infections and inflammation, creating a cycle that worsens lung health over time.
Understanding these aspects of bronchiectasis emphasizes why effective airway clearance is super important for managing the condition and improving quality of life for people dealing with the disease.
What Causes Bronchiectasis?
Bronchiectasis develops from a variety of underlying issues that damage the airways and impact their ability to clear mucus effectively. Up to 40% of cases have no known cause, but here are the most common causes we understand:
1. Infections: Severe or repeated lung infections are a leading cause of bronchiectasis. Infections like pneumonia, whooping cough, or tuberculosis can cause serious airway damage, leading to their dilation and the chronic production of excess mucus.
2. Cystic Fibrosis: Cystic fibrosis is a genetic disorder that causes thick, sticky mucus to build up in the lungs, pancreas, and other organs. This mucus can block the airways, causing repeated infections potentially, bronchiectasis. It's a common cause, especially in younger people.
3. Immune System Disorders: Conditions that affect the immune system, such as primary immunodeficiency diseases and autoimmune disorders are related to developing bronchiectasis. An impaired immune system means the body is less capable of fighting off infections, which can cause repeated damage to the lung tissues.
4. Allergic Bronchopulmonary Aspergillosis (ABPA): ABPA is an allergic reaction to the fungus Aspergillus, which can colonize the airways. This reaction can cause inflammation and damage and ultimately bronchiectasis.
5. Primary Ciliary Dyskinesia (PCD): PCD is a rare genetic disorder where the cilia (tiny hair-like structures in the airways that help move mucus out) do not function properly. This leads to mucus build-up and recurrent infections, eventually causing bronchiectasis.
6. Autoimmune Diseases: Autoimmune diseases like rheumatoid arthritis and Sjögren's syndrome can cause inflammation in various parts of the body, including the lungs. This inflammation can eventually result in bronchiectasis.
7. Environmental and Occupational Exposures: Long-term exposure to harmful substances like smoke, fumes, and chemicals can irritate and damage the airways, contributing to the development of bronchiectasis.
Understanding the underlying causes of bronchiectasis is important for proper diagnosis and treatment. Identifying and managing these causes can help prevent further damage to the lungs and improve overall respiratory health.
The Importance of Airway Clearance
Airway clearance techniques for bronchiectasis are a critical part of managing the disease. These techniques help in several ways:
1. Removing Excess Mucus
Effective airway clearance helps remove excess mucus from the lungs, reducing the risk of infections and making it easier to breathe.
2. Reducing Inflammation
By getting rid of mucus, airway clearance techniques for bronchiectasis can reduce inflammation in the airways. This can decrease the frequency and severity of flare-ups, improving overall lung function.
3. Preventing Infections
Regularly clearing mucus helps prevent bacterial infections. Mucus can trap bacteria, and if not cleared, it becomes a breeding ground for lung-damaging infections.
4. Improving Quality of Life
Patients who regularly practice airway clearance techniques often feel they have a better quality of life. They find it easier to engage in daily activities, exercise, and experience less shortness of breath and fatigue.
Airway clearance exercises are one of the most important management techniques for bronchiectasis – and ultimately a way for patients to feel better each day.
Common Airway Clearance Techniques for Bronchiectasis
Active Cycle of Breathing Techniques (ACBT)
Description: ACBT is a method that involves a series of breathing exercises designed to move mucus from deep in the lungs to the throat where it can be coughed out.
Steps:
- Deep Breathing: Inhale deeply to move mucus from the deeper parts of the lungs.
- Relaxed Breathing: Breathe normally to allow airways to open.
- Huff: Exhale forcefully to push mucus toward the throat.
- Cough: Finally, cough to expel the mucus.
Benefits:
- Helps clear mucus from the lungs efficiently.
- Reduces the risk of infections by maintaining clear airways.
Evidence and Studies: Research shows ACBT improves mucus clearance, enhances lung function, and is well-received by patients for its simplicity and effectiveness.
Coughing and Huffing
Description: This technique involves controlled coughing and making huffing sounds to clear mucus from the lungs.
Steps:
- Inhale Deeply: Breathe in deeply through the nose.
- Huff: Forcefully exhale with a “huff” sound to mobilize mucus.
- Repeat: Perform this sequence 2-3 times as needed.
Benefits:
- Effective for clearing mucus without additional equipment.
- Can be easily performed by the patient alone.
Evidence and Studies: Studies support the effectiveness of coughing and huffing in mucus clearance, demonstrating significant improvements in lung function and patient outcomes.
Manual Chest Physiotherapy (CPT)
Description: Manual CPT includes techniques like percussion and vibration applied to the chest to help loosen mucus.
Steps:
- Positioning: Get in a position that helps gravity assist in mucus drainage.
- Percussion/Vibration: Have someone apply rhythmic percussion or vibration to the chest wall.
- Cough: Cough to expel the mucus throughout the treatment.
Benefits:
- Assists in moving mucus from the smaller airways to the larger ones.
- Can be customized to the patient's needs by a respiratory therapist.
Evidence and Studies: Research indicates that manual CPT is effective, particularly when combined with other techniques, in improving mucus clearance and respiratory function.
High-Frequency Chest Wall Oscillation (HFCWO)
Description: HFCWO involves using a vest that delivers repeated air pulses to the chest, helping to loosen and mobilize mucus.
Steps:
- Wear the Vest: Put on the oscillating vest.
- Adjust Settings: Set the device to the appropriate frequency and intensity.
- Therapy Sessions: Conduct regular sessions as prescribed by a healthcare provider.
Benefits:
- Loosens mucus throughout the lungs and propels it toward larger airways.
- Can be used independently at home.
Evidence and Studies: Studies show HFCWO reduces respiratory infections and hospitalizations, demonstrating its effectiveness in long-term management of bronchiectasis.

Positive Expiratory Pressure (PEP) Therapy
Description: PEP therapy uses a device that creates resistance during exhalation, helping to keep airways open and clear mucus.
Steps:
- Exhale through the Device: Breathe out through the PEP device for around 5 seconds, keeping your cheeks stiff.
- Follow Breathing Pattern: Use the prescribed pattern to maximize effectiveness.
Benefits:
- Helps maintain open airways and aids in mucus clearance.
- Enhances overall lung function and reduces the risk of infection.
Evidence and Studies: Comparative studies indicate that PEP therapy is as effective as other airway clearance techniques, improving lung function and patient compliance with therapy (because of how easy it is to do).

Autogenic Drainage
Description: Autogenic Drainage is a technique involving controlled breathing exercises that help move mucus from the lower to the upper airways, making it easier to expel.
Steps:
- Unstick Phase: Breathe at low lung volumes to loosen mucus.
- Collect Phase: Breathe at mid lung volumes to gather the mucus.
- Evacuate Phase: Breathe at high lung volumes to move mucus to the upper airways for expulsion.
Benefits:
- Particularly effective for patients who have difficulty expectorating mucus.
- Can be performed independently without the need for equipment.
Evidence and Studies: Clinical studies have shown that Autogenic Drainage can improve mucus clearance and lung function. Patients often report better breathing and reduced symptoms after regular practice.
Hypertonic Saline
Description: Hypertonic saline is a concentrated saltwater solution used to help clear mucus from the lungs. It works by drawing water into the airways, thinning the mucus, and making it easier to cough out.
Steps:
- Preparation: Use a nebulizer to administer the hypertonic saline solution.
- Inhalation: Breathe in the mist produced by the nebulizer deeply and steadily until the solution is finished.
- Coughing: After inhalation, perform coughing or huffing techniques to expel the loosened mucus.
Benefits:
- Helps thin and loosen mucus, making it easier to clear from the lungs.
- Can reduce the frequency of lung infections by keeping airways clear.
- Improves overall lung function and breathing comfort.
Evidence and Studies: Research has demonstrated that regular use of hypertonic saline can significantly improve mucus clearance and reduce the incidence of respiratory infections. Studies have shown improvements in lung function and quality of life for patients using hypertonic saline as part of their airway clearance regimen. Ask your doctor about hypertonic saline for bronchiectasis.
Airway Clearance Devices
Types of Devices:
- Positive Expiratory Pressure (PEP) Devices: Create resistance during exhalation, helping keep airways open and aiding mucus clearance.
- Flutter Devices: Combine PEP with high-frequency oscillations to loosen mucus.
- Oscillating Positive Expiratory Pressure (OPEP) Devices: Use vibrations and resistance to help move mucus from the lungs.
How to Choose the Right Device:
- Medical Assessment: A healthcare provider should assess your condition to recommend the a device that makes sense for you.
- Ease of Use: Consider how easy the device is to use and integrate into your daily routine.
- Personal Preference: Some patients may prefer certain types of devices over others based on comfort and effectiveness.
- "Try It": Sometimes you have to just try a device to see if it works well for you!
Using airway clearance devices can significantly improve the management of bronchiectasis.
Recent Studies and Research
Overview of Recent Studies on Airway Clearance Techniques
Airway clearance techniques (ACTs) have been a focal point in managing bronchiectasis because of their role in improving mucus clearance, reducing exacerbations, and enhancing quality of life. Recent research continues to evaluate the efficacy of various ACTs, offering valuable insights into their benefits and limitations.
Key Findings from Research Articles
Study 1: Analysis From the United States Bronchiectasis and Non-TB Mycobacteria Research Registry
This study investigated the differences in clinical outcomes among bronchiectasis patients who used ACTs versus those who did not. The research focused on adult patients with bronchiectasis and a productive cough, using data from the United States Bronchiectasis and NTM Research Registry.
- Key Findings:
- Increased Use in Severe Cases: ACTs were more commonly used by patients with a history of exacerbations, hospitalizations for pulmonary illness, or infections with Pseudomonas aeruginosa.
- Exacerbation Frequency: Patients using ACTs continuously had higher odds of experiencing exacerbations at follow-up compared to those who did not use ACTs. This suggests that ACTs are often prescribed for more severely ill patients who are prone to frequent exacerbations.
- Pulmonary Function: No significant change in pulmonary function was observed at the one-year follow-up for patients using ACTs, indicating that while ACTs may help manage symptoms, they do not necessarily improve lung function over time.
- Implications for Clinical Practice:
- Targeted Use: The study highlights the importance of targeting ACTs for patients with severe symptoms and a history of frequent exacerbations.
- Monitoring and Adjustment: Continuous monitoring and adjustment of ACTs might be necessary to optimize patient outcomes and manage severe cases effectively.
Study 2: Airway Clearance Techniques: The Right Choice for the Right Patient
This study reviewed various ACTs and their effectiveness in managing bronchial secretions across different medical conditions, including bronchiectasis. The review emphasized the need to choose the appropriate ACT based on individual patient needs and preferences.
- Key Findings:
- Variety of Techniques: The study discussed multiple techniques, including postural drainage, manual techniques (percussion and vibration), PEP therapy, mechanical devices (like cough assist and HFCWO), and combined ACTs.
- Patient-Centered Approach: It highlighted the importance of considering patient preferences, adherence, and specific clinical conditions when selecting an ACT.
- Clinical Effectiveness: While no single ACT was found to be superior across all scenarios, combining different techniques based on the patient's needs showed potential benefits.
- Implications for Clinical Practice:
- Personalized Therapy: Clinicians should adopt a personalized approach when prescribing ACTs, taking into account patient preferences, lifestyle, and specific clinical conditions.
- Combination Therapy: Utilizing a combination of ACTs tailored to the patient's condition may enhance mucus clearance and improve clinical outcomes.
Ultimately, your doctor can give you individualized guidance based on your specific needs as a bronchiectasis patient. While some airway clearance devices or techniques can be purchased and performed without a prescription, other options like a vest require a written order.
Key Takeaways
Living with bronchiectasis can be tough due to the constant battle with mucus build-up and frequent lung infections. Regular airway clearance is a key part of managing this condition, making a significant difference in preventing complications and improving daily life.
Understanding the various airway clearance techniques for bronchiectasis available—from simple breathing exercises to high-tech devices—can empower you to choose the most effective methods for yourself or a loved one. Recent research shows the importance of tailoring these techniques to each individual, ensuring they are as effective and manageable as possible.
TruNeb™ is dedicated to helping people with bronchiectasis, COPD, and other respiratory diseases effectively manage their conditions through innovative nebulizers, saline, and devices.
Shop Now→







